* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download March 2003: Volume 31, Number 2 (PDF: 102KB/8 pages)
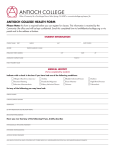
Survey
Document related concepts
Bioterrorism wikipedia , lookup
Tuberculosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Onchocerciasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Anthrax vaccine adsorbed wikipedia , lookup
Meningococcal disease wikipedia , lookup
Whooping cough wikipedia , lookup
Transcript
MINNESOTA DEPARTMENT OF HEALTH D ISEASE C ONTROL N EWSLETTER Volume 31, Number 2 (pages 13-20) March/April 2003 Recommended Childhood and Adult Immunization Schedules - Minnesota, 2003 In 2003, for the first time in several years, there are no significant changes or modifications to the Minnesota Department of Health (MDH)’s recom mended schedule for childhood immunizations. The schedule, now called the Recommended Childhood and Adolescent Immunization Schedule, includes several minor enhance ments to make it easier to use and understand (pages 14-15). The addition of “Adolescents” in the title reflects the entire population (birth through 18 years of age) covered by the schedule. A companion piece to the childhood and adolescent immuni zation schedule, the Recommended Adult Immunization Schedule, provides comparable guidelines for persons 19 years of age or older (pages 16-17). This schedule was modified slightly in the fall of 2002 following the withdrawal of the Lyme disease vaccine. less frequently and is updated as needed. MDH has attempted to consolidate and summarize the recommendations of the various advisory bodies as clearly and succinctly as possible in the Minnesota immunization schedules. Providers also should consult the national recommendations and subsequently published supplemental recommenda tions as needed. In particular, please be aware of the following points: • The charts and guidelines in each schedule must be read together. • Refer to the complete ACIP statement for specific circum stances beyond the guidance offered in the MDH schedules. Other resources include the following: The childhood and adult immunization schedules reflect recommendations of national advisory bodies such as the Advisory Committee on Immunization Practices (ACIP), the American Academy of Pediatrics (AAP), the American Academy of Family Physi cians, and the American College of Physicians. The MDH Immunization Practices Task Force reviews the schedules and suggests modifications, which are incorporated as appropriate for Minnesota’s populations. The childhood schedule is issued annually to incorporate changes as new vac cines are licensed, products change, and recommendations for their use are modified. The adult schedule changes • American Academy of Pediatrics. Pickering LK, ed. 2000 Red Book: Report of the Committee on Infectious Diseases. 25th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2000. • The Minnesota Immunization Hotline (M-F, 9:00 A.M. – 12:00 P.M. and 1:00 P.M. – 3:00 P.M.), at 612-676-5100 or 1-800-6573970. • The Centers for Disease Control and Prevention (CDC) hotline at 1-800-232-0233. and, • Vaccine manufacturers’ help-lines and package inserts. Both the childhood and adult immuniza tion schedules are available on the MDH website at http:// www.health.state.mn.us/immunize; scroll down to “Schedules and Recom mendations.” Color copies of both schedules are being printed, and MDH will distribute these to all clinics, hospitals, public health agencies, and health plans when they become available in mid- to late April. Additional copies can be ordered by calling the Minnesota Immunization Hotline at 612676-5100 or 1-800-657-3970, or by e-mailing MDH at [email protected]. • Department of Health and Human Services, Centers for Disease Control and Prevention. Atkinson W, Wolfe C, eds. Epidemiology and Prevention of Vaccine-Preventable Diseases. 7th ed. Washington, DC: Public Health Foundation; 2002. Inside: Newly Approved Blood Test for Diagnosing Latent Tuberculosis Infection: Guidelines for Use of QuantiFERON®-TB .................. 18 DCN Readership Alert and Survey .............................. 19 Recommended Childhood and Adolescent Immunization Schedule - Minnesota, 2003 Chart 12345678901234567890123456789012123 must be used with guidelines below 12345678901234567890123456789012123 12345678901234567890123456789012123 Catch-up vaccination 12345678901234567890123456789012123 Range of recommended ages ? Age? Birth Vaccine HBV - 1 Hepatitis B1 1 mo 2 mos 4 mos 6 mos DTaP DTaP DTaP Hib Hib Hib3 IPV IPV DTaP2 Varicella PCV PCV 4-6 yrs PCV 11-12 yrs 13 -18 yrs 1234567890123456789012345678 1234567890123456789012345678 1234567890123456789012345678 HBV1 series 12345678 12345678 12345678 2 DTaP Td 12345678 Hib3 MMR - 1 6 Pneumococcal7 24 mos IPV IPV Measles, Mumps, Rubella5 Varicella 18 mos HBV - 3 Haemophilus influenzae type b3 Polio4 15 mos only if mother is HBsAg(-) HBV - 2 Diphtheria, Tetanus, Pertussis2 12 mos Preadolescent assessment PCV 12345678901234 12345678901234 MMR-25 12345678901234 MMR-25 1234567890123456789012345678 1234567890123456789012345678 1234567890123456789012345678 Varicella 12345678901 12345678901 12345678901 PCV 12345678901 PPV Vaccines below line are for selected populations Hepatitis A8 Hepatitis A series Influenza9 Influenza (yearly) Guidelines: This schedule indicates the recommended ages for routine administration of currently licensed childhood vaccines, as of January 1, 2003, for children through age 18 years. Any dose not given at the recommended age should be given at any subsequent visit, when indicated and feasible. 123456 123456 : Indicates age groups that warrant special effort to administer those vaccines not previously given. Additional vaccines may be licensed and recommended during the year. Licensed combination vaccines may be used whenever any components of the combination are indicated and the vaccine’s other components are not contraindicated. Consult the manufacturers’ package inserts for detailed recommendations. 1. Hepatitis B vaccine (HBV): All infants should receive HBV-1 soon after birth and before hospital discharge; the 1st dose also may be given by age 2 mos if the infant’s mother is HBsAg-negative. Give HBV-2 >4 wks after HBV-1 and HBV-3 >8 wks after HBV-2 (provided it is >4 mos since HBV-1 and infant is no younger than 6 mos of age). Infants born to HBsAg-positive mothers should receive 0.5 mL hepatitis B immune globulin (HBIG) within 12 hrs of birth and HBV-1 at a separate site. HBV 2 is recommended at 1-2 mos of age and HBV-3 at 6 mos of age. Infants born to mothers whose HBsAg status is unknown should receive HBV-1 within 12 hrs of birth. Maternal blood should be drawn at the time of delivery to determine the mother’s HBsAg status. If the HBsAg test is positive, the infant should receive 0.5 mL of HBIG as soon as possible (no later than 1 wk of age). HBV-2 is recommended at 1 mo of age and HBV-3 at 6 mos of age. Children and adolescents who have not previously received all 3 doses of HBV should complete the series, with minimum intervals of 4 wks between HBV1 and HBV-2, and 8 wks between HBV-2 and HBV-3 (and 4 mos between HBV-1 and HBV-3). Refer to package insert for alternate 2-dose schedules for adolescents. 2. Diphtheria, tetanus, and acellular pertussis (DTaP): DTaP-4 may be given as early as 12 mos of age, if at least 6 mos have passed since DTaP-3 and the child is considered unlikely to return at 15-18 mos of age. Td (tetanus and diphtheria toxoids, adsorbed, for adult use) is recommended at 11-12 yrs of age, if at least 5 yrs have passed since the last dose of tetanus and diphtheria-containing vaccine. Subsequent routine Td boosters are recommended every 10 yrs. 3. Haemophilus influenzae type b (Hib): Three Hib conjugate vaccines are licensed for infants. If PRP-OMP (PedvaxHIB or Comvax) is given at 2 and 4 mos of age, a dose at 6 mos is not required. Do not use DTaP/Hib combination products for the first 3 doses (primary series). Use any Hib conjugate vaccine as a booster. 4. Polio: Inactivated polio vaccine (IPV) is the only vaccine available in the United States. 5. Measles, mumps, rubella (MMR): MMR-2 is recommended at 4-6 yrs but may be given during any visit, provided >4 wks have elapsed since MMR-1 and both doses are given at >12 mos of age. 6. Varicella (chickenpox): Varicella vaccine is recommended at any visit at or after age 12 mos for susceptible children - i.e., those who lack a reliable history of chickenpox. Susceptible persons age >13 yrs should receive 2 doses given at least 4 wks apart. 7. Pneumococcal: The heptavalent pneumococcal conjugate vaccine (PCV) is recommended for all children age 2-23 mos and for certain children age 24-59 mos. Pneumococcal polysaccharide vaccine (PPV) is recommended, in addition to PCV, for certain high-risk groups. See MMWR 2000;49(RR-9);1-35. 8. Hepatitis A: Give hepatitis A vaccine to children and adolescents who are at increased risk of infection, as defined by ACIP*, and consider it for all others >2 yrs of age who wish to obtain immunity. Give a booster >6 mos after the initial dose. 9. Influenza: Influenza vaccine is recommended annually for children age >6 mos with certain risk factors (including, but not limited to asthma, cardiac disease, sickle cell disease, HIV, and diabetes) [see MMWR 2002;51(RR-3);1-31]. It can also be administered to all others wishing to obtain immunity. In addition, healthy children age 6-23 mos are encouraged to receive influenza vaccine, if feasible, because they are at substantially increased risk for influenza-related hospitalizations. Children age <12 yrs should receive a dosage appropriate for their age (0.25 mL, if age 6-35 mos or 0.5 mL, if age >3 yrs). Children aged <8 yrs who are receiving influenza vaccine for the first time should receive 2 doses separated by at least 4 wks. Based on recommendations of the Advisory Committee on Immunization Practices (ACIP), the American Academy of Pediatrics (AAP), and the American Academy of Family Physicians (AAFP) and endorsed by the Immunization Practices Task Force of the Minnesota Department of Health (MDH). *Questions or need current ACIP recommendations? Call the Minnesota Immunization Hotline at 612-676-5100 or (toll-free) 1-800-657-3970. Web site: www.health.state.mn.us/immunize Minnesota Department of Health, March 2003, IC# 141-0188 14 For Children and Adolescents Who Start Late or Who Are >1 Month Behind For any vaccine given in a series, it is not necessary to start over. Refer to the tables below for the recommended “catch-up” schedule and minimum intervals between doses. Determine the number of previous doses of each vaccine received, find that number in the first column, and read across to the appropriate column for the next dose(s) and minimum interval(s). Table 1. Catch-up schedule for children 4 months through 6 years of age - must be used with guidelines below. Doses to be given and minimum intervals from previous dose Number of previous doses First dose DTaP IPV HBV MMR2 Varicella3 Hib1 PCV1,4 None Third dose Second dose DTaP: IPV: HBV: MMR2: Hib: One 4 weeks 4 weeks 4 weeks 4 weeks 4 weeks - if 1st dose given at <12 mos of age 8 weeks (as final dose) - if 1st dose given at 12-14 mos of age No further doses needed - if 1st dose given at >15 mos of age PCV4: 4 weeks - if 1st dose given at <12 mos of age and child is <24 mos of age 8 weeks (as final dose) - if 1st dose given at >12 mos of age or child is now 24-59 mos of age Two DTaP: 4 weeks IPV: 4 weeks HBV: 8 weeks and 16 weeks after first dose Hib: 4 weeks6 - if current age <12 mos 8 weeks (as final dose)6 - if current age >12 mos and 2nd dose given at age <15 mos No further doses needed if previous dose given at age >15 mos PCV4: 4 weeks - if child is <12 mos of age 8 weeks (as final dose) - if child is >12 mos of age Fourth dose DTaP: 6 months IPV5: 4 weeks Hib6: Fifth dose DTaP7: 6 months 8 weeks (as final dose) - this dose necessary only for children age 12 mos - 5 yrs who received 3 doses before age 12 mos PCV4: 8 weeks (as final dose) - if 3rd dose given at <12 mos of age Three Four Table 2. Catch-up schedule for children 7 through 18 years of age - must be used with guidelines below. Doses to be given and minimum intervals from previous dose Number of previous doses None First dose Td IPV Second dose Td: IPV : 4 weeks HBV HBV: 4 weeks 5 MMR: Varicella 3 Td: 4 weeks 5 MMR Third dose 6 months IPV5: 4 weeks HBV: 8 weeks and 4 months after 1st dose 4 weeks Varicella : 4 weeks 3 One Two Three Booster dose Td: If 7-10 yrs of age: • 6 mos, if 1st dose given at <1 yr of age • 5 yrs (but no sooner than age 11 yrs), if 1st dose given at >1 yr of age If 11-18 yrs of age: • 5 yrs, if 3rd dose given at <7 yrs of age • 10 years, if 3rd dose given at >7 yrs of age IPV5 Guidelines for Catch-up 1. Hib and/or PCV: Vaccine generally is not recommended for children >5 years of age. 2. MMR: Do not administer MMR vaccine before 12 months of age. Administer 2nd dose of MMR routinely at 4-6 years of age or earlier, if desired. 3. Varicella: Do not administer varicella vaccine before 12 months of age. Give 2-dose series to all susceptible adolescents >13 years of age. 4. PCV: Use Table 1 to determine catch-up scheduling of children at high risk of infection, as well as healthy children <60 months of age who have begun, but not completed, a schedule of PCV. Unvaccinated children 24-59 months of age and at moderate risk of infection need only 1 dose [see MMWR 2000;49(RR-9);135]. Consider giving 1 dose to unvaccinated children 36-59 months of age who are not at moderate or high risk of infection, yet wish to obtain immunity. 5. Polio: The 4th dose is not necessary in an all-IPV or all-OPV schedule, if the 3rd dose was given after the 4th birthday. If both OPV and IPV were given as part of the series, a total of 4 doses should be given, regardless of the child’s current age. Vaccine generally is not recommended for persons >18 years of age. 6. Hib: If PRP-OMP (PedvaxHIB or Comvax) was given for the first 2 doses, no more than 3 doses are needed, with the final dose given at 12-15 months of age and at least 8 weeks after the previous dose. If a 3rd dose of HbOC (HibTiter) or PRP-T (ActHib) is given at >12 months of age, a 4th dose is not needed. 7. DTaP: The 5th dose is not necessary if the 4th dose was given after the 4th birthday. Reporting Adverse Reactions Disease Reporting Report adverse reactions to vaccines through the federal Vaccine Adverse Event Reporting System. For information on reporting reactions following vaccines administered by private clinics, call the 24hour national toll-free information line at 1-800-822-7967. Report reactions to vaccine administered in public clinics to the Minnesota Department of Health at 612-676-5414 or (toll-free) 1-877-676-5414. Report suspected cases of vaccine-preventable diseases to the local health department or to the Minnesota Department of Health, P.O. Box 9441, Minneapolis, MN 55440, 612-676-5414 or (toll-free) 1-877-6765414. 15 Recommended Adult Immunization Schedule **Chart must be used with guidelines below** Age ? ? z Vaccine 45 - 49 years 19 - 44 years Tetanus, Diphtheria1 50 - 64 years 65+ years Booster every 10 years Measles, Mumps, Rubella2 1-2 doses, if born after 1956 Vaccines below line are for selected populations Influenza3 Pneumococcal4 Hepatitis A5 Annually, if at risk or wishing to obtain immunity 1-2 doses for those with risk factors Varicella8 1-2 doses 2 doses for those at increased risk of HAV infection and others wishing to obtain immunity 3 doses for those with risk factors Hepatitis B6 Meningococcal7 Annually 1 or more doses for those with risk factors 2-dose series for selected groups 1. Tetanus and Diphtheria (Td): All previously unvaccinated adults should complete a 3-dose primary series of diphtheria and tetanus toxoids. All adults for whom 10 years have elapsed since their primary series or since their last booster dose should receive a Td booster. 2. Measles, Mumps, Rubella: Adults born before 1957 are considered naturally immune. Adults born in 1957 or later should receive 1 dose of MMR vaccine. Some adults, such as college students, those working in health care facilities, and international travelers may need 2 doses given not less than 4 weeks apart. 3. Influenza: Administer influenza vaccine annually to all adults >50 years of age; residents of nursing homes and other long-term care facilities; younger adults with chronic cardiopulmonary disorders, chronic metabolic diseases (including diabetes), renal dysfunction, hemoglobinopathies, or immunosuppression, as well as to the household members, caregivers, and health care workers of the above. Other adults who wish to reduce their likelihood of becoming ill with influenza also may be vaccinated. 4. Pneumococcal: Give pneumococcal polysaccharide vaccine (PPV) to all adults >65 years of age and those <65 years of age with chronic cardiovascular disease, chronic pulmonary disease, diabetes mellitus, alcoholism, cirrhosis, CSF leaks, functional or anatomic asplenia, HIV infection, leukemia, lymphoma, Hodgkins disease, multiple myeloma, generalized malignancy, chronic renal failure, nephrotic syndrome, or if receiving immunosuppressive chemotherapy. Routine revaccination of immunocompetent persons previously vaccinated with 23-valent PPV is not recommended; however, revaccination is recommended if a person was vaccinated >5 years previously and either (1) was <65 years of age when first vaccinated and is now >65 years of age or (2) is at highest risk for serious pneumococcal infection, as defined by ACIP, or (3) is likely to have a rapid decline in pneumococcal antibody levels. 5. Hepatitis A: Give 2 doses of hepatitis A vaccine, 6-12 mos apart, to persons who are at increased risk for infection with hepatitis A virus (HAV), as well as to food-handlers and others wishing to obtain immunity. Populations at increased risk include: persons traveling to or working in countries with high rates of HAV, men who have sex with men, persons who use street drugs, persons with chronic liver disease, persons who work with HAV-infected primates or with HAV in a research setting, and persons with clotting factor disorders. 6. Hepatitis B: Adults at risk for HBV infection include: persons who may be exposed to blood or blood products in their work, clients and staff of institutions for the developmentally disabled, hemodialysis patients, recipients of factor VIII or IX concentrates, household or sexual contacts of persons identified as HBsAg-positive, persons who plan to travel or live in parts of the world where HBV infection is common, injecting drug users, sexually active homosexual or bisexual males, sexually active heterosexual persons with multiple partners or recent episode of an STD, inmates of long-term correctional facilities, and persons of Pacific Islander ethnicity or first-generation immigrants/refugees from countries where HBV infection is of high/intermediate endemicity. Give a 3-dose series on a schedule of 0, 1, and 6 months. 7. Meningococcal: Give quadrivalent polysaccharide meningococcal vaccine (A/C/Y/W-135) to adults with terminal complement component deficiencies, those with anatomic or functional asplenia, and travelers to countries where meningococcal disease is epidemic (e.g., the “meningitis belt” of sub-Saharan Africa) or to Mecca, Saudi Arabia. Consider revaccination within 3-5 years for persons who continue to be at high risk of infection (e.g., persons remaining in areas where disease is epidemic). Providers may consider vaccination of college freshman who live in dormitories to reduce their slightly increased risk of disease. 8. Varicella: Administer varicella vaccine to susceptible persons who will have close contact with persons at high risk for serious complications (e.g., health care workers and family contacts of immunocompromised persons). Consider vaccinating susceptible persons who are at high risk of exposure, such as those with occupational risk (e.g., teachers of young children, day care workers, and residents and staff in institutional settings), college students, inmates and staff of correctional institutions, military personnel, non-pregnant women of childbearing age, and international travelers. Vaccination for adults consists of 2 doses given 4-8 weeks apart. Based on recommendations of the Advisory Committee on Immunization Practices (ACIP) and the American College of Physicians and endorsed by the Immunization Practices Task Force of the Minnesota Department of Health (MDH). *Questions or need current ACIP recommendations? Call the Minnesota Immunization Hotline at 612-676-5100 or (toll-free) 1-800- 657-3970. Web site: www.health.state.mn.us/immunize Minnesota Department of Health, 2002, IC# 141-0316 16 Catch-Up Schedule and Minimum Intervals for Adults For any vaccine given in a series, it is not necesary to start over. Refer to the table below for the recommended “catch-up” schedule and minimum intervals between doses. Determine the number of previous doses of each vaccine received, find that number in the first column, and read across to the appropriate column for the next dose(s) and minimum interval(s). Doses to be given and minimum intervals from previous dose for adults >19 years of age Number of previous doses None First dose Second dose Td Td: 4 weeks after 1st dose MMR MMR: 4 weeks after 1st dose Pneumococcal (PPV) PPV: 5 years after 1st dose for those who received 1st dose at <65 years of age or who are at highest risk for pneumococcal infection Hepatitis A (HAV) HAV: 6 months after 1st dose Hepatitis B (HBV) HBV: 4 weeks after 1st dose Varicella Varicella: 4 weeks after 1st dose Third dose Booster dose Td: 6 months after 2nd dose Td: 10 years after completion of the primary series or since last booster dose HBV: 8 weeks after 2nd dose and 4 months after 1st dose One Two Three Guidelines for Patients with an Incomplete or Non-existent Vaccine History • For adult patients who are refugees or immigrants, provide vac cinations as you would for any other adult patient. Translations of foreign vaccine terms and vaccine products can be found in the Minnesota Department of Health (MDH) Provider’s Guide to Im munizations or on the MDH web site: www.health.state.mn.us/immunize. • Patients 18 years of age or older, including foreign-born adults, do not need polio vaccination, unless they are traveling to a coun try where wild poliovirus still exists. (See MDH Recommended Immunizations for International Travel.) • A Mantoux tuberculin skin test can be administered simulta neously with any live or inactivated vaccine. If the patient already received MMR, the Mantoux test must be delayed for at least 4 weeks after the MMR; if the Mantoux was applied first, MMR or any other vaccine can be given at any time. • Count only vaccinations that are well documented (i.e., includ ing month, year, and, preferably, day of vaccination). If no docu mentation exists, assume the patient is unvaccinated. It is always better to vaccinate when in doubt, rather than miss an opportunity to provide protection. • This catch-up schedule must be used together with the guide lines on page 16. • Use all opportunities to assess the vaccination status of adult patients. At age 50 years, give a Td (unless a dose has been given in the previous 10 years) and evaluate for risk factors for pneumococcal and other vaccine-preventable diseases. • If patient has started a series (e.g., HBV) but not completed it, continue where he/she left off. Never restart a series of any vaccine (exception: oral typhoid vaccine, in some situations). • MMR and varicella vaccines can be given at the same visit. If not given simultaneously, they must be separated by at least 4 weeks. • Patients do not need measles, mumps, and/or rubella vaccine if they were born before 1957, have lab evidence of immunity, or (for measles/mumps only) have a physician-diagnosed disease history. Consider vaccinating women born before 1957 who may become pregnant and do not have lab evidence of immunity or physician-diagnosed disease. Reporting Adverse Reactions Disease Reporting Report adverse reactions to vaccines through the federal Vaccine Adverse Event Reporting System. For information on reporting reactions following vaccines administered by private clinics, call the 24-hour national (toll-free) information line at 1-800-822-7967. Report reactions to vaccines administered in public clinics to the Minnesota Department of Health at 612-676-5414 or (toll-free) 1-877-676-5414. Report suspected cases of vaccine-preventable diseases to the local health department or to the Minnesota Department of Health, P.O. Box 9441, Minneapolis, Minnesota 55440, 612-676-5414 or (toll-free) 1-877-6765414. 17 Newly Approved Blood Test for Diagnosing Latent Tuberculosis Infection: Guidelines for Use of QuantiFERON®-TB Until recently, the only test available to diagnose latent tuberculosis infection (LTBI) was the tuberculin skin test (TST). In late 2001, the Food and Drug ® Administration approved QuantiFERON -TB (QFT), a new diagnostic test for LTBI. Due to limited clinical experience regarding the use of QFT and the absence of a “gold standard” to confirm LTBI, data to assess the accuracy and beneficial applications of QFT currently are limited. In January 2003, the Centers for Disease Control and Prevention (CDC) issued interim guidelines for the use of QFT.1 These guidelines are intended to provide guidance on the use and interpretation of QFT for public health professionals, health care providers, and laboratorians involved in TB prevention and control activities in the United States. Those recommendations are summarized here. and limited clinical and laboratory experience with the test. Also, due to insufficient data on the predictive accuracy of QFT in some populations, the CDC guidelines do not support the use of QFT in certain situations in which the TST commonly is employed (e.g., TB contact investigations or evaluation of patients with suspected TB disease). CDC also recommends confirming a positive QFT result with a TST before starting treatment for LTBI, particularly in certain low-risk patients. QFT, manufactured by Cellestis Limited of Australia, measures immune response to infection with Mycobacterium tuberculosis (Mtb) by quantifying the release of interferon-gamma in whole blood in response to stimulation by purified protein derivative. As with the TST, where cutoffs of 5, 10, or 15 millimeters of induration are used to identify a positive TST result for high-, moderate- and low-risk persons, interpretation of QFT results also is stratified by the patient’s estimated risk for LTBI. QFT can aid in detecting LTBI among certain populations, including recent immigrants from areas of the world where TB is common, injection drug users, residents and employees of correctional facilities, and health care workers. • initial and serial testing of persons Advantages of QFT include the facts that it is less subject to reader bias and error than the TST; it is accomplished in a single patient visit; it does not “boost” immune response in persons with remote LTBI; and, it differentiates between infection with Mtb and Mycobacterium avium, a common nontuberculous mycobacteria. Limita tions of QFT include the need to draw blood, the need to process the blood sample within 12 hours after collection, CDC recommends that QFT can be considered to screen for LTBI in the following circumstances: • initial and serial testing of certain persons at an increased risk for LTBI (e.g., recent immigrants, injection drug users, residents and employ ees of correctional facilities); who are, by history, at low risk for LTBI but whose future activity might place them at increased risk for exposure, and others eligible for LTBI surveillance programs (e.g., health care workers and military personnel); and, • testing of persons for whom screen ing may be required but who are not considered to have an increased risk for LTBI (e.g., entrance require ments for certain schools and workplaces). Due to a lack of sufficient data on which to base recommendations, CDC currently does NOT recommended QFT for: • evaluation of persons with sus pected TB disease; • assessment of contacts of persons • detection of LTBI after a suspected exposure (e.g., laboratory spill of Mtb) among persons who receive serial testing for LTBI; • confirmation of postitive TST results (because injection of tuberculin in tuberculin skin testing might affect subsequent QFT results); or, • diagnosis of M. avium complex disease. Consistent with current guidelines for tuberculin skin testing, CDC discour ages screening for LTBI among populations at low risk for TB, regard less of whether screening is performed using the TST or QFT. Also, screening for LTBI is recommended only if plans are in place to provide necessary follow-up, including medical evaluation for persons with positive screening results and treatment for persons diagnosed with LTBI. Before QFT testing is contemplated, arrangements should be made with a qualified laboratory to perform the test. The Minnesota Department of Health (MDH) TB Prevention and Control Program is not aware of any facility or laboratory in Minnesota that currently uses or performs the QFT test. How ever, MDH is interested in determining whether any facilities in Minnesota have used QFT (or plan to do so) and in learning from those experiences. If your facility is conducting (or consider ing implementation of) QFT testing, please contact the MDH TB Program’s Nurse Consultant, Deb Sodt, at (612) 676-5421. A fact sheet regarding QFT is available on the CDC website at http:// www.cdc.gov/nchstp/tb/pubs/ tbfactsheets/250103.htm. with infectious TB; References: • screening of children less than 17 years of age, pregnant women, or persons with clinical conditions (e.g., HIV infection) that increase the risk for progression of LTBI to TB disease; 18 1. Centers for Disease Control and Prevention. Guidelines for using the QuantiFERON®-TB test for diagnosing latent Mycobacterium tuberculosis infection. MMWR 2003;52(No. RR-2):1518. DCN Readership Alert and Survey The Minnesota Department of Health (MDH) Disease Control Newsletter (DCN) has been published for over 20 years. The printed newsletter is mailed free of charge to every licensed physician in Minnesota and to other health care profes sionals who desire to receive it. We currently send each issue to over 17,000 individuals. Eight to 10 issues are pub lished annually, including a yearly issue devoted to an annual summary of communicable diseases reported in Minnesota. Issues of the DCN are posted on the MDH website (http://www.health.state.mn.us/divs/dpc/ades/pub.htm). Due to cutbacks in federal and state budgets that fund publication of the DCN, we are prompted to evaluate both the content and format of the newsletter. To facilitate this assessment, please complete this brief survey. You may complete this form and mail or fax it to MDH, or you may access and complete the survey online at http://www.health.state.mn.us/ divs/dpc/ades/dcn/rdr_survey.cfm. Your opinions are valuable to us. Thank you for completing the survey. Name (optional):______________________________________________________ 1. Do you receive the DCN directly by mail? Yes___ No___ 2. How much of a DCN issue do you typically read? All ___ Most___ Some____ None___ 3. Do you access the DCN on the MDH website? Often ___ Sometimes ___ Never ____ 4. On a scale of 1 to 5, with 1 being “NOT USEFUL” and 5 being “HIGHLY USEFUL”, how do you rate the DCN for providing useful information? 1 2 3 4 5 5. If we were to stop printing and mailing the DCN, how often would you access DCN issues on the MDH website? Often ____ Sometimes ______ Never ____ 6. If we were to create an e-mail distribution list to disseminate electronic copies of the DCN, would you subscribe? Yes ____ No ____ 7. By what method would you prefer to receive the DCN (select one)? Printed and mailed ___ E-mail distribution list ____ On-line at MDH website _____ 8. What types of articles do you find particularly useful in the DCN? (select all that apply) Annual summary of communicable diseases ___ Reprints/excerpts of recently released clinical/public health guidelines ____ Antibiogram ___ Summaries of recent state/local outbreak investigations ____ Non-communicable disease issues (e.g., cancer) _____ Other (specify): _____________________________________________ 9. Your occupation: Physician___ Nurse ____ Public health professional ___ Laboratorian ____ Other (specify): ____________________________________ 10. If you are a physician, what is your speciality? Infectious Disease ___ Family Practice ___ Pediatrics ___ Internal Medicine ____ OB/GYN ____ Other (specify): _____________________________________ Please provide any additional comments regarding the DCN, its future, and/or about topics you would like to see ad dressed in the DCN: ________________________________________________________________________________________________________ ________________________________________________________________________________________________________ ______________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________ Thank you. Please fax this page to MDH at: (612) 676-5743 OR Mail to: Val Solovjovs Acute Disease Investigation and Control Minnesota Department of Health 717 SE Delaware St. Minneapolis, MN 55414 OR You can access and complete this survey on our website at http://www.health.state.mn.us/divs/dpc/ades/dcn/ rdr_survey.cfm. . 19 Please complete the survey on page 19. To report a communicable disease to the Minnesota Department of Health call 612-676-5414 or (toll-free) 1-877-676-5414 Aggie Leitheiser, Acting Commissioner of Health Division of Infectious Disease Epidemiology, Prevention and Control Harry F. Hull, M.D. ........................... Division Director & State Epidemiologist Richard N. Danila, Ph.D., M.P.H. ............................... ADIC Section Manager Kirk Smith, D.V.M., Ph.D. ...................................................................... Editor Wendy Mills, M.P.H. .............................................................. Assistant Editor Valerie Solovjovs ................................................................. Production Editor CHANGING YOUR ADDRESS? Please correct the address below and send it to: DCN MAILING LIST Minnesota Department of Health 717 Delaware Street SE PO Box 9441 Minneapolis, MN 55440-9441 The Disease Control Newsletter is available on the MDH Acute Disease Investigation and Control (ADIC) Section web site (http://www.health.state.mn.us/divs/dpc/ades/pub.htm). The Disease Control Newsletter toll-free telephone number is 1-800-366-2597.