* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular System
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
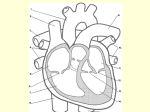
Heart • Considered to be a duel pump because the both sides work independently of one another. • The right side pumps blood to the lungs. – (pulmonary circulation) • The left side pumps blood to all of the other organs of the body – (systemic circulation) Pathway of Blood Through the Heart and Lungs Major Vessels of the Heart • Vessels returning blood to the heart include: – Superior and inferior venae cavae – Right and left pulmonary veins • Vessels carrying blood away from the heart include: – Pulmonary trunk, which splits into right and left pulmonary arteries – Ascending aorta (three branches) –, left common carotid, and subclavian arteries Figure 19.5a Figure 19.5b Ventricles of the Heart • Ventricles eject blood from the heart – Right ventricle pumps blood into the pulmonary trunk which will go to the lungs. • Left ventricle pumps blood into the aorta which will go to the rest of the body Atrioventricular Heart Valves • • Heart valves ensure unidirectional blood flow through the heart. Atrioventricular (AV) valves lie between the atria and the ventricles. – – • • Tricuspid Right Bicuspid (Mitral) Left AV valves prevent backflow of blood into the atria when ventricles contract. Chordae tendineae anchor AV valves to papillary muscles – First heart sound (LUB) when valves close • During diastole there is less pressure in the in ventricle. AV Valves open and filling the ventricle. • During systole the AV valves prevent the back flow of blood into the atrium. – Failure to prevent the blood from going back into the atria (systolic heart murmur) Semilunar Heart Valves • Aortic semilunar valve lies between the left ventricle and the aorta. • Pulmonary semilunar valve lies between the right ventricle and pulmonary trunk – Semilunar valves prevent backflow of blood into the ventricles. • Second heart sound (DUB) when valves close. Figure 19.9b • During ventricular systole the semilunar valves allow blood to be ejected from the ventricles into the aorta and pulmonary trunk. • During diastole they prevent the back flow of blood back into the ventricles. – Failure to prevent the backflow of blood into the ventricles. (diastolic murmur) Coronary Arteries • Left coronary artery (LCA) – anterior interventricular branch • supplies blood to interventricular septum and anterior walls of ventricles – circumflex branch • passes around left side of heart in coronary sulcus, supplies left atrium and posterior wall of left ventricle • Right coronary artery (RCA) – right marginal branch • supplies lateral R atrium and ventricle – posterior interventricular branch • supplies posterior walls of ventricles • Cardiac muscle is short and striated. • Ability to beat independent of stimulation from the nervous system. – ANS • Functional syncytium: – intercalated discs connect cardiac cells which allow free passage of ions. – This allows the spread of action potentials from one myocyte to another. • The result is a coordinated contraction that moves the blood out of the heart. Major Vessels Figure 20.23a Figure 20.27 Figure 20.28a Mesenteric Vessels Blood Pressure (BP) • Force per unit area exerted on the wall of a blood vessel by its contained blood. – Expressed in millimeters of mercury (mm Hg) – Measured in reference to systemic arterial BP in large arteries near the heart. • The differences in BP within the vascular system provide the driving force that keeps blood moving from higher to lower pressure areas. Resistance • Resistance – opposition to flow – Measure of the amount of friction blood encounters as it passes through vessels. – Generally encountered in the systemic circulation. – Referred to as peripheral resistance (PR) • The three important sources of resistance are blood viscosity, total blood vessel length, and blood vessel diameter. Resistance Factors: Viscosity and Vessel Length • Resistance factors that remain relatively constant are: – Blood viscosity – thickness or “stickiness” of the blood the greater the resistance. – Blood vessel length – the longer the vessel, the greater the resistance encountered. • Diameter- Smaller diameter arterioles are the major determinants of peripheral resistance – Fatty plaques from atherosclerosis: decreases both diameter and elasticity of vessel which results in: • Cause turbulent blood flow • Dramatically increase resistance due to turbulence Blood Flow, Blood Pressure, and Resistance • Blood flow (F) is directly proportional to the difference in blood pressure – If P increases, blood flow speeds up; if P decreases, blood flow declines • Blood flow is inversely proportional to resistance (R) – If R increases, blood flow decreases • R is more important than P in influencing local blood pressure. EKG Why Get an EKG • Unexplained chest pain, or reduced blood flow to the heart (ischemia), shortness of breath, dizziness, fainting, or rapid and irregular heartbeats (palpitations). • Identify ventricle hypertrophy and other changes of the myocardium. • Check how well mechanical devices, such as pacemakers or defibrillators implanted in the heart, are working to control a normal heartbeat. Electrocardiography • Electrical activity is recorded by electrocardiogram (ECG) • P wave corresponds to depolarization of SA node resulting in atrial systole • QRS complex corresponds to ventricular depolarization resulting in Ventricular contraction and blood being ejected from the heart. – Atrial repolarization is hidden with in QRS complex • ST segment - ventricular systole • T wave corresponds to ventricular repolarization EKG Normal Sinus Rhythm • The heart is being paced by the SA node. There is a degree of regularity between all components of EKG • Normal heart rate ranges between 60-100bpm. – 75bpm( average) dependent on activity. • Find a QRS that falls on a solid black line. • Then count 300-150-100-75-60-50-43 for each successive black line. Distance between QRS complexes are 5 black lines =60 Beats per minute Sinus Bradycardia (SB) is defined as a sinus rhythm with a rate below 60 bpm. • Normally found in well trained persons and during sleep. • May also be found in patients post myocardial infarction • Beta Blockers reduce sympathetic input to the heart reducing both cardiac workload and blood pressure. – If on this medication heart rate is not a valid measure of exertion. Tachycardia • Defined as a heart rate greater than 100bpm – This is a perfectly normal rhythm if you are exercising. • Heart beats faster under the influence of the SNS in order to meet the bodies increased demand of oxygen. • Stress, anxiety, or underline pathology may result in an elevated HR. – Context is important. Atrial Fibrillation • Multiple ectopic foci fire chaotically in the atrium • This diminished the atriums ability to contract and results in pooling in the atrium. – (High risk of blood clot formation =need blood thinners) – Loss of atrial kick = reduced SV – May lead to a more severe arrhythmia. Premature Ventricular Contraction (PVC) Ventricles contract before the atria in a cardiac cycle The SA node is not pacing the heart here. – typically caused by emotional stress, lack of sleep, smoking or stimulants (caffeine) which initiate an AP in the ventricles Ventricular Tachycardia( V-Tach) • Heart rate greater then 150 that originates from an irritable foci in the ventricle. • It is a regular rhythm but is hemo-dynamically inefficient. The heart CO will be very poor due to reduced ventricular filling. • Reduced CO leads to poor coronary perfusion. • Will lead to Ventricular Fibrillation Ventricular Fibrillation( V-FIB) • This is the most dangerous rhythm. There is no discernable pattern. • Multiple areas of the ventricles are initiating impulses at the same time resulting in a quivering heart instead of a contracting heart. • The heart will not efficiently fill up with blood. – Oxygen will not be delivered to the tissues. – Toe tag is eminent unless a defibrillator ( AED) is near.