* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Circulation Research
Survey
Document related concepts
Transcript
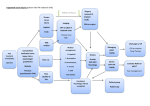
Circulation Research JUNE VOL. XXVIII 1971 NO. 6 An Official Journal of the American Heart Association Pressor Reflexes Produced by Stimulation of Afferent Fibers in the Cardiac Sympathetic Nerves of the Cat Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017 By D. Fred Peterson and Arthur M . Brown ABSTRACT Afferent fibers in cardiac sympathetic nerves were stimulated electrically in an attempt to evoke circulatory reflexes. A pressor response was always elicited during stimulation of the central end of the cut left inferior cardiac or pericoronary nerve in vagotomized intact-brain or spinal cats. The maximum blood pressure rise was 21.5 mm Hg during inferior cardiac nerve stimulation and 14.1 mm Hg during pericoronary nerve stimulation. Heart rate and respiration were unaffected by stimulation. The alpha-receptor-blocking agent phenoxybenzamine hydrochloride abolished the pressor resp3nse. Sequential sectioning of cardiac nerves arising from either the stellate ganglion or the thoracic sympathetic trunk, or of white rami 1 through 4, indicated that each branch carried afferents contributing to the pressor response. Evoked potentials revealed that excitation of ASfibersin the inferior cardiac nerve elicited a weak pressor response, and excitation of Cfibersprovoked a much stronger response. C fiber continuity between the pericoronary nerve and the inferior cardiac nerve was demonstrated. KEY WORDS evoked potential pericoronary nerve sympathetic reflex vagotomy phenoxybenzamine hydrochloride inferior cardiac nerve • Spinal sympathetic reflexes initiated by physiological stimulation of cardiovascular receptors have been described recently (1-3). They include an excitatory spinal sympathetic reflex elicited by increases in coronary pressure and a similar reflex provoked by myocardial ischemia (1, 2). Some receptors lie in or near the coronary arteries (4). The nerve fibers to which they are connected are in the From the Departments of Physiology and Medicine, University of Utah Medical Center, Salt Lake City, Utah 84112. This study was supported by U. S. Public Health Service Grant HE 05875-01, IROI HE 10977-01, and IROI NS 09545-01. Dr. Brown is an Established Investigator of the American Heart Association. Received January 14, 1971. Accepted for publication March 4, 1971. Reiewcb, Vol. XXV1I1, Jane 1971 cardiac sympathetic nerves and appear to enter the spinal cord through the upper five dorsal roots (5). Efferent sympathetics from which these reflexes have been recorded in spinal animals are in the third thoracic ramus communicans and the inferior cardiac nerve. The evidence for such excitatory spinal sympathetic reflexes originating from cardiac receptors has thus far been wholly electroneurographic. Reflex effects on blood pressure and heart rate due to changes in coronary pressure have not been established in previous experiments on spinal animals. There are several reasons for this. (A) Accumulation of vasoactive substances or vasodilator metabolites secondary to extensive surgery (6). (B) Change in cardiac performance when coro605 606 Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017 nary flow is altered, particularly when flow is reduced. (C) Depression of nervous and circulatory systems following acute spinal transection. We have circumvented the first two of these problems by electrically stimulating the central end of the cut pericoronary nerve in vagotomized, intact-brain or spinal cats. However, in addition to stimulating afferent fibers from receptors in or near the coronary arteries, fibers from receptors elsewhere in the heart projecting to the spinal cord through the cardiac sympathetic nerves (7) were also stimulated. The results show that stimulation of these afferent fibers produces a rise in blood pressure due to sympathetic vasoconstriction. They confirm and extend the finding that cardiac spinal sympathetic reflexes are primarily excitatory. This must be contrasted with cardiac and cardiovascular reflexes mediated through the vagi, carotid sinus nerves, and medulla that mainly inhibit sympathetic activity. Methods Experiments were performed on 23 cats weighing 2.5 to 5.0 kg anesthetized with sodium pentobarbital (0.5 ml/kg) injected intraperitoneally. The femoral vein was cannulated for subsequent administration of anesthetic or drugs. The trachea was cannulated and in all except five cats (see below), intermittent positive pressure respiration was begun. The stroke of the pump was adjusted to suppress spontaneous respiration by the animal. Loose ligatures were placed around the cervical vagi to facilitate sectioning later. Arterial blood pressure was recorded by a pressure transducer (Statham, Model P23dB) connected to a polyethylene catheter that had been passed through a femoral artery to the aorta. Body temperature was maintained with an electric heating pad placed under the animal. Two surgical approaches were used. 1. In each of 18 experiments, the animal was placed on its back and the thoracic cavity exposed via a bilateral incision between the fourth and fifth ribs. When necessary, ribs on the left side were removed to fully expose the region between the left stellate ganglion and the middle of the heart. This made possible access to the inferior cardiac nerve as well as to the pericoronary nerve. Anatomical arrangement of the innervation of this region is shown in Figure 1. PETERSON, BROWN Vl\| Schematic drawing of the left thoracic sympathetic trunk, stellate ganglion and their neural connections to the heart. A = aorta; CA = coronary artery; CAS = caudal limb of the ansa subclavia; CN = cardiac nerve; CSN = cervical sympathetic nerve; ICN = inferior cardiac nerve; PA = pulmonary artery; PCN = pericoronary nerve; Rj-R4 = white and gray rami; RAS = rostral limb of the ansa subclavia; SG = stellate ganglion; TSN = thoracic sympathetic nerve trunk; VN = vertebral nerve; X = vagus nerve. The usual arrangement of the stimulating (S) and recording (R) electrodes are shown. The inferior cardiac nerve was prepared by separating a length of 5 to 10 mm from the surrounding connective tissue. In 11 experiments, the left auricular flap was reflected to expose the left atrioventricular groove, and the left pericoronary nerve was separated from the surrounding connective tissue. Because of difficulties in making permanent mineral oil pools, the exposed nerves were covered with warm, saline-soaked gauze. During periods of Circulation Research, Vol. XXVIII, June 1971 CARDIAC SYMPATHETIC PRESSOR REFLEX Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017 stimulation, nerves were dried and suspended in air. 2. In five experiments, the left stellate ganglion and its major branches were exposed without entering the thoracic cavity, as described by Brown (5). This permitted the animal to breathe spontaneously during stimulation of the inferior cardiac nerve. Respiration was recorded with a concentric, bipolar electrode inserted into an external intercostal muscle. Bipolar hook electrodes (platinum-iridium) were used for both stimulating and recording. Square pulses were generated from a Grass SD9 stimulator. Intensity, frequency, and duration of the stimulus were varied in order to determine the optimum response for each animal. Except when otherwise noted, responses were elicited by rectangular pulses of 2.5 or 5.0 volts at a frequency of 15/sec and a duration of 5 msec. The period of stimulation was about 30 seconds. Blood pressure was monitored continuously on a Honeywell Visicorder (Model 1508), and in some experiments was stored on tape using an Ampex Tape Recorder (Model 1300). Evoked potentials were recorded from the inferior cardiac nerve after suitable amplification using a Grass DP9 a-c preamplifier (10-3KC). In two cats, the potentials were evoked by stimulating the pericoronary nerve, and in two other cats, the distal end of the inferior cardiac nerve was stimulated. These potentials were recorded on a storage oscilloscope record camera (Fairchild Type 450 A). In three experiments, phenoxybenzamine hydrochloride (3 to 5 mg/kg Dibenzyline, Smith, Kline and French) was administered intravenously to block alpha-receptor sites. The effectiveness of blockade was demonstrated by injection of norepinephrine (5/xg/kg DL-arterenol HC1, Sigma). In two experiments, the spinal cord was sectioned at the Cj level. Nerve stimulation was begun about two hours after spinal section. Periodically, corneal reflexes were tested and, if necessary, supplemental doses of pentobarbital (1/6 to 1/8 the initial dose) were given. Results It has been shown that changes in coronary arterial pressure excite afferent sympathetic fibers in the inferior cardiac nerve (1, 5). Therefore, the circulatory effects of stimulating these fibers were studied initially. However, this nerve contains afferent fibers from thoracic viscera other than the heart. For this reason, the effects of stimulating cardiac afferent fibers in the pericoronary nerve were Circulation Research, Vol. XXVIII, Jane 1971 607 Blood pressure responses to stimulation of the central end of the cut inferior cardiac nerve. A: Response with all other nerves intact; 2.5 v, IS/sec, 5 msec duration. B: Response after bilateral cervical vagotomy; 2.5 v, 15/sec, 5 msec duration. C: Response after section of all central sympathetic connections from the stellate ganglion; 10 v, 15/sec, 5 msec duration. D: Response after bilateral cervical vagotomy in a spinal animal; 5 v, 15/sec, 5 msec duration. examined. This nerve contains afferent fibers which come solely from cardiac receptors (8). Stimulation of the central end of the cut inferior cardiac nerve when all other nerves were intact produced a pressor response (Fig. 2A). Similar stimulation after unilateral or bilateral cervical vagotomy also produced an increase in blood pressure usually of greater magnitude (Fig. 2B, Table 1). In no case did stimulation significantly change heart rate. In the five experiments in which the pleura remained intact and respiration was spontaneous, there was no significant change in 608 PETERSON, BROWN Latency and Peak Pressor Response to Nerve Stimulation in Vagotomized Cats Latency (sec) Onset Peak Peak response (mm Hg) Inferior cardiac nerve (10) Pericoronary nerve (11) 5.4 =±= 0.75 20.4 =*= 2.44 4.1 ± 0.43 14.9 ± 1.46 21.5 =±= 2.39 14.1 ± 1.44 Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017 Values are mean ± SE. Number in parentheses is number of animals. respiration rate. The blood pressure and heart rate responses were similar in these experiments. Sequential sections of the vertebral nerve and the first three thoracic white rami reduced the response but did not eliminate it entirely. Subsequent section of the thoracic trunk below the third white ramus always eliminated the response (Fig. 2C). In two cats with spinal cords previously severed at the Ci level, the pressor response persisted (Fig. 2D), although it was smaller than in intact animals. The response was present both before and after bilateral cervical vagotomy. In one of these cats, cutting all central connections of the left stellate ganglion abolished the pressor response. Injection of phenoxybenzamine hydrochloride in two cats eliminated the response to stimulation of the inferior cardiac nerve. The blocking effect of this dose was verified by abolition of the pressor response following injection of norepinephrine. Prior to phenoxybenzamine hydrochloride, norepinephrine produced a rise in blood pressure of 60 to 90 mmHg. Stimulation of the central end of the cut pericoronary nerve with all other nerves intact produced a drop in blood pressure and a slowing of the heart rate in eight of eleven experiments (Fig. 3A). In the three remaining experiments, stimulation produced a pressor effect with no change in heart rate. We suspected that the bradycardia and hypotension were due to stimulation of cardiac vagal afferents in the pericoronary nerve. It was anticipated that bilateral cervical vagotomy would convert the depressor response to a pressor response, since the pericoronary nerve should also contain cardiac afferent fibers which run centrally in the cardiac sympathetic nerves (1, 2). In those eight experiments in which pericoronary stimulation produced a depressor effect, left cervical vagotomy caused no change, but right cervical vagotomy, either before or after left vagotomy, was followed by the predicted pressor response (Fig. 3B, Table 1). The pressor response was not accompanied by changes in heart rate. Complete left stellectomy and section of the third and fourth white rami eliminated the pressor response to left pericoronary nerve stimulation in two of three cases. In the third case, complete elimination of the response did not occur until the right stellate ganglion was excised as well. This is consistent with the finding that branches emanating from the right stellate ganglion join the left pericoronary nerve (8). FIGURE 3 Blood pressure response to stimulation of the central end of the cut pericoronary nerve. A: Response with all other nerves intact; 2.5 v, 15/sec, 5 msec duration. B: Response after bilateral cervical vagotomy; 2.5 v, 15/sec, 5 msec duration. C: Response after receptor block with phenoxybenzamine hydrochloride, 5 mg/kg. Circulation Research, Vol. XXV11I, June 1971 CARDIAC SYMPATHETIC PRESSOR REFLEX 609 Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017 FIGURE 4 Correlation between evoked potentials in the inferior cardiac nerve and blood pressure responses. A: Evoked potential of AS velocity with accompanying slight blood pressure rise (5 mm Hg); 10 v, 15/sec, 0.05 msec duration. B: Evoked potentials of As and C fiber velocities with accompanying large blood pressure change; 10 v, 15/sec, 0.1 msec duration. The larger AS wave in this record is due to a change in recording conditions. C: Evoked potential in a slip Of fibers from the inferior cardiac nerve during stimulation of the pericoronary nerve; 5 v, 0.5 msec duration. In three experiments, afferent pathways between the pericoronary nerve and stellate ganglion or sympathetic trunk were investigated. Pressor response to pericoronary nerve stimulation was demonstrated after bilateral cervical vagotomy and right stellectomy. Sequential sectioning of the left inferior cardiac nerve and other cardiac nerves indicated in Figure 1 demonstrated that each nerve contributed to the pressor response to stimulation. The response was totally abolished only after the final section. Stimulation of the central end in each of these cut nerves elicited a pressor response. Injection of phenoxybenzamine hydrochloride in one vagotomized cat eliminated the response to stimulation of the pericoronary nerve (Fig. 3C). In two animals, occlusion of the blood supply to the adrenal glands, using ligatures, did not alter the pressor response to pericoronary nerve stimulation in the vagotomized cat. Release of the ligatures in one cat was followed by an increase of 39 mm Hg in blood pressure. In one cat in which the spinal cord had been previously severed at the d level the Circulation Reiearch, Vol. XXVlll, June 1971 pressor response to pericoronary nerve stimulation was present both before and after bilateral cervical vagotomy. This response was not as great as that in the intact animal, however. Stimulation of the central end of the cut inferior cardiac nerve elicited two distinct compound potentials in the same nerve. In one animal, the first appeared at 10 v and 0.05 msec and had a conduction velocity of 10 to 20 m/sec (Fig. 4A), and fell in the AS category of afferent nerve fibers (9). With stronger currents (10 v, 0.1 msec), a second, larger evoked potential with a conduction velocity of 1 m/sec appeared (Fig. 4B). Such fibers belong to the C class (9), and many of them are undoubtedly postganglioriic sympathetic sC fibers. However, some of them are probably afferent or drC fibers (9), as we shall demonstrate subsequently. In two experiments, stimulation of the central end of the cut inferior cardiac nerve at voltages which were supramaximal for the AS fibers but below threshold for C fibers, evoked a small rise in mean arterial blood pressure (5 PETERSON, BROWN 610 Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017 mm Hg) (Fig. 4A). When the voltages were made supramaximal for the C fibers, much larger increases in mean blood pressure occurred (Fig. 4B). Stimulation of the central end of the cut pericoronary nerve in two experiments elicited a C potential in the inferior cardiac nerve (Fig. 4C). There was no evidence of an A8 component. The rise in blood pressure evoked by such stimulation occurred when the C elevation was evoked in the inferior cardiac nerve (two experiments). Discussion The nature and location of the cardiac receptors that send their afferent fibers centrally in the pericoronary nerve is only partially known. Brown and Malliani (unpublished observations) found some afferent fibers in the third thoracic ramus communicans excited by increases or decreases in coronary flow which were silenced when the pericoronary nerve was cut. However, other cardiac receptors located in the atria and ventricles may also have fibers in this nerve. Nevertheless, stimulation of this population of fibers produced a reflex rise in blood pressure in vagotomized intact-brain and spinal animals; the hypertension was due to reflex sympathetic vasoconstriction. This result is in agreement with the finding of Brown and Malliani (1) that changes in coronary flow in spinal, vagotomized cats evoked a reflex increase in sympathetic efferent discharge. Thus there is further support for the idea that excitatory sympathetic reflexes restricted at least in part to the spinal cord are mediated by afferent fibers originating from cardiac receptors that run in the cardiac sympathetic nerves. Moreover, the present experiments show that a significant rise in blood pressure results from such reflexes. The afferent fibers in the pericoronary nerve run to the stellate ganglion and sympathetic trunk in at least five branches and probably a relatively small percent of the fibers are found in each branch. This fact, combined with the technical problem of stimulating a short (2 to 3 mm) length of nerve while the heart is beating, probably accounts for the difficulty in evoking potentials in the inferior cardiac nerves from the pericoronary nerve. It is therefore not possible at this stage to identify definitely which fiber groups are involved. However, stimulation of AS and afferent C fibers in the inferior cardiac nerve elicited a pressor reflex similar to that elicited from the pericoronary nerve with the afferent C fibers making the larger contribution. Since we were able to evoke a C potential in the inferior cardiac nerve from the pericoronary nerve, these fibers (if they are indeed afferent) mav have been responsible for the effect of pericoronary nerve stimulation. Acknowledgment We thank Dr. Diana L. Kunze for her helpful criticism of this work and manuscript. References 1. BROWN, A.M., AND MALLIANI, A.: Spinal sympathetic reflexes initiated by coronary receptors. J Physiol (London), in press. 2. MALLIANI, A., AND BROWN1, A.M.: Reflexes arising from coronary receptors. Brain Res 24:352-355, 1970. 3. MALLIANI, A., SCHWARTZ, P.J., AND ZANCHETTI, A.: A sympathetic reflex elicited by experimental coronary occlusion. Amer J Physiol 217:703-709, 1969. 4. ABRAHAM, A.: Microscopic innervation of the heart and blood vessels in vertebrates including man. Oxford, Pergamon Press, 1969, pp 210211. 5. BHOWN, A.M.: Excitation of afferent cardiac sympathetic nerve fibers during myocardial ischaemia. J Physiol (London) 190:35-53, 1967. 6. MILLAR, R.A., AND MORRIS, M.E.: Sympatho- adrenal responses during general anesthesia in dog and man. Canad Anaesth Soc J 8:356386, 1961. 7. HEYMANS, C , AND NEIL, E.: Reflexogenic areas of the cardiovascular system. Boston, Little, Brown & Co., 1958, pp 109-110. 8. MCKIBBEN, J.S., AND GETTY, R.: Comparative morphologic study of the cardiac innervation in domestic animals: II. The feline. Amer J Anat 122:545-554, 1968. 9. RUCH, T.C., AND PATTON, H.D.: Physiology and Biophysics, 19th ed., Philadelphia, W. B. Saunders Co., 1965, pp 81-83. Circulation Research, Vol. XXVlll, June 1971 Pressor Reflexes Produced by Stimulation of Afferent Fibers in the Cardiac Sympathetic Nerves of the Cat D. FRED PETERSON and ARTHUR M. BROWN Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017 Circ Res. 1971;28:605-610 doi: 10.1161/01.RES.28.6.605 Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1971 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7330. Online ISSN: 1524-4571 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circres.ahajournals.org/content/28/6/605 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation Research is online at: http://circres.ahajournals.org//subscriptions/