* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Heart Valves
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
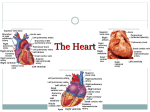
Anatomy and physiology of the heart The heart is composed of three layers :1- The inner layer, or endocardium, consists of endothelial tissue and lines the inside of the heart and valves. 2- The middle layer, or myocardium, is made up of muscle fibers and is responsible for the pumping action. 3-The exterior layer of the heart is called the epicardium. -The heart is encased in a thin, fibrous sac called the pericardium, which is composed of two layers. Adhering to the epicardiumis the visceral pericardium. Enveloping the visceral pericardium is the parietal pericardium, a tough fibrous tissue that attaches to the great vessels, diaphragm, sternum, and vertebral column and supports the heart in the mediastinum. The space between these two layers (pericardial space) is filled with about 30 mL of fluid, which lubricates the surface of the heart and reduces friction during systole. Heart Chambers:The four chambers of the heart constitute the right- and left sided pumping systems. The right side of the heart, made up of the right atrium and right ventricle, distributes venous blood (deoxygenated blood) to the lungs via the pulmonary artery (pulmonary circulation) for oxygenation. The right atrium receives blood returning from the superior vena cava (head,neck, and upper extremities), inferior vena cava (trunk and lower extremities), and coronary sinus (coronary circulation). The left side of the heart, composed of the left atrium and left ventricle, distributes oxygenated blood to the remainder of the body via the aorta (systemic circulation). The left atrium receives oxygenated blood from the pulmonary circulation via the pulmonary veins. The relationships of the four heart chambers are shown in The varying thicknesses of the atrial and ventricular walls relate to the workload required by each chamber. The atria are thin-walled because blood returning to these chambers generates low pressures. In contrast, the ventricular walls are thicker because they generate greater pressures during systole. The right ventricle contracts against low pulmonary vascular pressure and has thinner walls than the left ventricle. The left ventricle, with walls two-and-a-half times more muscular than those of the right ventricle, contracts against high systemic pressure. Because the heart lies in a rotated position within the chest cavity, the right ventricle lies anteriorly (just beneath the sternum) and the left ventricle is situated posteriorly. The left ventricle is esponsible for the apex beat or the point of maximum impulse (PMI), which is normally palpable in the left midclavicular line of the chest wall at the fifth intercostal space. Heart Valves:The four valves in the heart permit blood to flow in only one direction. The valves, which are composed of thin leaflets of fibrous tissue, open and close in response to the movement of blood and pressure changes within the chambers. There are two types of valves: atrioventricular and semilunar ATRIOVENTRICULAR VALVES:The valves that separate the atria from the ventricles are termed atrioventricular valves. The tricuspid valve, so named because it is composed of three cusps or leaflets, separates the right atrium from the right ventricle. The mitral, or bicuspid (two cusps) valve, lies between the left atrium and the left ventricle Normally, when the ventricles contract, ventricular pressure rises, closing the atrioventricular valve leaflets. Two additional structures, the papillary muscles and the chordae tendineae, maintain valve closure. The papillary muscles, located on the sides of the ventricular walls, are connected to the valve leaflets by thin fibrous bands called chordae tendineae. During systole, contraction of the papillary muscles causes the chordae tendineae to become taut, keeping the valve leaflets approximated and closed. SEMILUNARVALVES:The two semilunar valves are composed of three half-moon-like leaflets. The valve between the right ventricle and the pulmonary artery is called the pulmonic valve; the valve between the left ventricle and the aorta is called the aortic valve FUNCTIONOFTHEHEART:CONDUCTIONSYSTEM:The specialized heart cells of the cardiac conduction system methodically generate and coordinate the transmission of electrical impulses to the myocardial cells. The result is sequential atrioventricular contraction, which provides for the most effective flow of blood, thereby optimizing cardiac output. Three physiologic characteristics of the cardiac conduction cells account Automaticity:- for ability this to initiate coordination: an electrical impulse Excitability:- ability to respond to an electrical impulse Conductivity:- ability to transmit an electrical impulse from one cell to another. The sinoatrial (SA) node, referred to as the primary pacemaker of the heart, is located at the junction of the superior vena cava and the right atrium. The SA node in a normal resting heart has an inherent firing rate of 60 to 100 impulses per minute, but the rate can change in response to the metabolic demands of the body. The electrical impulses initiated by the SA node are conducted along the myocardial cells of the atria via specialized tracts called inter nodal pathways. The impulses cause electrical stimulation and subsequent contraction of the atria. The impulses are then conducted to the atrioventricular (AV) node. The AV node (located in the right atrial wall near the tricuspid valve) consists of another group of specialized muscle cells similar to those of the SA node. The AV node coordinates the incoming electrical impulses from the atria and, after a slight delay (allowing the atria time to contract and complete ventricular filling), relays the impulse to the ventricles. This impulse is then conducted through a bundle of specialized conduction cells (bundle of His) that travel in the septum separating the left and right ventricles. The bundle of His divides into the right bundle branch (conducting impulses to the right ventricle) and the left bundle branch (conducting impulses to the left ventricle). To transmit impulses to the largest chamber of the heart, Physiology of Cardiac Conduction:Cardiac electrical activity is the result of the movement of ions (charged particles such as sodium, potassium, and calcium) across the cell membrane. The electrical changes recorded within a single cell result in what is known as the cardiac action potential In the resting state, cardiac muscle cells are polarized, which means an electrical difference exists between the negatively charged inside and the positively charged outside of the cell membrane. As soon as an electrical impulse is initiated, cell membrane permeability changes and sodium moves rapidly into the cell, while potassium exits the cell. This ionic exchange begins depolarization (electrical activation of the cell), converting the internal charge of the cell to a positive one. Contraction of the myocardium follows depolarization. The interaction between changes in membrane voltage and muscle contraction is called electromechanical coupling. As one cardiac muscle cell is depolarized, it acts as a stimulus to its neighboring cell, causing it to depolarize. Sufficient depolarization of a single specialized conduction system cell results in depolarization and contraction of the entire myocardium. Repolarization (return of the cell to its resting state) occurs as the cell returns to its baseline or resting state; this corresponds to relaxation of myocardial muscle. CARDIAC CYCLE:- Beginning with systole, the pressure inside the ventricles rapidly rises, forcing the atrioventricular valves to close. As a result, blood ceases to flow from the atria into the ventricles and regurgitation (backflow) of blood into the atria is prevented. The rapid rise of pressure inside the right and left ventricles forces the pulmonic and aortic valves to open, and blood is ejected into the pulmonary artery and aorta, respectively. The exit of blood is at first rapid then, as the pressure in each ventricle and its corresponding artery equalizes, the flow of blood gradually decreases. At the end of systole, pressure within the right and left ventricles rapidly decreases. This lowers pulmonary artery and aortic pressure, causing closure of the semilunar valves. These events mark the onset of diastole. During diastole, when the ventricles are relaxed and the atrioventricular valves are open, blood returning from the veins flows into the atria and then into the ventricles. Toward the end of this diastolic period, the atrial muscles contract in response to an electrical impulse initiated by the SA node (atrial systole). The resultant contraction raises the pressure inside the atria, ejecting blood into the ventricles. Cardiac Output:Cardiac output is the amount of blood pumped by each ventricle during a given period. The cardiac output in a resting adult is about 5 L per minute but varies greatly depending on the metabolic needs of the body. Cardiac output is computed by multiplying the stroke volume by the heart rate. Stroke volume is the amount of blood ejected per heartbeat. The average resting stroke volume is about 70 mL, CONTROL OF HEART RATE:Changes in heart rate are accomplished by reflex controls mediated by the autonomic nervous system, including its sympathetic and parasympathetic divisions. The parasympathetic impulses, which travel to the heart through the vagus nerve, can slow the cardiac rate, whereas sympathetic impulses increase it. These effects on heart rate result from action on the SA node, to either decrease or increase its inherent rate. The balance between these two reflex control systems normally determines the heart rate. The heart rate is stimulated also by an increased level of circulating catecholamines (secreted by the adrenal gland) and by excess thyroid hormone, which produces a catecholamine-like effect. Heart rate is also affected by central nervous system and baroreceptor activity. Baroreceptors are specialized nerve cells located in the aortic arch and in both right and left internal carotid arteries The baroreceptors are sensitive to changes in blood pressure (BP). During elevations in BP (hypertension), these cells increase their rate of discharge, transmitting impulses to the medulla. This initiates parasympathetic activity and inhibits sympathetic response, lowering the heart rate and the BP. The opposite is true during hypotension (low BP). Hypotension results in less baroreceptor stimulation, which prompts a decrease in parasympathetic inhibitory activity in the SA node, allowing for enhanced sympathetic activity. The resultant vasoconstriction and increased heart rate elevate the BP. Cardiac Signs and Symptoms:Patients with cardiovascular disorders commonly have one or more of the following signs and symptoms: 1• Chest pain or discomfort (angina pectoris, MI, valvular heartdisease) 2• Shortness of breath or dyspnea (MI, left ventricular failure, HF) 3• Edema and weight gain (right ventricular failure, HF) 4• Palpitations (dysrhythmias resulting from myocardial ischemia, valvular heart disease, ventricular aneurysm, stress, electrolyte imbalance) 5• Fatigue (earliest symptom associated with several cardiovascular disorders) 6• Dizziness and syncope or loss of consciousness (postural hypotension, dysrhythmias, vasovagal effect, cerebrovascular disorders) Not all chest discomfort is related to myocardial ischemia. When a patient has chest discomfort, questions should focus on differentiating a serious, life-threatening condition such as MI from conditions that are less serious or that would be treated differently. -The following points should be remembered when assessing patients with cardiac symptoms: 1• Women are more likely to present with atypical symptoms of MI than are men. 2• There is little correlation between the severity of the chest discomfort and the gravity of its cause. Elderly people and those with diabetes may not have pain with angina or MI because of neuropathies. Fatigue and shortness of breath may be the predominant symptoms in these patients. 3• There is poor correlation between the location of chest discomfort and its source. 4• The patient may have more than one clinical condition occurring simultaneously. 5• In a patient with a history of CAD, the chest discomfort should be assumed to be secondary to ischemia .