* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biochi~ic~a - ScienceDirect
Survey
Document related concepts
Transcript
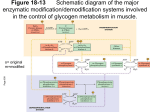
BiBBochi~ic~a i~ll!t'~l.' II et Biophysica A~ta ELSEVIER Biochimica et Biophysica Acta 1272 (1995) 1-13 Review McArdle's disease-muscle glycogen phosphorylase deficiency Clare Bartram a,*, Richard H.T. Edwards b, Robert J. Beynon a a Department of Biochemistry and Applied Molecular Biology, UMIST, PO Box 88, Manchester M60 IQD, UK b . . Department of Medwme, Universi~ of Liverpool, PO Box 147, Liverpool 1.,69 3BX, UK Received 13 February 1995; accepted 23 February 1995 Keywords: Glycogen phosphorylase; M c A r d l e ' s disease; Muscle glycolysis Contents I. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1.1. Discovery and history of the first defect in muscle glycolysis . . . . . . . . . . . . . . . . . . . . . . . 1.2. Identification of the enzyme defect . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1.3. Glycogen phosphorylase . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Isozymic forms of glycogen phosphorylase . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Activation of muscle glycogen phosphorylase . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Pyridoxal 5' phosphate . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2 2 2 2 2 2 3 2. Clinical presentation in M c A r d l e ' s disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.1. Symptomatology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.2. The 'second wind' phenomenon . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.3. Clinical heterogeneity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.4. Histology and the diagnosis of M c A r d l e ' s disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.5. Exercise analysis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 3 3 3 3 4 3. Glycogen utilisation in skeletal muscle . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3.1. Induction of glycogen breakdown during exercise . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3.2. Correlation of symptomatology with an absence of muscle glycogen phosphorylase . . . . . . . . . . . 3.3. Other biochemical effects of the glycogen block . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 4 4 4 4. Molecular pathology of M c A r d l e ' s disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.1. Molecular phenotypes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2. Muscle glycogen phosphorylase gene . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.3. Mutational analysis of M c A r d l e ' s disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.4. Effect of mutations on molecular phenotypes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5 5 5 7 7 5. Clinical management and therapy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.1. Exercise management . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.2. Dietary management . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Carbohydrate supplementation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Fatty acid supplementation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A m i n o a c i d / p r o t e i n supplementation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Vitamin B-6 supplementation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.3. Gene therapy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . * Corresponding author. Fax: + 4 4 161 2360409. 0 9 2 5 - 4 4 3 9 / 9 5 / $ 0 9 . 5 0 © 1995 Elsevier Science B.V. All rights reserved SSDI 0 9 2 5 - 4 4 3 9 ( 9 5 ) 0 0 0 6 0 - 7 9 9 9 9 9 9 10 11 C. Bartramet al. / Biochimicaet BiophysicaActa 1272 (1995) 1-13 Acknowledgements. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11 References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . lI 1. I n t r o d u c t i o n 1.1. Discovery and history of the first defect in muscle glycolysis In 1951, Dr. Brian McArdle reported physiological studies of a patient who presented with an 'exercise intolerance' [1]: " F o r as long as the patient could remember, light exercise of any muscle had always led to pain in the muscle and, if the exercise were continued, to weakness and stiffness." [1] In contrast to a normal individual, this patient failed to produce a rise in blood lactate in response to ischaemic forearm exercise. This suggested that there was a block in the glycolytic pathway preventing the breakdown of glycogen to lactate. It was inferred that skeletal muscle alone was affected because the normal hyperglycaemic response to adrenaline indicated that liver glycogen was broken down to glucose. Additionally, normal glycolysis was seen in blood cells [1]. 1.2. Identification of the enzyme defect It was not until 8 years later that the defect in glycolysis was identified [2,3]. The alleviation of the symptoms of this disorder by glucose suggested that the metabolic block occurred early in the glycolytic pathway. This was subsequently confirmed by the absence of glycogen phosphorylase activity in powdered muscle from a patient and similarly, by a lack of histochemical staining for activity in a muscle biopsy [2]. In another study, the addition of crystalline phosphorylase to a muscle homogenate from an affected individual resulted in a 3-fold increase in lactate production, whereas no lactate was generated in the absence of exogenous phosphorylase [3]. McArdle's disease was thus identified as a lack of muscle glycogen phosphorylase. It has subsequently been classified as Glycogen Storage Disease Type V (GSD V). 1.3. Glycogen phosphorylase Glycogen phosphorylase (1, 4-a-D-glucan: orthophosphate a-D-glucosyltransferase, E.C. 2.4.1.1) catalyses the phosphorolytic cleavage of glycogen to glucose-l-phosphate at a-l, 4-glycosidic linkages. This glucose-l-phosphate enters the glycolytic pathway to generate ATP with the concomitant formation of pyruvate or lactate. However, glycogen phosphorylase cannot completely degrade glycogen to its constituent glucose units and a second enzyme, debrancher enzyme, is required for the cleavage of a-1, 6-glycosidic linkages which form the branch points in the glycogen molecule. The combined action of these enzymes results in approx. 93% glucose-l-phosphate and 7% glucose. Isozymic forms of glycogen phosphorylase Glycogen phosphorylase has three isozymic forms: these are known as the muscle, liver and brain isozymes. The muscle form has been assigned to the long arm of chromosome 11 by high resolution chromosome sorting and DNA spot-blot analysis [4]. The liver form is encoded on chromosome 14 [5] and the brain form maps to chromosome 20 and to an homologous sequence on chromosome 10 although it is not known whether the latter is an expressed gene or a pseudogene [6]. There is a high degree of homology between the amino acid sequences of the three isozymes of glycogen phosphorylase [6] and in particular, residues involved in the activity of these enzymes are highly conserved [7]. This homology at the amino acid level is reflected in the nucleotide sequences. However, both the amino acid and nucleotide sequences of the muscle and brain forms show greater similarity to each other than to the liver sequences [6]. Although the three isozymes of glycogen phosphorylase are highly conserved, each is generally more similar to its corresponding isozyme in another species than to the other isozymes in the same species [8] and each has a distinct physiological role. The muscle isozyme provides ATP for muscle contraction whereas the liver form has a homeostatic function in the regulation of glucose release from hepatic glycogen stores. The brain isozyme is thought to provide an emergency supply of glucose during periods of anoxia or hypoglycaemia [8]. As their different functions would imply, isozymic expression of phosphorylase is tissue-specific and the brain, liver and muscle isozymes are the major forms expressed in the brain, liver and skeletal muscle, respectively. Expression in other tissues varies between species but in man, the liver form predominates; the muscle isozyme is found only in skeletal muscle, heart and possibly as a hybrid in brain [9]. It is thought that the brain isozyme is the foetal form of phosphorylase and that this is completely or partially replaced during development by the liver and muscle isozymes. This isozyme-switching during development is seen in rats [10] and in human skeletal muscle [11]. However, northern blot analysis of phosphorylase mRNA from a 24 week old human foetal liver indicated that the liver transcript predominated in this tissue and only low levels of brain mRNA were seen [6]. Activation of muscle glycogen phosphorylase Glycogen phosphorylase exists as a dimer of identical 97 kDa subunits. There are two forms of glycogen phos- C. Bartramet al. / Biochimica et BiophysicaActa 1272 (1995) 1-13 phorylase: phosphorylase a (higher activity) and phosphorylase b (lower activity) and conversion from b to a can be achieved by phosphorylation of Ser-14 [12,13]. Phosphorylation of the muscle isozyme is under neural and hormonal control. Neural control is mediated by calcium flux via calmodulin. Calcium ions released from the sarcoplasmic reticulum, upon initiation of muscle contraction, bind to the calmodulin y-subunit of phosphorylase kinase thus activating it. This enzyme phosphorylates glycogen phosphorylase resulting in more of the high-activity phosphorylase a and hence, glycogen breakdown is induced. Hormonal control of glycogen phosphorylase activity is mediated via the glycogenolytic cascade in response to adrenaline which activates the cAMP-dependent protein kinase. This enzyme activates phosphorylase kinase by phosphorylation and this in turn results in an increase in phosphorylase a. Glycogen phosphorylase is also a complex allosteric enzyme with two conformers: an active 'R' state and an inactive 'T' state and interconversion between these two states is via phosphorylation or binding of allosteric ligands at distinct sites on the enzyme. The muscle isozyme can be activated to 80% of its full activation capacity by AMP [8]. The phosphorylation site and the AMP binding site are in close proximity in the three-dimensional structure of the rabbit muscle isozyme and may activate the enzyme in the same way. Thus, the muscle isozyme is sensitive to both external signals and to changes in the concentrations of intracellular ligands which indicate the energy balance within the cell. Pyridoxal 5' phosphate Each subunit of the phosphorylase dimer binds, in a tight complex, one molecule of the cofactor pyridoxal-5'phosphate [14] to an active site lysine residue (Lys-680 in rabbit muscle phosphorylase) via a Schiff base. The cofactor is known to play a role in catalysis and although the proposed mechanism is not conclusive, it is thought that it serves as a proton donor and also has a role in maintaining the correct electrostatic environment of the catalytic site [15]. 3 myoglobinuria may result and this can cause renal failure [17,18]. Symptoms are typically less severe during childhood and as a consequence, the disease is often not recognised until individuals reach their second or third decade of life (Section 5.1). However, patients frequently recall incidences during childhood when they had problems with exercise although, at the time, a clinical disorder was not suspected. 2.2. The 'second wind' phenomenon Patients frequently find that they can continue to exercise with increased endurance if they rest briefly at the first signs of muscle pain. This is termed the 'second wind' phenomenon [19] and it is attributed to either a shift in a metabolic pathway or to a circulatory adjustment which results in enhanced peffusion of intramuscular capillaries [19-21]. The metabolic shift is facilitated by mobilisation of reserves, such as fatty acids [20,21]. This phenomenon has latterly been studied by 31P-NMR techniques [22,23] and it is clear, although not always feasible, that increasing the availability of substrate can improve exercise tolerance (Section 5.2). 2.3. Clinical heterogeneity In addition to the normal clinical picture of McArdle's disease, a number of atypical presentations have been described. These include: a very mild form of the disease with symptoms such as excessive tiredness and poor stamina [16]; a late-onset form of the disease ( > 40 years old) in which no exercise-induced symptoms were noted previously [24-27]; a fatal infantile form which is characterised by progressive weakness soon after birth and severe breathing difficulties followed by death before 4 months, as seen in two sisters [28,29]. An unrelated infant also exhibited this form of the disease but died at 16 days [30]; mild congenital weakness seen in a 4 year old boy [31]; exercise-induced myoglobinuria in an 8 year old boy with no previous history of exercise intolerance [32]; an attack of myoglobinuria in a 42 year old man which was apparently unrelated to a triggering effect. The second episode of myoglobinuria resulted in severe renal failure [33]. 2. Clinical presentation in McArdle's disease 2.4. Histology and the diagnosis of McArdle's disease 2.1. Symptomatology McArdle's disease is characterised by myalgia, severe cramps, early fatigue and muscle weakness brought on by exercise, although the severity of the symptoms does vary between individuals. Progressive weakness of the muscle may occur later in life. Patients are generally most affected by either high intensity exercise of short duration, such as sprinting or carrying heavy loads, or by less intense but sustained activity, such as walking uphill or riding a bicycle [16]. If exercise is continued once pain occurs, McArdle's disease is typically diagnosed by negative histochemical staining for phosphorylase activity in a muscle biopsy [34]. This stain relies on the ability of phosphorylase to work in the reverse direction and synthesise glycogen from glucose-l-phosphate -the newly formed glycogen is detected by an iodine stain. Added insulin, AMP (activators) and glycogen (primer) enhance the reaction to the extent that even low levels of phosphorylase activity result in a deep blue stain. In the absence of phosphorylase activity, the section remains brown. In a 4 C. Bartram et al./Biochimica et Biophysica Acta 1272 (1995) 1-13 biopsy from McArdle's patients, the muscle fibres do not usually take up stain but the smooth muscle of the intramuscular blood vessels does stain. In addition, McArdle's patients often show subsarcolemmal deposits of glycogen which can be detected with periodic acid-Schiff (PAS) stain on a portion of a muscle biopsy. These increases are typically 3-5-fold compared to the glycogen content of normal individuals. 2.5. Exercise analysis Although histochemical staining of a muscle biopsy from patients is the most reliable method for the diagnosis of McArdle's disease (Section 2.4), the ischaemic forearm test may also be performed on patients. This test is based on the failure of blood lactate levels to rise in McArdle's disease in response to exercise (Section 1.1). However, this test is not specific for glycogen phosphorylase and may indicate a block in another enzyme of the glycolytic pathway. Muscle cell membrane damage frequently occurs in McArdle's patients due to over-exertion of the muscles and this releases intracellular components into the circulation. The most significant of these is myoglobin (Section 2.1) but creatine kinase activity is almost always raised in the plasma of McArdle's patients. In addition to the release of these intracellular contents, acute local muscle damage appears as a painful hardening and shortening of the muscle. This contracture is electrically silent indicating that it is not caused by active contraction of the muscle fibres. It could be due to the same kind of failure of actin-myosin crossbridge relaxation as is known to occur in 'rigor mortis' when intramuscular ATP is depleted [35]. However, needle biopsy studies have shown that the muscle content of phosphocreatine is not depleted when the muscle is fatigued [36] and this has been confirmed by 31P-NMR [37]. Leakage of potassium is also consequential to muscle damage. During whole body exercise, the large increases in the plasma potassium concentration offers a possible explanation of the cause of fatigue [38]. Induction of fatigue by electrical stimulation showed that muscle of a McArdle's patient was more fatiguable than that of a normal individual and this was attributed in part to 'fading' of the muscle action potential [39-41] and partly to myofibrillar activation failure [42]. tion is of limited use during intense exercise because the circulation cannot provide substrates (fatty acids and carbohydrates) and oxygen quickly enough to meet the energy demands [19]. Muscle glycogen phosphorylase breaks down glycogen to glucose-l-phosphate which enters the glycolytic pathway to generate ATP with the formation of pyruvate and, under anaerobic conditions, lactate. Use of glycogen for glycolysis instead of intracellular glucose results in greater net ATP generation and delays muscle fatigue [44]. 3.2. Correlation of symptomatology with an absence of muscle glycogen phosphorylase Due to a lack of muscle phosphorylase activity, McArdle's patients cannot mobilise their muscle glycogen stores. Therefore, depletion of intracellular glucose and ATP, during the first few minutes of exercise, results in onset of symptoms. To exacerbate the situation, oxidative phosphorylation is impaired in patients due to an abnormally low substrate flux through the TCA cycle. This is probably because the virtual absence of pyruvate from glycolysis is likely to reduce the rate of acetyl-CoA formation and this affects the TCA cycle [23,45]. Acetyl-CoA can be generated from the breakdown of fatty acids but unless trained, most individuals have a limited capacity for fatty acid oxidation during exercise. This decline in oxidative phosphorylation results in a decreased oxygen consumption in patients [23] and in fact, maximal oxygen uptake into McArdle's muscle is 35-50% of normal values [46]. In addition, McArdle's patients exhibit a disproportionate increase in heart rate and ventilation rate compared to normal individuals [21,23]. 3.3. Other biochemical effects of the glycogen block The absence of glycolysis and reduction in oxidative phosphorylation in McArdle's patients means that increased reliance is placed on the creatine kinase and adenylate kinase reactions. Both reactions regenerate ATP very rapidly to provide an immediate short-term source of energy [47]. The action of these enzymes in combination with decreased ATP generation from carbohydrate and fatty acids results in increased levels of ADP and AMP within the muscle. This affects normal metabolism of adenine nucleotides resulting in excessive purine degradation [48,49]: 3. Glycogen utilisation in skeletal muscle ATP ~ 3.1. Induction of glycogen breakdown during exercise In the resting state, fatty acid oxidation predominates in the skeletal muscle of normal individuals but during exercise, the energy requirements are largely met by glycogen breakdown and anaerobic glycolysis [43]. Aerobic oxida- ADP ",~ "" AMP - - ~ ~ ~ Inosine ~ Hypoxanthine NH3 Inosine, hypoxanthine and ammonia enter the bloodstream and elevated plasma levels of all three have been detected in some McArdle's patients following exercise C. Bartram et al. / Biochimica et Biophysica Acta 1272 (1995) 1-13 [48-50]. However, excessive release of hypoxanthine and inosine has not been observed in all McArdle's patients [51,52]. Elevated ammonia output is seen consistently but cannot be solely attributed to purine nucleotide degradation use of amino acids as an alternative energy source in McArdle's muscle also releases ammonia into the bloodstream (Section 5.2.). McArdle's patients also show an enhanced response to various hormones compared to normal individuals which helps to minimise the effect of the glycolytic block. Neural feedback from working muscle causes an increase in the concentrations of growth hormone, cortisol, noradrenaline, adrenaline and adrenocorticotrophic hormone and a decrease in insulin concentration which results in mobilisation of extramuscular fuel, such as glucose and free fatty acids, to meet the energy requirements of the muscle [53]. 4. Molecular pathology of McArdle's disease 4.1. Molecular phenotypes McArdle's disease is characterised by an absence of functional muscle glycogen phosphorylase but patients show heterogeneity in their protein and mRNA expression (Table 1). The majority of McArdle's patients do not have detectable muscle glycogen phosphorylase [54-61]; of 93 patients, only 13 expressed low levels of protein [54,57-61] and a further two expressed inactive protein [55,61]. Of 22 patients whose mRNA has been determined, twelve lacked detectable mRNA [54,57,59] whereas nine expressed the 3.4 kb phosphorylase mRNA at normal [59,61] or reduced levels [56]. Another patient expressed a truncated form (1.2 kb) of the transcript [61]. Bidimensional protein maps of muscle extract from three McArdle's patients identified potential degradative intermediates of phosphorylase. Mus- 5 cle phosphorylase (molecular mass 97 kDa) was not seen but two spots with molecular masses 60 kDa and 70 kDa were detected. However, these two spots were not recognised by antibodies to phosphorylase [62]. These spots may be completely unrelated to phosphorylase or alternately, the antibodies may have been sensitive to a conformational epitope that was altered by misfolding or by sample preparation. 4.2. Muscle glycogen phosphorylase gene Although there have been a number of studies on the molecular phenotypes of McArdle's patients, until recently, nothing was known of the mutations causing the disease. The human muscle glycogen phosphorylase gene is approx. 14 kb [63]. Sequencing of the 5' region identified several promoter regions [11] including a TATA-Iike homology, TTTAAA, located at position - 2 9 (based on the designation of the transcription start site as + 1) and a potential CAAT box, CCAAGAC, at - 8 0 . There is a region at - 5 9 2 with the sequence CTCCAAAAGG which is necessary for efficient transcription of the phosphorylase gene. This sequence superficially resembles the CArG motif CC(A/T)rGG present in the promoter regions of skeletal and cardiac muscle a-actin genes and has been implicated in their tissue-specific expression [64,65]. It is repeated at - 2 5 2 in the 5' region of the phosphorylase gene, but expression studies indicate that this later sequence is not necessary for transcription so sequence context may be critical [11]. Even before the elucidation of the mutations causing McArdle's disease, it was generally held to be an autosomal recessive disease [66,16]. Autosomal dominant inheritance was suggested in a family in which four generations were reportedly affected with McArdle's disease [67]. However, the disease was only confirmed in two individu- Table 1 Molecular phenotypes in McArdle's patients Molecular phenotypes [54] No protein, no mRNA No protein, normal mRNA No protein, decreased mRNA No protein, truncated mRNA No protein, mRNA n.d. Decreased protein, normal mRNA Decreased protein, mRNA n.d. Normal levels of inactive protein 2 Total number of patients [55] [56] [57] [58] 5 [59] [60] 5 3 [61 ] 1 3 5 2 2 2 2 4 I 2 3 6 2 1 2 1 1 9 3 10 11 3 1 39 1 5 1 48 The column headings indicate the citations from which the information was obtained. n.d. = not determined. A number of studies have focused on expression of muscle phosphorylase protein and mRNA in McArdle's patients [54-61]. This has demonstrated the heterogeneity in the molecular phenotypes of patients with the same clinical condition. There is much more information available on the expression of phosphorylase protein than on mRNA expression. The majority of patients do not express protein at all but of those that do, the protein is generally present at very low levels. Normal levels of phosphorylase protein are seen in two patients but in both cases, the protein is inactive or virtually inactive [55-61]. 6 C. Bartram et al./Biochimica et Biophysica Acta 1272 (1995) 1-13 1844+ 1G->A NcoI L291P SacI 122G-> "IT t'N\\\lll llHH R49X N l a 111 II • Ill 1606delG AF708/709 I 1 nl m nm nnn / nit niL.~ K542T MaeII G204S HaeBI 77A->C MallI Key: Untraml~ted regions Exons Introns Mutation Base change Exon Effect of mutation R49X CGA->TGA 1 Nonsense 77A->C ATG->CTG 1 Missense 122G->TT G->TT 1 Frameshift G204S GGC->AGC 5 Missense L291P CTG->CCG 8 Missense 1606delG GAG->GA 13 Frameshift K542T AAG->ACG 14 Missense 1844+ 1G->A G->A '14' AF708/709 ATTC 17 Abnormal splicing Amino acid deletion Fig. 1. Sites of mutation and their detection in the muscle phosphorylase gene. At present, there are nine known mutations across the muscle phosphorylase gene which cause McArdle's disease [71,72,74-77]. The rapid diagnosis of some of these mutations is facilitated by digestion of a PCR product with the restriction enzyme indicated. The G204S mutation disrupts a recognition site for HaelII but all the other mutations create an extra restriction site and so an additional band results from digestion with the enzyme. Rapid detection of 1844 + 1G --* A is dependent upon the introduction of a base change into the PCR product by a primer which binds adjacent to the possible site of mutation; in the presence of the mutation, the mismatch primer creates a recognition site for NcoI. The effects of each mutation are shown in the table. Note: Mutation 1844 + 1G ~ T has previously been defined as 1778de167 [109] but whilst a deletion of 67 bp in the transcript does result from this mutation, the primary defect is in fact alteration of the consensus splice site sequence and so the nomenclature has been reviewed. C. Bartram et aL / Biochimica et Biophysica Acta 1272 (1995) 1-13 als from two generations and a dominant mechanism of inheritance in this family is questionable. In most cases, heterozygous carriers for McArdle's disease are unaffected because it seems that one normal allele of the muscle phosphorylase gene is adequate for normal levels of the protein. However, there are a number of reports of manifesting heterozygotes who do have phosphorylase activity upon histochemical staining but who show clinical symptoms of McArdle's disease [68,69]. A threshold value of 2 0 - 4 5 % of normal has been suggested to be the minimum activity below which symptoms occur [69] although assignment is tentative. [74]. Again the truncated peptide would probably be unstable and therefore, rapidly degraded. There are four missense mutations and a single amino acid deletion which may have functional or structural consequences on muscle glycogen phosphorylase (Section 4.4). The G204S mutation occurs in a domain involved in glycogen binding whereas K542T affects the glucose-binding domain [72]. Both L291P and A F 7 0 8 / 7 0 9 may alter normal protein folding and possibly, intracellular stability [75]. The initial methionine codon is altered by the 77A --* C mutation thus abolishing translation initiation [76]. Another mutation ( 1 8 4 4 + I G ~ A ) alters the consensus splice site sequence at the 5' end of intron 14 and as a consequence, an alternative sequence in exon 14 is used. This results in abnormal splicing which produces a 67 bp deletion in the transcript. The resulting shift in the reading frame generates a short sequence of missense polypeptide containing 14 amino acids before translation is prematurely terminated after 580 amino acids [75]. Another frameshift is caused by the deletion of a single base in codon 509 (1606delG) and this again results in premature termination of translation, this time after 536 amino acids [77]. The allele frequencies of the above mutations are shown in Table 2. 4.3. Mutational analysis o f McArdle's disease Initial work focused on restriction fragment length polymorphism of the muscle phosphorylase gene of McArdle's patients but met with little success [56,61]. The muscle phosphorylase gene is notable for its lack of polymorphisms and restriction enzyme analysis with 94 enzymeprobe combinations in 20 unrelated patients revealed just a single polymorphism at a CpG site associated with McArdle's disease [70]. This analysis did, however, preclude the possibility of gene deletions greater than 100 bp. Since these initial studies, sequencing has revealed a number of mutations in the muscle phosphorylase gene which cause McArdle's disease (Fig. 1). The most common base change is a nonsense mutation [71,72], designated R49X (nomenclature proposed in Ref. [73]). This results in premature termination of translation; the resulting truncated peptide is so short that it is non-functional and probably rapidly degraded. A second mutation in exon 1, 122G ~ TT, shifts the reading frame such that a short sequence of missense protein containing 11 amino acids is synthesised before translation is prematurely terminated N M5 M6 M2 N M7 N 7 4.4. Effect o f mutations on molecular phenotypes The R49X mutation occurs in the coding region of the muscle phosphorylase gene and causes premature termination of protein translation. However, of the patients whose biochemical phenotype is known, all those homozygous for the R49X mutation have no detectable m R N A on northern blots (Fig. 2). Therefore, premature termination of protein translation affects the stability of the m R N A [71,72] and there are a number of precedents for this in other M8 M1 M3 M4 M9 N 3.4kb phosphorylase mRNA Mutation analysis __+ R49X R49X R49X +_ R49X + ? R49X R49X + R49X + R49X R49X n.d. Rg9X R49X + + ? 122G->TT ? R49X + K e y : N = normal individual M1-9 = McArdle's patients [numbering as in ref. 71] +/+ = normal sequence i.e. no mutations n.d. = not determined Fig. 2. Comparison of northern blot analysis and mutational analysis. Northern blot analysis has shown heterogeneity in the expression of phosphorylase mRNA in McArdle's patients [59]. Correlation of this information with the mutation analysis for these patients [71,74] shows that those individuals who are homozygous for the R49 × mutation lack detectable mRNA. Therefore, a premature termination codon in the muscle phosphorylase gene not only affects protein synthesis but decreases transcript stability. However, detectable mRNA is seen with individual M1 although premature termination of translation also occurs from both alleles in this individual. (Reprinted from 'McArdle's disease: molecular genetics and metabolic consequences of the phenotype' by R.J. Beynon et al. in Muscle and Nerve. Copyright: 1995, John Wiley and Sons, Inc.) 8 C. Bartram et al./Biochimica et Biophysica Acta 1272 (1995) 1-13 Table 2 Allele frequency of the mutations causing McArdle's disease Mutation Allele frequency in European population [71,74,109] Allele frequency in USA and Japanese population [72,75-77] R49X 77A ~ C 122G ~ TT G204S L291P 1606delG K542T 1844+1G ~ A AF708/709 46 0 1 2 0 n.d. 0 0 n.d. 5l 1 n.d. 8 1 2 3 1 7 n.d. = not determined. The most common mutation is R49X which is present in 46 out of a total of 76 available alleles from European McArdle's patients, The majority of these patients are Caucasians although there are a number of patients whose ethnic origins are not known. The USA patients are Caucasian and R49X is the predominant mutation in these patients. However, the AF708/709 mutation has only been found in Japanese patients (7 out of 14 alleles) suggesting that this might be a common mutation in this population. None of the Japanese patients carry R49X and so, it would appear that McArdle's disease has occurred independently in these two populations. The other mutations are much less frequently observed. diseases. For example, decreased stability of the transcript in response to premature termination of translation occurs in human /3-globin mRNA as illustrated by the /30 thalas- saemias [78-81], mRNA of cystic fibrosis transmembrane conductance regulator which is implicated in cystic fibrosis [82] and mRNA of human /3-hexosaminidase A which is defective in Sandhoff disease [83]. Patient M 1 carries the R49X mutation on one allele of the muscle phosphorylase gene and the 122G ~ TT on the other, both of which cause premature termination of translation. However, this individual does seem to express low levels of mRNA as seen by northern blot analysis (Fig. 2) which is unexpected given that termination of translation in exon 1 occurs from both alleles. The mechanism by which mRNA stability could be differentially affected by these two different mutations is not clear but it is possible that the mRNA carrying the frameshift mutation is not translatable. Degradation of aberrant transcripts is thought to be co-translational [84], such that a complete inability to translate the mRNA would cause it to have increased stability. Analysis of molecular phenotypes of patients has suggested that the missense mutations destabilise the protein [75]. Rabbit muscle glycogen phosphorylase remains the only isozyme for which the three-dimensional structure has been determined and thus the structural interpretation of amino acid changes must be based upon this protein. The overall amino acid sequence identity for rabbit and human muscle phosphorylase is 97% and there is no variation in any catalytic or allosteric sites [63,85]. All three of the G204S L29 IP I Human muscle Rabbit muscle Rat muscle Human liver Rat liver Human brain Rat brain Yeast Potato type H VHFYGHVEH VHFYGRVEH VHFYORVEH VHFYGKVEH VHFYGRVEH VHFYGRVEH VHFYORVEH VTFYGYVDR IRFFGHVEV I Human muscle Rabbit muscle Rat muscle Human liver Rat liver Human brain Rat brain Yeast Potato type H K542T KQENKLKFA KQEN]KLKFA KQENKLKFS KQENKLKFS KQENKLKFS KQENIKLKFS KQENKLKFS KLNNI~IRLV KMANKQRLA EGKELRLKQ EGKELRLKQ EGKELRLKQ EGKELRLKQ EGKELRLKQ EGKELRLKQ QGKELRLKQ NGKLLRLKQ AF'/08/709 I Human muscle Rabbit muscle Rat muscle Human liver Rat liver Human brain Rat brain Yeast Potato type H EGKELRLKQ I Human muscle Rabbit muscle Rat muscle Human liver Rat liver Human brain Rat brain Yeast Potato type H GEENFFIFG GEENFFIFG GEDNFFIFG GEENLFIFG GEENLFIFG GAENLFIFG GEENLFIFG GEDNVFLFG GEDNFFLFG Fig. 3. Sequence conservation at the sites of mutation in McArdle's disease. The above figure shows short segments of the amino acid sequence alignments for nine glycogen pbosphorylases [7] in the vicinity of the G204S, L291P, K542T and AF708/709 mutations. The mammalian sequences include liver, brain and muscle isozymes from human and rat plus the muscle isozyme from rabbit. Yeast phosphorylase and potato phosphorylase type H are shown to indicate the high degree of sequence conservation even in non-mammalian phosphorylases. All three missense mutations occur at a position at which there is absolute conservation of the amino acid between the nine sequences. Both pbenylalanine residues in the region 708/709 are highlighted, because the codons are the same and it is not possible to be more specific about the deletion. c. Bartram et al. / Biochimica et Biophysica Acta 1272 (1995) 1-13 9 missense mutations (G204S, L291P and K542T) change a highly conserved amino acid (Fig. 3). The sequence conservation is such that the amino acid at these positions remains unchanged across the species [7] including two non-mammalian phosphorylases (yeast and potato type H). This suggests that each of these amino acids is critical for the normal function of glycogen phosphorylase; their alteration could decrease the activity or the stability of the mutant protein. There is also strong conservation in the region of the AF708/709 mutation (Fig. 3). creased by heparin [21], noradrenaline [20,21] or by infusion of emulsified fat, particularly in combination with glucose [19]. The same effect was produced by fasting which increases plasma concentrations of free fatty acid [91]. However, a high fat diet gave more variable results because one patient reported no beneficial effect [89] whereas another noted subjective improvement after 3 days although there was no increase in measured muscle strength [92]. The benefits of a high fat intake on muscle performance must be weighed up against the potentially detrimental effect on an individual's long-term health. 5. Clinical management and therapy Amino a c i d / p r o t e i n supplementation 5.1. Exercise management Exercise management and weight control have an important role to play in the management of McArdle's disease. Weight determines oxygen consumption during walking, especially when walking uphill. It is therefore advantageous for a patient with McArdle's disease to avoid excess weight. Patients should also try to keep active within the capability of their muscles as reduced activity in patients with muscle disorders can diminish the mitochondrial function in muscle [86]. The greater the mitochondrial oxidative capacity, the less dependent an individual is on glycogenolysis. Children are more active than adults with a higher aerobic capacity per kilogram body weight [87] and this may explain why McArdle's disease is usually not diagnosed in young children. 5.2. Dietary management The aim of any current therapy for McArdle's disease is to enable patients to exercise with increased tolerance and to prevent the occurrence of muscle damage or myoglobinuria which can lead to renal failure. The provision of alternative or additional energy fuels to the skeletal muscle can accelerate the onset of the 'second wind' phenomenon and thus alleviate glycolytic deprivation. Carbohydrate supplementation Glucose infusion enables patients to exercise with increased endurance [19,21,22,50] and prevents exercise-induced ATP degradation as measured by a decrease in the degradative metabolites [50] and by a decline in plasma ammonia [23]. Similarly, fructose infusion improves exercise endurance [ 19,21 ]. However, long-term oral administration of glucose or fructose has been largely unsuccessful in improving the exercise capabilities of patients [16,89]. Benefits are only seen when carbohydrate is given immediately before exercise and in practice, it is not always possible to predict a bout of exertion [90]. Fatty acid supplementation McArdle's patients could exercise with increased endurance when plasma levels of free fatty acid were in- There is evidence for increased utilisation of amino acids in skeletal muscle of McArdle's patients [52,93]. Therefore, provision of adequate amino acids by direct supplementation, or via a high protein diet might improve muscle function. This was confirmed in one patient whose protein intake was increased to 25-30% protein from 14% [94]. In a subsequent study, three patients were provided with branched chain amino acids in amounts calculated to exceed the levels expected from a high protein diet but none experienced either an immediate or long-term (1-2 months) subjective improvement or an objective benefit as assessed by their maximal strength and endurance [95]. The first step in amino acid catabolism is donation of the a-amino group to 2-oxoglutarate (a TCA cycle intermediate) in a transamination reaction which generates the cognate 2-oxo acid and glutamate. The 2-oxoglutarate may be regenerated by deamination with the release of ammonia. Alternately, a second transamination reaction with pyruvate regenerates 2-oxoglutarate and results in the corresponding formation of alanine. In the normal individual, alanine and glutamine (formed by the reaction of glutamate with ammonia) provide a mechanism for the elimination of nitrogen from the muscle and its transport to the liver for detoxification. However, in McArdle's disease, the supply of precursors for alanine and glutamine is compromised. In exercising McArdle's muscle, glycolytic flux is suppressed and it is unlikely that adequate pyruvate is synthesised to sustain the levels of alanine required for ammonia removal. Likewise, any reaction that drains TCA cycle intermediates, such as 2-oxoglutarate, would ultimately impair energy metabolism. Thus, a decreased ability to remove ammonia, in the form of alanine and glutamine might explain the elevated plasma ammonia levels during exercise in McArdle's disease [38]. These increased ammonia levels may be responsible in part for the muscle pain and fatigue [96]. The ability of glucose to diminish ammonia output by McArdle's muscle [23] is probably due to an increased supply of pyruvate which can be transaminated to alanine. Uptake and oxidation of the branched chain amino acids occurs in both normal individuals and at a higher rate in McArdle's patients during exercise [52]. Consistent with this suggestion is the observation of exercise-induced acti- 10 c. Bartram et al. / Biochimica et Biophysica Acta 1272 (1995) 1-13 vation of the branched chain 2-oxo acid dehydrogenase, the key enzyme in the oxidation of branched chain amino acids [97]. The complex was activated to a greater extent, and at a lower work load in McArdle's patients compared to normal individuals. Amino acid supplements (10 g each of leucine, isoleucine and valine) were initially given to patients prior to exercise in an effort to improve their performance. However, supplementation did not have the expected beneficial effect and in fact, exercise performance actually deteriorated [96]. This may be due to the increased ammonia resulting from transamination of these amino acids. Any benefits gained from branched chain amino acid oxidation must be offset against the additional nitrogen burden. In contrast, supplements of 10 g of the ornithine salts of the 2-oxo acids of leucine and valine (4-methyl-2-oxopentanoate and 3-methyl-2-oxobutanoate, respectively) and 5 g of the sodium salt of the 2-oxo acid of isoleucine (3-methyl-2-oxopentanoate), if given 20 min prior to exercise, improved exercise performance, resulted in smaller increases in heart rate and suppressed plasma ammonia output [38,96]. The 2-oxo acids provide an alternative energy source but they do not contribute to the nitrogen load of the muscle cells, sparing pyruvate and 2-oxoglutarate. If the supplements of 2-oxo acids were given 90 min prior to exercise, this beneficial effect was no longer seen [52] which may have been due to re-amination. The most consistent increase in endurance was achieved when the branched chain oxo acids were combined with 75 g glucose given orally 30 rain before exercise [38,96]. Uptake of alanine by exercising muscle was described in one McArdle's patient [93] although it is usually released from normal muscle. A later study with a number of McArdle's patients initially appeared to be at variance with this finding as alanine was released by muscle [52]. However, when the exercise protocols were examined in more detail, the two opposing results can be related to the work pattern (Fig. 4a). In both studies, similar total work was performed but in the earlier study, the work was gradually increased and so, it is likely that the patient actually reached the 'second wind'. It is possible to gain some insight into alanine metabolism by combining the information from these two studies although the conclusions should be treated with caution (Fig. 4b). Release of alanine from exercising McArdle's muscle peaks earlier, and total alanine output is lower than in normal individuals. This is consistent with an initially increased demand on pyruvate for transamination and a subsequent decrease in the pyruvate pool which cannot be replenished. It then appears that McArdle's muscle actually takes up alanine which may be driven by gluconeogenesis. However, the magnitude of alanine uptake into muscle is substantially lower than initial release. Amino acid supplementation may have a second effect on muscle protein metabolism. Increased oxidation of amino acids by skeletal muscle in McArdle's disease a) 8O 6O ~" 40 g' 20 0 0 20 40 60 80 Exercise duration (rain) b) 160 120 ~ Release 80 ~ 40 II 0 = -40 ~ -80 2 ~40 Time (rain) 60- 80 - -120 + Uptake - 160 l Fig. 4. Alanine fluxes in McArdle's disease. This figure collates the data from two studies on alanine flux in McArdle's disease. They used very different exercise protocols, which are illustrated in panel a. The study by Wagenmakers and colleagues (study I) [52] used short periods of higher intensity exercise, whereas that of Wahren and colleagues (study II) [93] was a longer duration, low intensity programme. The comparisons of the two protocols are approximate, and are based on our interpretation of the experimental details given. The data for alanine flux, obtained from both studies (including those from normal individuals), are placed on the same time scale, but must be interpreted in the light of the different exercise protocols. McArdle's patients, []; Normal individuals, I . might reduce their availability for the synthesis of new muscle protein [98] or elicit enhanced protein degradation. If this imbalance in protein turnover is prolonged it could ultimately lead to long term muscle wasting and weakness. Vitamin B-6 supplementation Glycogen phosphorylase requires PLP as a cofactor and apo-phosphorylase cannot be detected in skeletal muscle [99]. It is not clear whether this is due to a marked instability of apo-enzyme or whether the apo-enzyme has such a high affinity for its cofactor that it 'scavenges' PLP C. Bartram et al. / Biochimica et Biophysica Acta 1272 (1995) 1-13 from other body pools. However, because phosphorylase is such an abundant protein (2-5% of the total soluble protein in skeletal muscle), and because of the large mass of the musculature, 80% of the body pool of vitamin B-6 is attached to this enzyme [100]. We have used [G-3H] pyridoxine as a specific label for phosphorylase in vivo and have observed that the rate of loss of labelled PLP from the enzyme parallels the rate of phosphorylase degradation [101-103]. Therefore, release of PLP from phosphorylase is dependent on degradation of the protein [104]. Vitamin B-6 metabolism studies have consistently identified a large, slowly accessible vitamin B-6 pool in the body [105,106] which is undoubtedly muscle glycogen phosphorylase. The other body pools of vitamin B-6 appear to have a much higher turnover rate and are probably more readily depleted when vitamin B-6 intake is inadequate. In contrast, even extended periods of vitamin B-6 deprivation do not significantly diminish the adult muscle phosphorylase pool [107,108]. This has led to the suggestion that the daily vitamin B-6 requirements are different in growth and maintenance; during growth, vitamin B-6 is incorporated into the slow muscle phosphorylase pool, whereas in the adult, the daily requirement is that which is needed to sustain the fast pools [106]. We therefore propose that muscle phosphorylase could function as a 'buffer', compensating for day-to-day variation in dietary intake of vitamin B-6 in normal individuals. The majority of McArdle's patients lack muscle glycogen phosphorylase, which means that this slow pool of vitamin B-6 is absent and consequently, its 'buffering' capacity is lost. McArdle's patients may therefore be more reliant on a regular intake of vitamin B-6 and vitamin B-6 status, as assessed by an erthyrocyte transaminase assay, does seem to be compromised in some of our patients [109]. Furthermore, McArdle's patients may be more reliant on adequate vitamin B-6 compared to normal individuals because they are dependent on alternative energy pathways which require PLP. Aminotransferases play a key role in amino acid catabolism (Section 5.2.) and these enzymes are PLP-dependent. In addition, there is evidence that carnitine biosynthesis requires PLP. Carnitine is required to facilitate the transport of fatty acyI-CoA across the inner mitochondrial membrane prior to oxidation. Inadequate vitamin B-6 status results in reduced carnitine biosynthesis and as a consequence, reduced fatty acid oxidation [ 110]. We have postulated that the exercise performance of those McArdle's patients who lack glycogen phosphorylase protein might be improved by supplementation with relatively high daily doses (50 mg) of vitamin B-6 (the recommended daily dose for normal individuals is 2 mg). Vitamin B-6 supplementation did improve the muscle fatiguability of three McArdle's patients by increasing the force generation of the muscle [109]. This implies that i m p r o v e m e n t is due to an increase in fuel mobilisation/utilisation and the inference from this is that 11 the cofactor saturation of the aminotransferases in the muscles is improved. Supplementation of two patients with vitamin B-6 in earlier studies did not prove effective [ 18,11 1], but both patients had some phosphorylase protein on an SDS polyacrylamide gel. The presence of protein, albeit inactive, means that it could still function as a 'buffer' for PLP and vitamin B-6 supplementation may not be beneficial in these patients. Mild sensory neuropathy associated with vitamin B-6 overdosage is only seen at levels of 2 - 4 g / d over several months [112]. Therefore, vitamin B-6 at 50 m g / d may potentially improve the exercise capacity of the majority of McArdle's patients without having a detrimental effect on their health. In addition, as aminotransferases require PLP as a cofactor, we suggest that any increased protein or amino acid regimen must ensure that vitamin B-6 intake is adequate. If the activity of the aminotransferases is limited by inadequate PLP then the increased protein may have little benefit. 5.3. Gene therapy Interest is now being focused on gene therapy in the treatment of genetically inherited diseases. A recombinant adenovims has been used to drive expression of rabbit muscle phosphorylase cDNA in a C2C12 myoblast cell line [1 13]. Adenoviral delivery into myoblasts, which were subsequently induced to differentiate, resulted in a moderate and transient increase in phosphorylase activity. However, introduction into non-proliferating myotubes resulted in higher phosphorylase activity which was sustained over the period of the experiment (20 days). The heterologously expressed phosphorylase was subject to both hormonal and allosteric control which suggests that glycogen breakdown will occur in a regulated manner in the treated muscle of patients. It might be anticipated that when suitable delivery vehicles are developed for muscle, probably driven by other severe myopathies, such therapy in McArdle's disease will also be successful. Acknowledgements We would like to acknowledge The Muscular Dystrophy Group of Great Britain and Northern Ireland for their financial support. We would also like to thank the McArdle's patients, their families and our colleagues for their continuing contribution to this work. References [1] McArdle,B. (1951) Clin. Sci. 10, 13-33. [2] Mommaerts, W.F.H.M., Illingworth, B., Pearson, C.M., Guillory, R.J. and Serayolarian,K. (1959) Proc. Natl. Acad. Sci. USA 45, 791-797. [3] Schmid, R. and Mahler, R. (1959) J. Clin. Invest. 38, 2044-2058. [4] Lebo, R.V., Gorin, F., Fletterick,R.J., Kao, F.-T., Cheung, M.-C., Bruce, B.D. and Kan, Y.W. (1984) Science225, 57-59. 12 C. Bartram et al. / Biochimica et Biophysica Acta 1272 (1995) 1-13 [5] Newgard, C.B., Fletterick, R.J., Anderson, L.A. and Lebo, R.V. (1987) Am. J. Hum. Genet. 40, 351-364. [6] Newgard, C.B., Littman, D.R., Van Genderen, C., Smith, M. and Fletterick, R.J. (1988) J. Biol. Chem. 263, 3850-3857. [7] Hudson, J.W., Golding, B.G. and Crerar, M.M. (1993) J. Mol. Biol. 234, 700-721. [8] Newgard, C.B., Hwang, P.K. and Fletterick, R.J. (1989) Crit. Rev. Biochem. Mol. Biology 24, 69-99. [9] Proux, D. and Dreyfus, J.C. (1973) Clin. Chim. Acta 48, 167-172. [10] David, E.S. and Crerar, M.M. (1986) Biochim. Biophys. Acta 880, 78-90. [11] Lockyer, J.M. and McCracken, J.B. (1991) J. Biol. Chem. 266, 20262-20269. [12] Fischer, E.H. and Krebs, E.G. (1955) J. Biol. Chem. 216, 121-132. [13] Fischer, E.H., Graves, D.J., Crittenden, E.R.S. and Krebs, E.G. (1959) J. Biol. Chem. 234, 1696-1698. [14] Baranowski, T., Illingworth, B., Brown, D.H. and Cori, C.F. (1957) Biochim. Biophys. Acta 25, 16-21. [15] Johnson, L.N. (1992) FASEB J. 6, 2274-2282. [16] DiMauro, S. and Bresolin, N. (1987) in Myology (Engel, A.G. and Banker, B.Q., eds.), Vol. 2, pp. 1585-1601, McGraw Hill Book Company, New York. [17] Bank, W.J., Di Mauro, S. and Rowland, L.P. (1972) New Engl. J. Med. 286, 1102. [18] Grunfeld, J.P., Ganeval, D., Chanard, J., Fardeau, M. and Dreyfus, J.C. (1972) N. Engl. J. Med. 286, 1237-1241. [19] Pearson, C.M., Rimer, D.G. and Mommaerts, W.F.H.M. (1961) Am. J. Med. 30, 502-517. [20] Pernow, B.B., Havel, R.J. and Jennings, D.B. (1967) Acta Med. Scand. (Suppl.) 472, 294-307. [21] Porte, D., Crawford, D.W., Jennings, D.B., Aber, C. and Mcllroy, M.B. (1967) N. Engl. J. Med. 275, 406-412. [22] Lewis, S.F., HaUer, R.G., Cook, J.D. and Nunnally, R.L. (1985) J. Appl. Physiol. 59, 1991-1994. [23] Lewis, S.F. and Hailer, R.G. (1986) J. Appl. Physiol. 61,391-401. [24] Engel, W.K., Eyerman, E.L. and Williams, H.E. (1963) N. Engl. J. Med. 268, 135-137. [25] Felice, K.J., Schneebaum, A.B. and Jones, H.R. (1992) J. Neurol. Neurosurg. Psychiat. 55, 407-408. [26] Hewlett, R.H. and Gardner-Thorpe, C. (1978) S. Afr. Med. J. 53, 60. [27] Pourmand, R., Sanders, D.B. and Corwin, H.M. (1983) Arch. Neurol. 40, 374-377. [28] DiMauro, S. and Hartlage, P.L. (1978) Neurology 28, 1124-1129. [29] Miranda, A.F., Nette, G.E., Hartlage, P.L. and DiMauro, S. (1979) Neurology 29, 1538-1541. [30] Milstein, J.M., Herron, T.M. and Haas, J.E. (1989) J. Child. Neurol. 4, 186-188. [31] Cornelio, F., Bresolin, N., DiMauro, S., Mora, M. and Balestrini, M.R. (1983) Neurology 33, 1383-1385. [32] Kristjansson, K., Tsujino, S. and DiMauro, S. (1994) J. Pediatrics 125, 409-410. [33] Chiado-Piat, L, Mongini, T., Doriguzzi, C., Maniscalco, M. and Palmucci, L. (1993)Eur. Neurol. 33, 208-211. [34] Takeuchi, T. and Kuriaki, H. (1955) J. Histochem. Cytochem. 3, 153-160. [35] Bendall, J.R. (1973) in The structure and function of muscle (Bourne, G.H., ed.), pp. 243-309, Academic Press, New York. [36] Ross, B.D., Radda, G.K., Gadian, D.G., Rocker, G., Esiri, M. and Falconer-Smith, J. (1981) New EngL J. Med. 304, 1338-1342. [37] Edwards, R.H.T., Young, A. and Wiles, C.M. (1980) New Engl. J. Med. 302, 261-271. [38] Coakley, J.H., Wagenmakers, A.J.M. and Edwards, R.H.T. (1992) Am. J. Physiol. 262, E167-E172. [39] Brandt, N.J., Buchthal, F., Ebbesen, F., Kamieniecka, Z. and Krarup, C. (1977) J. Neurol. Neurosurg. Psych. 40, 920-925. [40] Dyken, M.L., Smith, D.M. and Peake, R.L. (1967) Neurology 17, 45-50. [41] Wiles, C.M., Jones, D.A. and Edwards, R.H.T. (1981) in Human muscle fatigue: physiological mechanisms (Ponter, R. and Whelan, J., eds.), pp. 264-282, Putman Med., London. [42] Cooper, R.G., Stokes, M.J. and Edwards, R.H.T (1989) J. Neurol. Sci. 93, 1-10. [43] Gollnick, P.D. (1985) Federation Proc. 44, 353-357. [44] Katz, A., Sahlin, K. and Broberg, S. (1991) Am. J. Physiol. 260, E411-E415. [45] Sahlin, K., Areskog, N.-H., Hailer, R.G., Henriksson, K.G., Jorfeldt, L. and Lewis, S.F. (1990) J. Appl. Physiol. 69, 1231-1235. [46] Hailer, R.G., Lewis, S.F., Cook, J.D. and Blomqvist, C.G. (1985) Ann. Neurol. 17, 196-199. [47] Edwards, R., Young, A. and Wiles, M. (1980) N. Engl. J. Med. 302, 261-271. [48] Brooke, M.N., Patterson, V.H. and Kaiser, K.K. (1983) Muscle Nerve 6, 204-206. [49] Mineo, I., Kono, M. and Shimizu, T. (1985) J. Clin. Invest. 76, 556-560. [50] Mineo, I., Kono, N., Yamada, Y., Hara, N., Kiyokawa, H., Hamaguchi, T., Kawachi, M., Yamasaki, T., Nakajima, H., Kuwajima, M. and Tarui, S. (1990) Muscle Nerve 13, 618-620. [51] Sinkeler, S.P.T., Joosten, E.M.G., Wevers, R.A. Binkhorst, R.A. Oerlemans, F.T., Van Bennekom, C.A. Coerwinkel, M.M. and Oei, T.L. (1986) Clin. Sci. 70, 399-400. [52] Wagenmakers, A.J.M., Coakley, J.H. and Edwards, R.H.T. (1990) Int. J. Sports Med. 11, S101-Sl13. [53] Vissing, J., Lewis, S.F., Galbo, H. and Hailer, R.G. (1992) J. Appl. Physiol. 72, 1773-1779. [54] Daegelen, D., Munnich, A., Levin, M.J., Girault, A., Goasguen, J., Kahn, A. and Dreyfus, J.C. (1983) Ann. Hum. Genet. 47, 107-115. [55] Feit, H. and Brook, M.H. (1976) Neurology 26, 963-967. [56] Gautron, S., Daegelen, D., Mennecier, F., Dubocq, D., Kahn, A. and Dreyfus, J.-C. (1987) J. Clin. Invest. 79, 275-281. [57] Koster, J.F., Slee, R.A., Jennekens, F.G.I., Wintzen, A.R. and Van Berkel, T.J.C. (1979) Clin. Chim. Acta 94, 229-235. [58] Mantle, D., Lauffart, B., Atack, J. and Lane, R.J. (1987) L Neurol. Sci. 78, 63-70. [59] McConchie, S.M., Coakley, J., Edwards, R.H.T. and Beynon, R.J. (1991) Biochim. Biophys. Acta 1096, 26-32. [60] Papadimitriou, A., Manta, P., Divari, R., Karabetsos, A., Papadimitriou, E. and Bresolin, N. (1990) J. Neurol. 237, 267-270. [61] Servidei, S., Shanske, S., Zeviani, M., Lebo, R., Fletterick, R. and DiManro, S. (1988) Ann. Neurol. 24, 774-781. [62] Daegelen-Proux, D., Kahn, A., Marie, J. and Dreyfus, J.-C. (1981) Ann. Hum. Genet. 45, 113-120. [63] Burke, J., Hwang, P., Anderson, L., Lebo, R., Gorin, F. and Fletterick, R. (1987) Proteins 2, 177-187. [64] Bergsma, D.J., Grichnik, J.M., Gossett, L.M.A. and Schwartz, R.J. (1986) Mol. Cell. Biol. 6, 2462-2475. [65] Minty, A. and Kedes, L. (1986) Mol. Cell. Biol. 6, 2125-2136. [66] Dawson, D.M., Spong, F.L. and Harrington, J.F. (1968) Ann. Intern. Med. 69, 229-235. [67] Chui, L.A. and Munsat, T.L. (1976) Arch. Neurol. 33, 636-641. [68] Manfredi, G., Silvestri, G., Servidei, S., Ricci, E., Mirabella, M., Bertini, E., Papacci, M., Rana, M. and Tonali, P. (1993) J. Neurol. Sci. 115, 91-94. [69] Schmidt, B., Servidei, S.G., Gabbai, A., Silva, A., De Souza Bulle De Oliveira, A. and Di Mauro, S. (1987) Neurology 37, 1558-1561. [70] Lebo, R.V., Anderson, L.A., DiMauro, S., Lynch, E., Hwang, P. and Fletterick, R. (1990) Hum. Genet. 86, 17-24. [71] Bartram, C., Edwards, R.H.T., Clague, J. and Beynon, R.J. (1993) Hum. Mol. Genet. 2, 1291-1293. [72] Tsujino, S., Shanske, S. and DiMauro, S. (1993) New Engl. J. Med. 329, 241-245. C. Bartram et al. / Biochimica et Biophysica Acta 1272 (1995) 1-13 [73] Beaudet, A.L. and Tsui, L.-C. (1993) Hum. Mutation 2, 245-248. [74] Bartram, C., Edwards, R.H.T., Clague, J. and Beynon, R.J. (1994) Biochim. Biophys. Acta 1226, 341-343. [75] Tsujino, S., Shanske, S., Nonaka, I., Eto, Y., Mendell, J.R,, Fenichel, G.M. and DiMauro, S. (1994) Am. J. Hum. Genet. 54, 44-52. [76] Tsujino, S., Rubin, L.A., Shanske, S. and DiMauro, S. (1994) Hum. Mut. 4, 73-75. [77] Tsujino, S., Shanske, S., Goto, Y., Nonaka, I. and DiMauro, S. (1994) Hum. Mol. Genet. 3, 1005-1006. [78] Baserga, S.J. and Benz, E.J. (1988) Proc. Natl. Acad. Sci. USA 85, 2056-2060. [79] Humphries, R.K., Ley, T.J., Anagnou, N.P., Baur, A.W. and Nienhuis, A.W. (1984) Blood 64, 23-32. [80] Kinniburgh, A.J., Maquat, L.E., Schedl, T., Rachmilewitz, E. and Ross, J. (1982) Nucleic Acids Res. 10, 5421-5427. [81] Maquat, L.E,, Kinniburgh, A.J., Rachmilewitz, E.A. and Ross, J. (1981) Cell 27, 543-553. [82] Hamosh, A., Trapnell, B.C., Zeitlin, P.L., Montrose-Rafizadeh, C., Rosenstein, B.J., Crystal, R.G. and Cutting, G.R. (1991) J. Clin, Invest. 88, 1880-1885. [83] Brown, C.A., Mclnnes, B., Dodelson de Kremer, R. and Mahuran, D.J. (1992)Biochim. Biophys. Acta 1180, 91-98. [84] Brown, A J.P. (1993) Trends Cell. Biol. 3, 180-183. [85] Titani, K., Koide, A., Hermann, J., Ericsson, L.H,, Kumar, S., Wade, R.D., Walsh, K.A., Neurath, H. and Fischer, E.H. (1977) Proc. Natl. Acad. Sci. USA 74, 4762-4766. [86] Wagenmakers, A.J.M., Coakley, J.H. and Edwards, R.H.T. (1988) Ergonomics 31, 1519-1527. [87] Kemper, H.C.G. and Verschuur, R. (1980) in Children in Exercise IX (Berg, K. and Eriksson, B.O., eds.), Int. Ser. Sports Sci., Vol. 10, pp. 55-63, Baltimore Univ. Park Press. [89] Hockaday, T.D.R., Downey, J.A. and Mottram, R.F. (1964) J. Neurol. Neurosurg. Psychiatry 27, 186-197. [90] Mahler, R.F. (1976) in Clinics in endocrinology and metabolism (Alberti, K.G.M.M., ed.), Vol. 5, pp. 579-598, W.B. Saunders Publishing Company, London. [91] Lewis. S.F., Hailer, R.G., Cook, J.D, and Blomqvist, C.G. (1984)J. Appl. Physiol. 57, 1749-1753. [92] Viskoper, R.J., Wolf, E., Chaco, J., Katz, R. and Chowers, I. (1975) Am. J. Med. Sci. 269, 217-221. [93] Wahren, J., Felig, P., Havel, R.J., Jorfeldt, L., Pernow, B. and Saltin, B. (1973) New Engl. J. Med. 288, 774-777. 13 [94] Slonim, A.E. and Goans, P.J. (1985) New Engl. J. Med. 312, 355-359. [95] Kushner, R.F. and Berman, S.A. (1990) Arch. Neurol. 47, 383-384. [96] Coakley, J.H., Wagenmakers, A.J.M. and Edwards, R.H.T. (1989) Clin. Sci. 76, 49P. [97] Wagenmakers, A.J.M., Coakley, J,H. and Edwards, R.H.T. (1987) Clin. Sci. 73, 1P [98] Millward, D.J., Garlick, P3., Nnanyelugo, D.O. and Waterlow, J.C. (1976) Biochem. J. 156, 185-188. [99] Cookson, E.J., Flannery, A.V,, Cidlowski, J.A. and Beynon, R.J. (1992) Biochem. J. 288, 291-296. [100]Cobum, S.P., Lewis, D.L., Fink, W3., Mahuren, J.D., Schaltenbrand, W.E. and Costill, D.L. (1988) Am. J. Clin. Nutr. 48, 291-4. [1Ol] Cookson, E.J. and Beynon, R.J. (1989) Int. J. Biochem. 21,975-82. [lo2] Leyland, D.M., Turner, P.C. and Beynon, R.J (1990) Biochem. J. 272, 231-237. [103] Leyland, D.M. and Beynon, R.J. (1991) Biochem. J. 278, 113-117. [104] Beynon, R.J.. Flannery, A.V., Edwards, R.H.T., Evershed, R.P. and leyland, D.M. (1993) in Proteolysis and Protein Turnover (Bond, J.S. and Barrett, A.J., eds.), pp. 157-162, Portland Press, London. [1o5] Johansson, S, Lindstedt, S., Register, U. and Wadstrom, L. (1966) Am. J. Clin. Nutr. 18, 185-196. [1o6] Coburn, S.P. (1990) Ann. NY Acad. Sci. 585, 76-85. [107] Cobum, S.P., Ziegler, P.J., Costill, D.L., Mahuren, J.D., Fink, W.J., Schaltenbrand, W.E., Pauly, T.A., Pearson, D.R., Conn, P.S. and Guilarte, T.R. (1991) Am. J. Clin. Nutr. 53, 1436-1442. [lO8] Cochary, E.F., Gershoff, S.N. and Sadowski, J.A. (1991) J. Nutr. Biochem. 2, 135-141. [lO9] Beynon, R.J., Bartram, C., Edwards, R.H.T., Gibson, H., Hopkins, P., Phoenix, J. and Toescu, V.T. (1995) Muscle and Nerve, in press. [11o] Cho, Y.O. and Leklem, J.E. (1990) J. Nutr. 120, 258-265. [lll] Hailer, R.G., Dempsey, W.B., Feit, H., Cook, J.D. and Knochel, .1.P. (1983) Am. J. Med. 74, 217-220. [112] Schaumberg, H., Kaplan, J., Windebank, A., Vick, N., Rasmus, S., Pleasure, D. and Brown, M.J. (1983) New Engl. J. Med. 309, 445-448. [ll3] Baque, S., Newgard, C.B., Gerard, R.D., Guinovart, J.J. and Gomez-Foix, A.M. (1994) Biocbem. J. 304, 1009-1014.