* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lymphatic System
Embryonic stem cell wikipedia , lookup
Cell culture wikipedia , lookup
Dictyostelium discoideum wikipedia , lookup
Microbial cooperation wikipedia , lookup
Human embryogenesis wikipedia , lookup
Cell theory wikipedia , lookup
Neuronal lineage marker wikipedia , lookup
State switching wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Developmental biology wikipedia , lookup
Regeneration in humans wikipedia , lookup
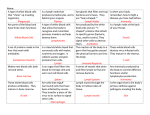
Lymphatic System Chapter 12: Body Defenses Overview Two part system: • 1. lymphatic vessels: transport fluids that have escaped from the circulatory system back to blood vessels. • 2. lymphoid tissue and organs: make and store lymphocytes and phagocytes which are important in body defense. Lymph Vessels • Interstitial fluid (AKA lymph): fluid that surrounds tissues and cells. • Most of this fluid comes from the blood in the capillaries that is forced out taking nutrients with it. • If this fluid is not returned to the capillary blood then blood volume will decrease…and that is bad!!!! • As much as 3L per day soak our tissues and that’s a lot! Lymph Vessels • Edema: fluid accumulation; too much fluid reduces the amount of nutrient exchange with cells. BAD!!! • So in come the lymph vessels to save the day! • Just like blood vessels, the lymph vessels taper to capillaries called … lymph capillaries. Lymph Vessels Lymph capillaries • Dead end vessels • Flow toward heart • Flap-like minivalves that open when there is low pressure internally (lots of interstitial fluid) and close with high internal pressure. • Large enough openings to allow large proteins, bacteria and viruses to diffuse into the vessel. Lymph Vessels • Lymph capillaries larger lymph vessels lymphatic collecting vessels lymphatic duct • Right lymphatic duct: drains from the right arm, head and thorax into the right subclavian vein. • Thoracic duct: drains from the rest of the body into the left subclavian vein. Lymphatic Vessels • No heart pump like the cardiovascular system. • BUT… – Uses one way valves, – Muscular pumps (skeletal muscles), – The respiratory pump, – And smooth muscles push lymph through large vessels. Lymph Nodes Lymph Nodes Functions: • Remove foreign substances like bacteria, viruses and cancer cells. • Produce lymphocytes: type of white blood cell that produce antibodies. • House macrophages: type of white blood cell that eat bacteria and such. • Lymph node swelling is the result of the increased production of wbc and trapping the foreign objects. Lymph Nodes Anatomy • Cluster along lymph vessels (See page 371 figure 12.3) • Kidney shaped • Less than one inch long • Surrounded by a capsule. • Trabeculae strands branch off the capsule and compartmentalize the node. Lymph Nodes Lymph Nodes Anatomy • Cortex: outer area – Follicles filled with T-lymphocytes (T-cells) – Germinal centers filled with Blymphocytes that produce plasma cells which release antibodies • Medulla: central area – House the phagocytic macrophages (cell eaters) Lymph Nodes Anatomy • Afferent vessels: flow towards the node; enter at the convex side; there are many of them • Efferent vessels: flow away from the node; out the concave side (called the hilus); there are few of them. • Flow through the node is slow allowing the filtering process to complete. Other Lymph Organs • Lymph nodes: one type of lymph organ…but there’s more! • All lymph organs have two things in common: reticular connective tissue and lymphocytes. Examples: spleen, thymus, tonsils, Peyer’s patches (MALT) Other Lymph Organs 1. SPLEEN: a. on the left side of the stomach b. Filters blood of bacteria, viruses, and debris (unlike the liver) c. Act as blood reservoir (like the liver) d. Destroy old erythrocytes and recycle parts e. Store platelets f. Produce lymphocytes Spleen Other Lymph Organs 2. THYMUS a. covered in chapter 9 as an endocrine gland b. found low in the throat by the heart c. produces hormones like thymosin that program certain lymphocytes Thymus Other Lymph Organs 3. TONSILS a. lymph tissue that surrounds the pharynx (back of throat). b. “air filter” trap bacteria and debris that enters the throat. c. can become congested with bacteria and inflamed Tonsils Other Lymph Organs • 4. PEYER’S PATCHES a. tonsils for the intestines b. many are found in the small intestine c. capture and destroy bacteria like the tonsils with macrophages d. MALT (mucosa-associated lymphatic tissue) tonsils and Peyer’s patches Peyer’s Patches Body Defenses Two systems of defense (a broad overview) • 1. nonspecific defense system – First line of defense – Responds immediately & to all foreign substances (no questions asked!) – Defenders include: intact skin, mucous membranes, inflammatory responses, and some specific blood proteins. Body Defenses • 2. specific defense system (AKA immune system) – Second line of defense – Not quick, but very specific (must be invaded by pathogen, antigen, then produce a specific antibody to attack). – Attack invaders like pathogens as well as transplants, grafts, and sometimes our own selves (autoimmune disease) – Defenders include: cells like lymphocytes and macrophages and chemicals like antibodies Nonspecific Body Defenses See table 12.1 • 1. surface membrane barriers (mechanical barrier) – Skin (lines the outside of us) and mucous membranes (lines the inside of us; respiratory, digestive, urinary tracts) – Acidic pH, toxic chemicals and enzymes • 2. cells and chemicals – Phagocytes, natural killer cells, inflammation, bacteriotoxins, and fever Nonspecific Body Defenses Cells and Chemicals A. phagocytes (cell eater): like macrophages and neutrophils Nonspecific Body Defenses Cells and Chemicals • B. Natural (born) killer cells: in blood and lymph that lyse (slice and dice) virus-infected body cells and cancer cells. – Recognize sugars on membranes of bad guys. – Release chemicals that digest plasma and nuclear membranes. – No antibodies and no phagocytosis! Nonspecific Body Defense Cells and Chemicals C. Inflammatory response (see page 375) • Steps for inflammation – – 1. injury (trauma, burn, cut, infection) – 2. chemical ALARM sent out (histamines and kinins are released by the injured cells) – 3. blood vessels dilate bringing more blood (heat and redness) – 4. capillaries leak plasma (swelling and pain) – 5. this brings lymphocytes and phagocytes to the area Nonspecific Body Defense Nonspecific Body Defense Awesome things the inflammatory response brings to you… • Prevents the spread of disease • Gets rid of damaged cells and pathogens • Prepares the tissue for repair Nonspecific Body Defense Cells and Chemicals D. Antimicrobial Chemicals: 1. Complement proteins – about 20 different proteins that float around in the blood plasma attaching themselves to the membranes of foreign bodies. a) Effects include: osmotic explosion, vasodilation, chemotaxis, opsonization Nonspecific Body Defense Cells and Chemicals D. Antimicrobial Chemicals: 2. Interferons – virus infected cells send out interferons to bind to the membrane proteins of other, noninfected cells, that new viruses would attach to. Nonspecific Body Defense E. Fever: moderate temperature elevations are helpful in two ways, but extreme temperature elevations cause damage to even healthy tissue by denaturing their proteins. – Lessens Fe and Zn needed for bacterial reproduction – Increases metabolic rates and tissue repair Specific Body Defenses • 1st line of defense is the membrane barrier (skin and mucous membranes) • 2nd line of defense are nonspecific cells and chemicals (killer cells, phagocytes, compliment and interferon proteins) • 3rd line of defense is the immune response. Specific Body Defenses Some Definitions: 1. Antigens: any foreign molecules, including, but not limited to, foreign proteins, nucleic acids, many carbohydrates, some lipids and things with these chemicals on them like bacteria, pollen, viruses, etc. 2. Haptens: small, “incomplete” antigens found in allergens like poison ivy, animal dander, 3. Antibodies: “factors”, usually proteins, that attack antigens. Specific Body Defenses • Three important aspects of the immune system… 1. It is antigen specific 2. It is systemic 3. It has a “memory” Specific Body Defenses Two arms of the immune system 1. Humoral (antibody-mediated) immunity: – Antibodies are chemicals found in the humors (fluid) of the body…produced by B lymphocytes 2. Cellular (cell-mediated) immunity: – The lymphocytes themselves…T lymphocytes – Before we get into more details of each of these two arms let’s look at the major cells involved. Specific Body Defenses Lymphocytes: arise from hematocytes • T cells become immunocompetent in the thymus (cell-mediated) • B cells become immunocompetent in the bone marrow (antibody-mediated) • Immunocompetent = becoming competent or capable of responding to a specific antigen by bonding to it. Specific Body Defenses Specific Body Defenses Lymphocyte • Immunocompetent lymphocytes are antigen specific which means they can attach to one and only one antigen. • “It is our genes, not antigens, that determine what specific foreign substances our immune system will be able to recognize and resist.” • They migrate through the lymph and blood system and “hide and wait” where they may or may not be used. Specific Body Defenses Macrophages: arise from monocytes • work in one of three ways… 1. Put fragments of engulfed antigens on their membrane to help T cells recognize them. 2. Secrete proteins called monokines that stimulate T cells and cause fever. 3. Become “killer macrophages” via T cell activation. Specific Body Defenses Back to the two types of immune responses… 1. Humoral (antibody-mediated) immunity: – Antibodies are chemicals found in the humors (fluid) of the body…produced by B lymphocytes 2. Cellular (cell-mediated) immunity: – The lymphocytes themselves…T lymphocytes Specific Body Defenses Primary humoral response (AKA Cloning) 1. Antigen binding activates B cells. 2. Clonal selection: rapid multiplication of the cell with the same antibody on its surface. 3. Most cells lose their membrane antibodies* to become plasma cells that die within a few days. 4. Some cells keep their membrane antibodies to become memory cells that live forever (almost). Specific Body Defenses Secondary humoral response 1. Memory cells await another meeting with the same antigen. 2. The same steps happen, but… 3. The next meeting is faster, longer lasting, and much more effective (often you don’t even know you have been infected again). See page 382 & 383 Specific Body Defenses • Active and passive humoral immunity 1. Active immunity a. Naturally acquired via bacteria/virus b. Artificially acquired via vaccine 2. Passive immunity a. Naturally acquired via mother and child b. Artificially acquired via immune serum or gamma globulin. Specific Body Defenses Vaccines • Keep us from experiencing the trauma of the disease. • Boost the secondary immune response Specific Body Defenses • Immune serum is used as… – Antivenom (snake venom) – Antitoxin (tetanus) – Antirabies serum – Monoclonal antibodies – commercially prepared antibodies used for treating cancer, diagnosing pregnancy, hepatitis, rabies and Specific Body Defenses Antibodies (immunoglobulins or Igs) • Soluble proteins secreted by B cells and bind with specific antigens. • There are 5 classes of Igs • Two identical halves Antibody/Antigen Complex Immunoglobin Classes: MADGE Immunoglobin Classes (p386) • IgM: (pentamer) first to be released in primary response • IgA: (dimer) protects mucus lining from pathogens • IgD: (monomer) activates B cells • IgG: (monomer) major participant in primary and secondary response; crosses placenta • IgE: (monomer) primary inflammatory and allergenic responder Antibody Functions 1. Complement fixation 2. Neutralization 3. Agglutination 4. Precipitation Antibody Function 1. Compliment fixation – Chief source of antibody used against cellular antigens (discussed in nonspecific body defenses pgs 376377) – Causes lysing of foreign cells via osmosis Antibody Function 2. Neutralization • Neutralizes viruses or bacteriotoxins by “hiding” them. • The antibodies surround the target. • This makes it easy pickings for macrophages. Antibody Function 3. Agglutination • Cross-linking of cell antibodies • Causes clumping of foreign cells • Seen mainly in blood transfusions • Macrophages can gobble them up easier Antibody Function 4. Precipitation • Same as agglutination, but instead of cross-linking cells it cross-links soluble proteins. • This makes them insoluble and precipitate out of solution • Now macrophages can slurp them up like frosting! <3 Specific Body Defenses Back to the two types of immune responses… 1. Humoral (antibody-mediated) immunity: – Antibodies are chemicals found in the humors (fluid) of the body…produced by B lymphocytes 2. Cellular (cell-mediated) immunity: – The lymphocytes themselves…T lymphocytes Specific Body Defenses Cell-Mediated Immune Response • T cells • Can’t bind with antigens on their own. • They must be helped by macrophages via antigen presentation Specific Body Defenses Produces different types of mature T cells 1. Cytotoxic (killer) T cells: kill virus infected cells, cancer cells and graft cells by injecting toxins like perforin. 2. Helper T cells: “boss” lymphocytes 3. Suppressor T cells: suppress lymphocyte activities at the end of an attack. 4. Delayed hypersensitivity T cells: major player in cell-mediated allergy and chronic inflammation. (IgE is the antibody-mediated counterpart) Organ Transplants/Rejection 1. Autografts: tissue grafts from the same person 2. Isografts: tissue grafts from an identical twin 3. Allografts: tissue grafts from an unrelated person (most common grafting) 4. Xenografts: tissue graft from another species (never successful-?-) Organ Transplant/Rejection Allografting is tricky… a. Match ABO blood group b. Match other blood antigens c. Match cell membrane antigens of the specific tissue being transplanted; must have at least 75% matching. d. Receiving immunosuppressive therapy treatments (severe side effects; easily mortally infected) Disorders of Immunity Three main types of immune disorders: • Allergies • Immunodeficiencies • Autoimmune disease Disorders of Immunity Allergies (“paranoia”) • Tissue damage caused by an overactive immune response of a “perceived” threat. • Allergen: “special” type of antigen • Two main types of allergic reactions – Immediate (acute) hypersensitivity – Delayed hypersensitivity Disorders of Immunity Immediate (acute) hypersensitivity • Antibody-mediated response (B cells) • IgE antibodies attach to mast cells (histamine holding cells) releasing histamines (inflammation). • Symptoms like: runny nose, watery eyes, bronchiole contraction • Use antihistamines to control. Disorders of Immunity Anaphylactic shock • Similar to immediate hypersensitivity, but more widespread and rapid. • Allergen is run through the blood stream (insect sting or bite, medicine like penicillin) • Epinephrine is used instead of antihistamine • Life threatening Disorders of Immunity Delayed hypersensitivity • Cell-mediated response (T cells) • After a few days cytotoxic T cells release lymphokines that cause skin irritations • Use corticosteroid drugs to control • Poison ivy, smellies, ect. Disorders of Immunity Immunodeficiencies • Low immune function • Examples include: – Severe combined immunodeficiency disease (SCID) where the immune system is so compromised even the slightest disease is a killer… bubble kid syndrome. – Acquired immune deficiency syndrome (AIDS) where HIV attack Helper T cells to compromise the immune system. Disorders of Immunity Autoimmune disease • The immune system goes rogue, attacking self-antigens as well as foreigners; this causes damage to tissues. • Examples include (p396): – – – – Multiple sclerosis Juvenile diabetes Lupus Rheumatoid arthritis