* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 0 150 E E 0 VENT RIC ULAR VOLUME ml
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Rheumatic fever wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Aortic stenosis wikipedia , lookup
LETTERS TO THE EDITOR
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
tive prosthetic orifice size may have to be performed at least a few
weeks after valve insertion. Second, in some patients, the problem is
compounded by the small size of the annulus compared with the size
of the patient. My article was not written just to highlight the
difficulties of a small aortic annulus.
Dr. Kinsley's ability to insert a prosthetic valve size commensurate with the patient's body size is to be applauded. However, Dr.
Kinsley's letter and previous paper' leave many questions unanswered. The technique of anticipating stroke volume and tailoring
the prosthetic valve to that stroke volume is not described. The
belief that favorable hemodynamic characteristics are actually
enhanced is not based on data that have been presented. Although
gradients obtained at surgery are cited, calculated prosthetic valve
areas and valve area indices of patients studied some weeks or
months after surgery have not been presented. It would also be of interest to know how many patients had aortic valve replacement
without use of this technique during the same period of time when
the 52 patients were operated on with use of this technique. There
have been two deaths with the use of this technique, and some patients
already have aortic incompetence; moreover, the device is inserted
in an abnormal position. Before one is convinced that the technique
is safe and effective, one should know: 1) the long-term mortality
and morbidity of patients so treated and the data analyzed with the
use of actuarial techniques;5 and 2) the results of detailed
hemodynamic evaluation which provide information about
prosthetic valve areas, frequency and severity of valvular regurgitation and about ventricular performance.
SHAHBUDIN S. RAHIMTOOLA, M.D.
Visiting Professor
University of California, San Francisco
San Francisco, California 94143
References
1. Rahimtoola SH: The problem of valve prosthesis-patient mismatch. Circulation 58: 20, 1978
2. KonnoS, Imai Y, lida Y, Nakajuma M, Tarsuno K: A new
method for prosthetic valve replacement in congenital aortic
stenosis associated with hypoplasia of the aortic valve ring. J
Thorac Cardiovasc Surg 70: 909, 1975
3. Blank RH, Puello DF, Bessone LN, Harrison EE, ShawS:
Method of managing the small aortic annulus during valve
replacement. Ann Thorac Surg 22: 356, 1976
4. Kinsley RH: The narrow aortic annulus. A technique for inserting a larger prosthesis. Am Heart J 93: 759, 1977
5. Rahimtoola SH: Valve replacement a perspective. Am J Cardiol 35: 711, 1975
-
419
0 150
E
E
I
Ck1
LU 100
W.
In
LU
z
LU
a-
o -4+
0
20
30
VENT RIC ULAR
VOLUME ml
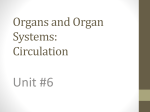
FIGURE 1. Pressure-volume trajectories of two isovolumic
contractions (a and b) and two ejecting contractions (c and
d). The arrows indicate the direction of movement of a pressure-volume data point on the trajectories. The slanted,
dashed line connecting the peak isovolumic pressures
represents the end-systolic pressure-volume relationship.
vivo type of contraction, the left upper corner of the pressurevolume loop corresponds to our end-systole.3 All these end-systoles
come on or very near a line representing the end-systolic pressurevolume relationship.3' When the pressure-volume loop of an abnormal contraction has a sharp left upper corner asloop c in figure 1,
this corner can be identified as our end-systole because it is situated
on the end-systolic pressure-volume line.
However, the identification of our end-systole is very difficult if
the pressure-volume loop of an abnormal contraction has a rounded
shoulder at its left upper part, asloop d in figure 1. The point on the
loop nearest the end-systolic pressure-volume line should be identified as our end-systole (solid circle). However, if loop d were alone
in the diagram, it would be very difficult to pinpoint the end-systole
on the loop. Obviously, the point with the smallest volume (open circle) should not be identified as the end-systole of
loop d because it
occurs late in the relaxation phase.
From our animal experiments,3 I have been impressed that the
close coincidence of the end of ejection with end-systole in natural in
vivo contractions3 is circumstantial. This coincidence is probably
due to an appropriate interaction among the heart, the valve and the
artery. If this interaction becomes abnormal, the end ofejection
may no longer coincide with the end-systole, and the identification
of the end of ejection as the end of systole may no longer be correct.
Further studies are needed to discover the relationship between the
ends of systole and ejection and the factors influencing this
4
End-Systolic Pressure-Volume Relations
To the Editor:
Referring to a recent article by Grossman et al.,' Dr. lizuka
commented that the end-systole identified as the moment for
the smallest volume may not necessarily be the true end-systole
contributing to the end-systolic pressure-volume relationship.' Both
Dr. lizuka's comment and Dr. Grossman's response to it emphasize
the problems in identifying the end-systole in the clinical setting.
As one of the reserchers who originally proposed the end-systolic
pressure-volume ratio as an index of ventricular contractility from
animal experiments,3 I would like to reemphasize our definition of
end-systole to prevent misunderstanding of the end-systolic pressure-volume relationship.
There is no unanimous definition of systole and end-systole.5 In
our definition, the end of mechanical systole is the moment at which
the contraction becomes maximal and the relaxation starts. This
end-systole may not coincide with the end-systole identified as the
end of ejection or the moment of the dicrotic notch of aortic pressure. In an isovolumic contraction, the peak pressure corresponds to
our end-systole, as seen in figure 1, loops a and b. In a natural in
4
relationship.
HIROYUKI SUGA, M.D.
Department of Cardiac Physiology
National Cardiovascular Center
Suita, Osaka 565, Japan
References
1. Grossman W, Braunwald E, Mann T, McLaurin LP, Green LH:
Contractile state of the left ventricle in man as evaluated from
end-systolic pressure-volume relations. Circulation 56: 845, 1977
2. lizuka M: End-systolic pressure-volume relations. Circulation
58: 379, 1978
3. Suga H, Sagawa K, Shoukas AA: Load independence of the in-
CIRCULATION
420
stantaneous pressure-volume ratio of the canine left ventricle and
the effects of epinephrine and heart rate on the ratio. Circ Res
32: 314, 1973
4. Suga H, Sagawa K: Instantaneous pressure-volume relationships
and their ratio in the excised, supported canine left ventricle. Circ
Res 35: 117, 1974
5. Remington JW: Introduction to muscle mechanics, with a
glossary of terms. Fed Proc 21: 954, 1962
"Trifascicular Block"
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
To the Editor:
In a recent comment relating to my paper, "Prognosis for Patients with Congenital Heart Disease and Postoperative Intraventricular Conduction Defects," (Circulation 57: 867, 1978), Dr.
Gillette states that an error in terminology should be brought to the
attention of the readers. There is no error in this paper.
Dr. Gillette's argument is that the term "trifascicular block" is an
electrocardiographic pattern which may result from various
etiologies, such as a true trifascicular disease, or "bifascicular disease" and His bundle and/or atrioventricular (AV) nodal disease or
no fascicular disease and P-R prolongation due to atrial conduction
delay due to atrial enlargement. This last pattern is commonly seen
in patients with various types of AV canal defects and other congenital heart defects.'
I wholeheartedly agree with Dr. Gillette's comment that
"trifascicular block" is a misnomer referring to a descriptive electrocardiographic pattern rather than to an implication of an underlying pathophysiologic mechanism or process. Indeed, our group
has commented extensively in the past on this problem and the risks
involved by confusing descriptive electrocardiograpnic terminology
with possible underlying pathophysiologic mechanisms.2'5
Because of the brevity of descriptive terms and the day-to-day
convenience inherent in the use of these terms, rather than a long explanation of a possible mechanism, their use is extremely
widespread. For example, "bifascicular block," "AV block," "intraventricular conduction defects" - all may be due to mechanisms
other than "block" as implied in these terms.
We have previously stated that "attempts to indicate a precise
VOL 59, No 2, FEBRUARY 1979
electrophysiologic mechanism from the scalar electrocardiogram
may lead- to oversimplification and misinterpretation of the true
underlying cardiac abnormality."4
The section referred to by Dr. Gillette is entitled, Right Bundle
Branch Block and Left Anterior Hemiblock Pattern and P-R
Prolongation ("trifascicular block pattern"). Use of quotation
marks for identification of a mistaken idea is common and proper in
the English language (Professor Michael Hayes, Department of
English, Columbia University: personal communication), and I
used it extensively throughout the article when I felt that the term
used did not properly reflect the underlying pathophysiologic
mechanism. When Dr. Gillette uses the term "trifascicular disease"
in an identical way to mine, he identifies the underlying impropriety
of this term by placing it within quotation marks.
EHUD KRONGRAD, M.D.
Babies Hospital
New York, New York
References
1. Ongley PA, DuShane JW: Counterclockwise superiorly
displaced frontal plane loops of the vectorcardiogram in
children. In Vectorcardiography, edited by Hoffman I, Taymor
RC. Philadelphia, JB Lippincott Co, 1966, p 339
2. Steeg CN, Krongrad E, Davachi F, Bowman FO Jr, Gersony
WM: Post-operative left anterior hemiblock and the right bundle
branch block following repair of tetralogy of Fallot: clinical and
etiologic considerations. Circulation 51: 1026, 1975
3. Gersony WM, Krongrad E: The patient with congenital heart
disease following surgical correction: a long-term overview.
Progr Cardiovasc Dis 18: 29, 1975
4. Schatz J, Krongrad E, Malm JR: Left anterior and left posterior
hemiblock in tricuspid atresia and transposition of the great
vessels. Observations on electrocardiographic nomenclature and
electrophysiologic mechanism. Circulation 54: 1010, 1976
5. Steeg CN, Krongrad E: Disorders of A-V conduction in children.
In The Anatomic, Physiologic and Pharmacologic Basis for the
Diagnosis and Management of Arrhythmias in Children, edited
by Roberts NK, Gelband H. New York, Appleton-CenturyCrofts, 1977, pp 211-230
End-systolic pressure-volume relations.
H Suga
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Circulation. 1979;59:419-420
doi: 10.1161/01.CIR.59.2.419
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1979 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/59/2/419.citation
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/