* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Notes to Heart 2
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Aortic stenosis wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
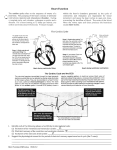
Dr. Chris Doumen Lecture 1 2402 : Anatomy/Physiology The Heart The El ectroCardiogram The impulses generated by the heart generate electrical currents that can be detected TextBook Readings at the surface of the heart. An Electrocardiogram records electrical changes that occur ♦ Pages 697 through 720. ♦ Make use of the figures in your textbook ; a picture is worth a thousand words ! ♦ Work the Problems and Questions at the end of the Chapter Collin County Community College District at each heartbeat. It is obtained by placing electrodes on the arm, legs and six positions on the chest. From an ECG one can determine for example • if conduction pathways are normal • if the heart is enlarged • if a certain region of the heart is damaged The EKG consists of 3 waves called deflection waves • P-wave • represents atrial depolarization • spreads from the SA node throughout the atria • QRS-wave • onset of ventricular depolarization • ventricles contract shortly after QRS wave begins • T-wave • represents ventricular repolarization • occurs juts before they start relaxing • smaller than QRS. wave because repolarization occurs more slowly than depolarization • Repolarization of Atria is not seen; buried in QRS wave 2402 : Anatomy/Physiology Page 2 of 8 Clinical manifestations : • • • Large P wave : enlargement of the atria (mitral restenosis, blood backs up) Large Q wave : may indicate myocardial infarction large R wave : ventricular enlargement Bradycardia : slower than normal heart rate (< 50bpm) Tachycardia : faster than normal heart rate (> 100 bpm) • • Heart block refers to impeded impulses at the AV node ( poor conduction to ventricles, no ventricular contraction) • First Degree : a long P-QR interval, long conduction from SA node to AV node, possible scar tissue • Second degree: AV node fails to pass impulses every 2 or 3 beats ( 2,3 P waves /QRS wave) (missed beats) • Third degree block : no impulse from the nodes reaches the ventricles. The atria and ventricles beat independently with their own rhythm. Fibrillation occurs when the heart muscle mass starts beating independently at different positions of the heart. • atrial fibrillation ( not immediate dangererous) • ventricular fibrillation ( ventricles don’t pump anymore) Complete heart block ( 3rd degree block) 2401 : Anatomy/Physiology Page 3 of 8 The Cardiac C ycle (Fig. 20-17) In a normal cycle, two events take place one after another • the two atria contract while the ventricles relax • then the two ventricles contract while the atria relax The phase of contraction = SYSTOLE The relaxation phase = DIASTOLE a. The Relaxation period • • starts with the T-wave in the EKG it is the period when both ventricles and atria are relaxed • • results in a closure of the SL valves ( backflow of aortic blood against the valves) also results in a pressure drop within the ventricles • pressure drop within the atria causes blood to rush into the atria from vena cava and pulmonary veins • this period is know as the isovolumic relaxation period b. Ventricular filling phase • • • • • starts when pressure inside ventricles drops even more and allows opening of the AV valves (pressure slightly starts increasing) it is followed by firing of the SA-node = atrial systole blood rushes into the ventricles and volume increases until it shuts the AV-valves note that most of the blood entering the ventricles is due to the relaxation of the ventricles; only ~ 20% enters due to atrial systole The end of ventricular filling is when the ventricles are still relaxed • • c. Volume at that point = END DIASTOLIC VOLUME (EDV) Pressure at that point = END DIASTOLIC PRESSURE Ventricular systole • starts when the impulse from the SA-node reaches the AV-node (start of QRS) • ventricles contract and atria relax • since SL-valve is closed, pressure builds up till it is higher than aortic pressure (blood pressure) • The volume at the end of systole = END-SYSTOLIC VOLUME (ESV) • Pressure at the end of systole = END-SYSTOLIC PRESSURE (=peak pressure) • At this point the SL open and we have ventricular ejection • the end point is reached when blood has been ejected out of the ventricles and the ventricles start to relax (back to the top) 2401 : Anatomy/Physiology Page 4 of 8 The he art be at s about 75 time s p er mi n or 0 .8 sec pe r be at. The average time the atri a and ve nt ricle are i n s ys t ole- di as t ol e is the n : Time Atria Ventricles SL-valves AV-valves 0.4 sec 0.1 sec 0.3 sec Diastole Systole Diastole Diastole Diastole Systole closed closed open open open closed Stroke Volume Both ventricles eject the same amount of blood volume per beat = st rok e vol ume (SV) Strok e V ol ume (SV ) = EDV - ES V ( roughl y equ al t o 135 ml - 65 ml = 70 ml pe r h eart be at ) Since the left ventricle has to overcome a higher pressure when ejecting blood, the walls are more massive. Heart Sound s • During each heart cycle, 4 heart sounds are produced. • Only 2 are loud enough to hear without instrumentation; called the "LUBB-DUPP" sounds • • Lubb = closure of the AV valves (after ventricular systole) • Dupp = closure of the SL valves (beginning of ventricular diastole) The noise is associated with blood turbulence and thus any abnormal noise indicates some kind of blood turbulence problems 2401 : Anatomy/Physiology Page 5 of 8 Heart murmurs for example indicate valve disorders. Possible valve disorders and associated terminology • mitral stenosis = narrowing of the mitral valve • mitral insufficiency = back flow from left ventricle into the left atrium (bad valve or chordae tentidinae) • aortic stenosis = narrowing of the aortic SL valve • aortic insufficiency = backflow from aorta into left ventricle • mitral valve prolapse = mitral valve pushed back into the atrium Cardiac Output Cardiac Output (CO) is the amount of blood ejected from the left ventricle into the aorta each minute Cardi ac Ou tp ut (CO) = H eart rate x St roke V olum e ( roughl y equ al t o 70 be at s/min x 70 ml/ be at = 5,2 50 ml/ min So in a resting individual the cardiac output comes close to being equal to the total blood volume. When demand for oxygen and nutrients increases in the body, such as during exercise, the CO will need adjustment in order to cope with these demands. How does the heart comply ? By adjusting the two elements that make up CO e.g. Stroke Volume and Heart Rate ! Regul ation of Cardiac Output Regulation of Stroke Volume Remember that stroke volume = EDV - ESV . A. Preload • Cardiac muscle, just like skeletal muscle , exhibits a length-tension relationship • However, resting cardiac muscle are shorter than their optimal length for developing maximal tension (in contrast to skeletal muscle) • Therefore, increasing their length (stretching) prior to contraction will increase the force of contraction • exercise allows more venous return due to the squeezing action of skeletal muscle; this increases EDV and thus SV Note that preload ensures that both left and right ventricle keep up with the amount of blood pumped. Any increase in CO by the left ventricle will result in more venous return to the right ventricle which then will pump equivalent amount back to the left ventricle Page 6 of 8 • 2401 : Anatomy/Physiology Thus • increased venous return or exercise, allows more blood to return to the heart • this will increase the stretch on the ventricular muscle cells and increase ventricular filing • increased ventricular filling prior to contraction = increased EDV • the greater the EDV, the more forceful the contraction but also the higher the stroke volume • This preload effect is also know as the F rank-S t arl ing L aw • It is influenced by the heartbeat and exercise • low heart beat allows more time for ventricular filling and thus increases the preload, and thus CO • however at a heart beat of 160 or more , less time is available to fill the ventricles before it is ejected and this will actually reduce SV • exercise allows more venous return due to the squeezing action of skeletal muscle; this increases EDV and thus SV Note that preload ensures that both left and right ventricle keep up with the amount of blood pumped. Any increase in CO by the left ventricle will result in more venous return to the right ventricle which then will pump equivalent amount back to the left ventricle This diagram shows the relationship between Increased EDV and Stroke Volume ( The Frank Starling Effect). Curves A and B illustrate the rise in cardiac output with increases in ventricular enddiastolic volume (pre-load) in the normal heart. Note that with an increase in contractility there is a greater cardiac output for the same ventricular enddiastolic volume. In the diseased heart (C and D), cardiac output is leass and falls if ventricular enddiastolic volume rises to high levels, as in heart failure or overload. B. Contractility • This is the strength of contraction at any given preload • Substances that can increase contractility at any given preload are called positive inotropic agents • They usually promote extra Calcium inflow ( thus increasing the number of cross bridge cycling) • The result is thus a more forceful ejection of blood, lowering ESV and in turn increasing SV • Example • digitalis • sympathetic stimulation (increases calcium influx at each heart beat into the cell) 2401 : Anatomy/Physiology Page 7 of 8 C. Afterload • Refers to the pressure that must be overcome to eject the blood from the ventricles • The pressure in the pulmonary trunk is not a problem (only 10 mm Hg) • The pressure in the aorta (blood pressure)is a major determinant of stroke volume • The higher the blood pressure, the more blood remains in the left ventricle (higher ESV), the lower the SV A series of curves illustrates the effects of increasing afterload on systemic vascular resistance. As afterload increases, the patient moves to a lower curve, with a lower stroke volume for the same ventricular end-diastolic volume (preload). Regulation of Heart rate The SA-node initiates contraction at a certain pace. Several factors contribute to the regulation of heart-rate A. Via Autonomic Nervous system • Sympathetic branch • connects with the SA, AV node and most of the myocardium • releases norepinephrine that stimulates Ca2+ entry into SA node cells and the contractile cells ( via beta 1 receptors, cAMP and PK-A production and opening of Calcium channels) • This causes threshold to be reached quicker in pacemaker cells --- increased HR • In the myocardial cells this increases contractility • Since ESV is reduced, SV does not decline as it would if only HR were 2401 : Anatomy/Physiology • Page 8 of 8 Parasympathetic regulation • reaches heart via the vagus nerve • Innervates SA, AV node and opposes sympathetic effects • Releases acetylcholine which increases K permeability in pacemaker cells and thus slows the time before they reach threshold --- reduces HR The heart exhibits vagal tone as it is dominated by the vagus nerve. Cutting the vagal nerve immediately increases the heart rate by about 25 beats / min . B. Via Blood Circulating Chemicals • • Hormones • Epinephrine release by the adrenal medulla (same effect as norepinephrine) • Thyroxine released by thyroid gland increases HR Ions • Calcium : reduced levels (hypocalcemia) depress the heart • Sodium : too much (hypernatremia) inhibits transport of calcium into the cells • Potassium: too much (hyperkalemia) interferes with depolarization (negative inotropic agent)