* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Isorhythmic AV Dissociation
Survey
Document related concepts
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
The Mechanism of Synchronization
Isorhythmic A-V Dissociation
II.
in
Clinical Studies
By MATrHEW N. LEVY, M.D.,
AND
JOSEF EDFLSTEIN, M.D.
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
SUMMARY
The electrocardiographic patterns recorded from seven patients with isorhythmic
A-V dissociation fall into two distinct groups. In pattern I, the P wave fluctuates
cyclically back and forth across the QRS complex. The mechanism responsible for
this type of A-V synchronization represents a typical biologic feedback control
system. The P-R interval is a determinant of stroke volume, which in turn influences
the arterial blood pressure. The blood pressure has an inverse effect on the discharge
frequency of the S-A node through the baroreceptor reflex. The S-A nodal frequency
then affects the P-R interval, to close the feedback loop. In pattem II, the P wave is
in a fairly constant position relative to the QRS complex. It is usually coincident with
the QRS complex or appears on the ST segment or first half of the T wave. The
mechanism producing synchronization in pattern II type of isorhythmic dissociation
has not been established conclusively.
Additional Indexing Words:
Arteriosclerotic heart disease
Arrhythmia
Complete heart block
Atrial contraction
Myocarditis
Junctional rhythm
Electrocardiogram
recently been noted in dogs with experimentally produced complete heart block.8 In these
animals, synchronization was critically dependent upon the accompanying rhythmic fluctuations in arterial blood pressure; when such
pressure variations were precluded, synchronization ceased. A feedback control loop was
shown to be operative, in which a change in
P-R interval affects the blood pressure, the
change in blood pressure alters the S-A nodal
frequency, and the consequent change in
cardiac cycle duration alters the P-R interval,
to complete the loop. In the study described
herein, observations have been made on a
group of patients with various forms of
isorhythmic dissociation to determine whether
such a correlation between P-R interval and
arterial blood pressure also prevails in the
clinical arrhythmia.
IT HAS been recognized for many years that
in complete heart block, there is a distinct
tendency toward synchronization of atria and
ventricles.'- 3 In the absence of ventricular
pacing, the ventricular contraction frequency
is ordinarily much less than the atrial contraction frequency. In such cases, synchronization
is manifested as an integral ratio of atrial to
ventricular contractions (such as 2:1, 3:1, and
3:2).
Patients with severely impaired A-V conduction but without complete block have a
pronounced tendency toward A-V synchronization when the ventricles are paced at a
frequency close to the spontaneous sinoatrial
(S-A) nodal rate.7 A similar manifestation has
From the Departments of Investigative Medicine
and Cardiology, Mt. Sinai Hospital, Cleveland, Ohio.
This work was supported by Grant HE-10951-03
from the U. S. Public Health Service.
Received May 26, 1970; revision accepted for
publication July 14, 1970.
Circulation, Volume XLII, October 1970
Artificial pacemaker
Digitalis toxicity
P-R interval
Methods
Observations were made on seven patients with
various forms of A-V dissociation. In three of
689
LEVY, EDELSTEIN
690
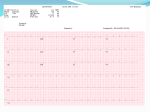
Figure 1
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Continuous strip (lead II) from a patient (case 1) with complete heart block; right yentricular pacing.
Innt
150-
0
Figure 2
Correlation between the electrocardiogram and the arterial blood pressure (mm Hg) in case 1.
Right ventricle was paced at 67 stimuli/min.
these patients, isorhythmic dissociation had
developed spontaneously. One of these patients
had chronic myocarditis, and the other two had
arteriosclerotic heart disease with digitalis toxicity. In the remaining four patients, three with
third-degree A-V block and one with seconddegree (2:1) block, temporary transvenous pacemakers had been inserted into the right ventricular cavity. In the course of studies preparatory to
the insertion of permanent pacemakers, the
tendency for A-V synchrohization was determined
by gradually varying the ventricular pacemaker
frequency. An indwelling needle was inserted into
the brachial or radial artery, and the arterial
pressure and the electrocardiogram were registered simultaneously on an Electronics for
Medicine recorder.
Results
Case 1: Complete A-V Block with
Ventricular Pacing
The electrocardiogram shown in figure 1 was
recorded from an 84-year-old man with complete
heart block. When the pacemaker frequency was
adjusted to 65 stimuli/min, which was close to
the spontaneous atrial frequency, a stable,
persistent synchronization of atria and ventricles
ensued. The two strips displayed in the figure are
continuous, and they reveal the characteristic
pattern of the oscillation of the P wave about the
QRS. At the beginning of the top strip, the P-R
interval was 0.23 sec, which was the maximum
positive value. The P wave marched progressively
to the right with respect to the QRS and passed
into and then through the QRS. The maximum
Circulation, Volume XLII, October 1970
ISORHYTUMIC DISSOCIATION
691
A
3
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
0
Figure 3
Continuotus strip from a patient (case 2) with right ventricular pacing for treatment of secondclegree A-V block (2:1).
R-P interval of 0.12 sec was reached at the end
of the top strip. The P then moved to the left relative to the QRS, so that by the end of the bottom
strip, the P was 0.21 sec before the QRS. This
oscillation of the P about the QRS was repeated
continuously, with a period of about 20 sec.
The correlation of the arterial blood pressure
and the electrocardiogram in this patient is shown
in figure 2. At the left end of the record, the P
was just visible at the end of the R wave, and the
arterial blood pressure was 115/60 mm Hg. The
P frequenicy at this point in time was slightly
greater than the R frequency, so that by the
seventh beat, the P appeared slightly in front of
the QRS, and the blood pressure started to rise.
As the P continued to move to the left of the
QRS, the blood pressure rose progressively. At the
end of the tracing, the P wave was well in front
of the QRS, and the arterial pressure had
increased to 160/85 mm Hg. The fluctuations in
arterial pressure were periodic, witlh the pressure
peaks correspondinig to the positive P-R intervals
Circulation, Volume XLII, October 1970
and the pressure troughs coincidinig with the
negative P-R (or R-P) intervals.
Case 2: Second Degree A-V Block with
Ventricular Pacing
The four consecutive electrocardiographic
strips shown in figure 3 were recorded from a 75year-old man who h-ad a pacing catheter inserted
for the treatment of a 2:1 A-V block. The
venitricular pacing frequency was gradually
increased to 100 stimuli/min, which was close to
the prevailing rate of the S-A node. This resulted
in atrioventricular synchronization, which was
manifested by a slow oscillation of the P xvave
about the QRS complex. In strip A, the P shifted
slowly from just in front of the QRS simitil it
coincided with the QRS, and finallv reappeared
in the ST segment or orn the iniitial portionl of the
T wave (strip B). The frequency of the P xave
then increased, and the P begani to marel to the
left relative to the QRS, uintil it mioved to a
maximum interval of 0.20 sec befor-e the QRS
692
LEVY, EDELSTEIN
100
75
50
25
0
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Figure 4
Correlation between the electrocardiogram (aVe) and the arterial blood pressure (mm Hg)
in case 2. Right ventricle was paced at 100 stimuli/min.
B
C
0
Figure 5
Conlitnuiouis strip (lead V) from a patient rcith chronic myocarditis (case 3).
(strips C and D). Thereafter, the P-wave
frequency diminished, and the P again moved to
the right and disappeared in the QRS complex
(end of strip D).
The correlation between the P-R interval anid
the arterial blood pressure in this patient is
displayed in figure 4. When the P wave and QRS
complex were coincident, the blood pressure was
90/35 mm Hg. When the onset of the P wave
preceded the QRS, then the arterial blood
pressure increased to a maximum valuLe of 115/40
mm Hg.
Case 3: Chronic Myocarditis with Spontaneous
Isorhythmic Dissociation
The four continuous strips of electrocardiogram
shown-i in figure 5 were recorded from a 44-yearold man with chronic myocarditis. At the
Circulation, Volume XLII, October 1970
ISORHYTHMIC DISSOCIATION
100o- 2--
7510
693
-
0
0
0
^):
0
;
k
t
;
25
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Figure 6
Correlation between electrocardiogram (lead aVF) and arterial blood pressure (mm Hg) in a
patient with complete heart block (case 4). Right ventricle paced at 84 stimuli/min. Note
premature P waves before sixth and tenth QRS complexes and the consequent reductions in
arterial blood pressure.
beginning of strip A, the P wave was buried in
the QRS complex. It gradually moved in front of
the QRS, to reach a maximum P-R interval of
0.14 sec near the middle of strip A. Thereafter,
the P wave gradually shifted back toward the
QRS, to become lost in it again near the
beginning of strip B. The P remained masked by
the QRS for about 21 sec, and then reappeared
in front of the QRS near the beginning of strip D.
A maximum P-R interval of 0.14 sec was again
attained, after which the P wave again moved to
the right to disappear within the QRS complex
once more.
Intra-arterial blood pressure recordings in this
patient revealed that when the P wave was
located in front of the QRS, the blood pressure
averaged 120/75 mm Hg. When the P wave
coincided with the QRS complex, the blood
pressure
decreased to 105/70 mm Hg.
Case 4: Complete Heart Block with
Ventricular Pacing
A pacemaker catheter was inserted in this 79year-old man for the treatment of complete heart
block. Adjustment of the frequency of the
pacemaker to that near the prevailing S-A nodal
rate resulted in A-V synchronization, with the P
wave oscillating slowly about the QRS. These
oscillations were irregular because of frequent
premature atrial contractions, and the period
varied from 15 to 45 sec.
The variations in arterial blood pressure
Circulation, Volume XLII, October 1970
associated with the changes in P-R interval are
apparent in figure 6. When the P wave was
located on the ascending limb of the T wave (first
four beats), the blood pressure was only 85/40
mm Hg. As the P gradually advanced in front of
the QRS, the blood pressure increased to 105/45
mm Hg. The influence of P-R interval on blood
pressure is also evident in the record by virtue of
the occurrence of two premature atrial contractions. After each of these atrial contractions (sixth
and tenth beats), there was a significant
reduction in the systolic arterial blood pressure
resulting from the corresponding ventricular
contractions. The excessively prolonged P-R
intervals were evidently well beyond the optimum
value.
Case 5: Arteriosclerotic Heart Disease with
Digitalis Toxicity
This 80-year-old man was admitted to the
hospital in congestive heart failure, with a history
of three previous myocardial infarctions. He had
been treated with digitoxin, antihypertensive
agents, and diuretics. His electrocardiogram on
admission exhibited signs of the remote infarctions, a prolonged P-R interval (0.22 sec), and
other effects of digitalis. On the third hospital
day, the sinus rhythm was replaced by one in
which the P waves consistently occurred shortly
after the QRS complex (fig. 7A) but were upright
in leads II, III, and aVF.
LEVY, EDELSTEIN
694
I-
D~~~
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
lFigure
Electrocardiog:ram
(lead
III) from
a patient
7
with
toxicity (case 5). A continuous strip was recorded
arteriosclerotic
heart
At the beginning of strip B, the carotid sinus regions were massaged.
strips: A-B, 35 sec; B-C,
19 sec; C-D,
18 see; D-E, 24 see; E-F,
Seven segments from a continuous tracing
(lead III) are shown in figure 7. The most
frequent position of the P wave was in the ST
segment (as in the last five beats in strip A).
However, the R-P interval occasionally became
more prolonged so that the P wave appeared just
before the summit of the T wave (as in the first
several beats of strip A). During the 35 sec which
elapsed between strips A and B, the P wave
remained in the same position as in the last few
beats of strip A.
During the first two beats of strip B, pressure
was applied to the carotid sinuses. This resulted
in a significant prolongation of the next R-R
interval of 0.30 sec, but produced a lengthening
of the corresponding P-P interval of only 0.04 sec.
As a consequence, the P wave preceded the
QRS by 0.20 sec (presumably sinus rhythm)
during the last four beats in strip B. During the
subsequent 2 or 3 min, the atria and ventricles
became dissociated. In the 19 sec between strips
B and C, the P-P and R-R intervals gradually
diminished, but the R-R interval decreased slightly more rapidly than did the P-P interval. Consequently, the P-R interval was gradually reduced,
and it measured only 0.11 sec in strip C.
Both P-P and R-R intervals gradually increased
during the 18 sec period between strips C and D,
but the increments in R-R slightly exceeded those
in P-P. Therefore, the P-R interval gradually
increased again and was 0.20 sec in strip D.
Subsequently, the S-A and junctional pacemakers
again accelerated, the junctional slightly more
disease
and
digitalis
from which seven segments were selected.
Time
33 see;
intervauls betwJeen
and
EG,
49 sec.
than the sinus nodal; again the P-R interval
gradually diminished. The P-R interval decreased
from 0.16 sec to 0.12 sec in strip E (recorded
24 sec after D), and was 0.06 sec in strip F
(recorded 33 sec after E).
There was a slight, transient prolongation of
the P-R interval after strip F was recorded. The
P-R interval then gradually diminished until the P
wave finally moved into and through the QRS. It
reappeared on the ST segment, where it remained
thereafter in a relatively fixed position. Forty-nine
seconds elapsed between strips F and C.
Repetitive determinations of systolic arterial
blood pressure were made by the usual sphygmomanometric method during the above observations. Measurements were made by a cardiology
resident who was not apprised in advance of the
purpose of the measurements nor of the existing
relationship between the P waves and QRS
complexes at the time of each blood pressure
determination. Before and during strip A, the
mean level of the systolic pressure was 116 mm
Hg. While the P wave preceded the QRS (strips
B through F), the systolic pressure averaged 130
mm Hg. When the P returned to its relatively
fixed position after the QRS (strip G), the
systolic pressure fell to 100 mm Hg.
Case 6: Complete Heart Block with
Ventricular Pacing
A transvenous pacemaker was inserted into the
right ventricle of this 68-year-old man for the
treatment of complete heart block with recurrent
Circulation, Volume XLII, October 1970
ISORHYTHMIC DISSOCIATION
695
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Figure 8
Continuous strip (lead I) recorded from case 7.
4~~~~~~4A4c~~~~~~~~
{iMf. S-M.
.........
-M* *-
.:(L
it
+
min
ATROPINE
0.8 MG
min
t+10
6~
ATROPINE
min
0.8 MG
Figure 9
+ 35
min
Segments of lead II recorded fromt case 7, 1 min before (strip 1) and 6 min after (strip 2)
atropine sulfate, 0.8 mg iv. A second injection of atropine, 0.8 mg iv, was given 7 min after
the first injection. Strips 3 and 4 were recorded 10 and 35 min, respectively, after the first
injection.
episodes of syncope. When the frequency of
ventricular pacing was different from the spontaneous S-A nodal frequency by 2 beats/min or
more, there was little tendency evident for
synchronization of atria and ventricles. When the
P waves preceded the QRS complexes, then the
arterial pressure was greater than when the P
waves occurred just after the QRS. However, the
changes in arterial pressure were not great (10 to
15 mm Hg change in systolic pressure and about
5 mm Hg change in diastolic pressure). When the
ventricular pacing frequency was within 2
beats/min of the spontaneous atrial frequency,
persistent synchronization did occur. In this
patient, however, there was no characteristic
oscillation of the P about the QRS. Instead, the P
wave remained in a rather constant position near
the beginning of the T wave.
Circulation, Volume XLII, October 1970
Case 7: Arteriosclerotic Heart Disease with
Digitalis Toxicity
Figure 8 shows a continuous rhythm strip (lead
I) recorded from a 58-year-old man in congestive
heart failure, who was treated with digoxin and
ethacrynic acid. At the beginning of the top strip,
the P wave is located in the ST segment. The R-P
interval gradually diminished, so that in beats 3
to 5 in the bottom strip, the P is manifested
simply as a slurring of the downstroke of the R
wave. The R-P interval then increased again, and
the P is clearly evident in the ST segment at the
end of the bottom strip. Similar changes in R-P
interval were also recorded in leads II, III, and
aVF. In all these leads, the P wave was
upright.
The changes in the electrocardiographic pattern associated with the intravenous injections of
696
atropine sulfate are displayed in figure 9. One
minute prior to the first injection, the heart rate
was 80 beats/min, and the P wave in lead II
was upright and located in the ST segment. Six
minutes after administration of atropine (0.8 mg),
the heart rate increased to 100 beats/min, and the
P wave was largely obscured by the QRS. A second injection of atropine was given 7 min after the
first, and 3 min later, the heart rate was still 100
beats/min, but now the beginning of the P was
evident just in front of the QRS (P-R interval,
0.04 sec). At 35 min after the first injection, the
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
mechanism had reverted briefly to a normal sin7ts
rhythm, with a heart rate of 90 beats/min and a
P-R interval of 0.15 sec. This persisted only 3
min; then the pattern returned to that observed 6
min after the first injection (second tracing, fig.
9).
Discussion
In isorhythmic dissociation, the relationship
between the P waves and QRS complexes
appears to fall into two distinct patterns. The
first type of pattern is characterized by a
rhythmic fluctuation of the interval between
the P and QRS waves, most often with the P
oscillating gradually back and forth across the
QRS; that is, with periodically varying P-R
and R-P intervals. This pattern, which has
been described previously by numerous observers,5 9-16 was characteristic of cases 1
through 4 in the present study. Furthermore,
this pattern occurred consistently in the dog
with experimentally induced A-V block in
which ventricular pacing was used.8
In the second type of electrocardiographic
pattern, the P-R or R-P interval did not
undergo rhythmic fluctuations, but the P and
R waves were in a relatively fixed position
with respect to each other. This pattern, which
has also been reported frequently,6 15,17-21
was observed in cases 5 through 7 of the
present study. It did not appear during
synchronization in the experimental animal
with complete heart block.8
Pattern I: Rhythmical Variations in P-R
and R-P Intervals
The mechanism of A-V synchronization in
this type of isorhythmic dissociation has been
elicidated by recent studies on dogs with
experimentally induced complete heart block.8
A classical biologic control system was shown
to be operative. The dissociated atrial and
LEVY, EDELSTEIN
ventricular pacemaker sites are differentially
responsive to the level of the arterial blood
pressure. The frequency of the usual atrial
pacemaker (that is, the S-A node) varies inversely as the arterial pressure, primarily via
the sino-aortic baroreceptor reflex. Idioventricular pacemaker cells are presumably less
responsive to reflex alterations in autonomic
neural activity, and with artificial ventricular
pacing, the ventricular contraction frequency
would, of course, be totally independent of
the level of the arterial blood pressure.
The phase difference (the P-R interval)
between the beginnings of atrial and ventricular activation is a determinant of stroke
volume, and hence of the arterial blood
pressure.22-28 The correlation between the
A-V contraction delay and the arterial blood
pressure in animals was described originally
by Gesell22 in 1911, and analogous phenomena
have subsequently been reported in human
subjects.2 34 In the patients analyzed in the
present study who exhibited the pattern I type
of isorhythmic dissociation (cases 1 to 4),
there was a characteristic relationship between the P-R interval and the arterial blood
pressure. As shown in figures 2, 4, and 6, as
the P wandered rhythmically back and forth
across the QRS, the blood pressure increased
significantly as the P moved in front of the
QRS, and fell as the P moved into and behind
the QRS. This relationship between the P-R
interval and the blood pressure closely resembled that seen in the experimental animal
under analogous conditions.8
In the dog with experimentally induced
complete A-V block, it was demonstrated that
the rhythmic fluctuations in blood pressure
were essential for synchronization.8 When the
amplitude of the fluctuations was severely
attenuated, synchronization ceased. In patients with the pattern I type of isorhythmic
dissociation, the same mechanism producing
synchronization undoubtedly prevails. As the
P moves to the right and passes beyond the
QRS, the blood pressure decreases, and this
reflexly accelerates the S-A node. The P then
begins to move to the left relative to the QRS,
and when the P passes in front of the QRS,
Circulation, Volume XLII, October 1970
ISORHYTHMIC DISSOCIATION
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
the blood pressure begins to rise. The motion
of the P to the left relative to the QRS is
thereby decelerated, and within a few beats,
the P begins moving to the right again, to
complete the cycle.
Synchronization can be sustained by this
mechanism when the steady-state gains of two
of the elements in this biologic feedback loop
are of sufficient magnitude.8 One of these
gains is the change in blood pressure per unit
change of P-R interval, and the other gain is
the change in S-A nodal frequency per unit
change in blood pressure. It was very difficult
to produce persistent synchronization in patient 6. The probable reason is that the first of
these system gains was inadequate. In this
patient, the arterial pressure was affected only
slightly by the position of the P relative to the
QRS. Perhaps atrial contractility was severely
depressed, so that the extent of the atrial
contribution to ventricular filling was minimal
even when the P-R interval was optimal.
Pattern II: Relatively Fixed Relationship
Between P and QRS
In this type of isorhythmic dissociation, the
P wave is in a fairly constant position relative
to the QRS complex. It is usually coincident
with and therefore hidden by the QRS complex, or it is located on the ST segment or
first half of the T wave.6' 15. 17-21 This pattern
was observed in cases 5 through 7 of the
present study (fig. 7, panels A and G; fig. 8).
Since the beginning of atrial activation occurs
synchronously with or later than the beginning of ventricular excitation, any small
change in the R-P interval is not likely to
affect arterial blood pressure significantly.
Therefore, the mechanism proposed to explain
the pattern I type of isorhythmic dissociation
cannot account for synchronization in the
pattern II of this arrhythmia.
Several other mechanisms have been proposed which could explain synchronization in
this form of isorhythmic dissociation. The
most widely cited hypothesis is that advanced
by Segers,35 who demonstrated electrical and
mechanical interactions in separate segments
of frog heart. It has been postulated that there
is an electrical interaction between dissociated
Circulation, Volume XLII, October 1970
697
atrial and ventricular pacemakers which is
analogous to that between two coupled
relaxation oscillators.'3' 36 The mechanical pulsation in the S-A node artery has been shown
to have a synchronizing effect on the pacemaker cells in that node.37 It is conceivable,
therefore, that arterial pulsations could also
produce a synchronizing effect on pacemaker
cells in the A-V junctional or ventricular
conducting tissue, thereby synchronizing atria
and ventricles. It is also possible that some
reflex mechanism might be involved, other
than that responsible for the pattern I type of
synchronization. Recent studies have demonstrated that discrete bursts of impulses in the
efferent cardiac vagus nerves tend to synchronize the pacemaker activity in the S-A node
with the rhythmic neural action potentials.38 3 Such bursts of activity in the efferent vagal pathways could originate from the
effect of ventricular ejection on the arterial
baroreceptors,40' 41 and they could thereby
synchronize atrial contraction with ventricular
ejection. In one patient in the present study
(case 7), isorhythmic dissociation ceased
briefly after atropine (fig. 9). However, the
effect did not occur until 35 min after atropine
and was so transient that this incident cannot
be considered convincing evidence in support
of a vagal reflex mechanism.
One final possibility which must be considered as an explanation for electrocardiographic pattern II is that this pattern does not really
represent isorhythmic dissociation. Waldo and
his associates2' have recently proposed that
during this arrhythmia, true A-V dissociation
is only a transient phenomenon and that the
persistent mechanism is actually an A-V
junctional rhythm. Their hypothesis may be
illustrated by referring to cases 5 and 7.
In case 5, the P wave occurred during the
early portion of the T wave (fig. 7A), and it
appeared to be upright in leads II, III, and
aVF. However, Waldo and associates2' presented cogent evidence which indicates that
upright-appearing P waves in these leads are
not incompatible with an origin in the A-V
junction. Hence, according to their hypothesis,
the arrhythmia in figure 7A and G is not
LEVY, EDELSTEIN
698
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
isorhythmic dissociation but merely an A-V
junctional rhythm with retrograde P waves
appearing as positive deflections in leads II,
III, and aVF. After carotid sinus stimulation in
this patient, a brief period of normal sinus
rhythm was followed by true A-V dissociation.
In segments C through F, there was a
rhythmic variation in the P-R interval, which
was associated with the expected changes in
arterial blood pressure. Segments C through
F, therefore, probably represent the pattern I
type of isorhythmic dissociation, as described
above. Subsequently, this presumably reverted
to a junctional rhythm (segment G).
The observations made in case 7 may also
be explained by the hypothesis proffered by
Waldo and associates. Despite the upright P
waves in leads II, III, and aVF, the continuous
rhythm strip in figure 8 might represent a
junctional rhythm, with some slow variations
in the ratios of antegrade to retrograde
conduction time to account for the changing
R-P intervals. Atropine might also have
produced some changes in the ratio of antegrade to retrograde conduction time or in
the location of the pacemaker site within the
junction, as well as a transient reversion to a
normal sinus rhythm (fig. 9).
It seems less likely that the apparent
synchronization observed in case 6 can be
explained by the hypothesis of Waldo and
associates, although this possibility cannot be
excluded entirely. In this patient with complete heart block, when synchronization was
achieved by careful adjustment of the artificial
ventricular pacemaker, the P wave occurred in
a fixed position on the ST segment. To be
compatible with the hypothesis of Waldo and
co-workers, this would have to represent
retrograde transmission to the atria. In a
patient with complete heart block, this is
unlikely, although valid instances have been
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
und Ventrikel: Erk1arung des partiellen Herzblocks. Z Klin Med 110: 401, 1929
FiscHER R: Uber das Vorkommen einfacher
zahlenmassiger Beziehungen zwischen der
Frequenz dissoziiert schlagender Herzabschnitte. Z Klin Med 116: 466, 1931
KisCm B: Boebachtungen bei einem Kranken mit
totalem Block. Cardiologia 2: 47, 1938
SEGERS M, LEQUIME L, DENOLIN H: Synchronization of auricular and ventricular beats during
complete heart block. Amer Heart J 33: 685,
1947
MARRIOTT HJL: Atrioventricular synchronization
and accrochage. Circulation 14: 38, 1956
BURCHELL HB: Experiences with electronic
pacemakers. In Mechanism and Therapy of
Cardiac Arrhythmias, edited by LS Dreifus, W
Likoff. New York, Grune & Stratton, Inc, 1966,
pp 535-541
LEVY MN, ZIESKE H: The mechanism of
synchronization in isorhythmic A-V dissociation: I. Experiments on dogs. Circulation
Research, In press
GALLAVARDIN L, VEIL P: Sur un cas de
bradycardie permanente 'a 40: Rhythme nodal
avec P positif ou dereglage auriculo-ventriculaire. Arch Mal Coeur 21: 210, 1928
ENESCU I, VACAREANU N: Dissociation auriculoventriculaire isorhythmique transitoire. Arch
Mal Coeur 27: 691, 1934
MAHAIM I, TANNER A: Dissociation iso-rhythmique provoquee avec automatisme ventriculaire accelere: Myocardite gommeuse de la
cloison. Acta Cardiol 3: 296, 1948
SEGERS M, ENDERLE J, PIRART J: Un cas de
dissociation isorhythmique. Acta Cardiol 8:
417, 1953
GRANT RP: The mechanism of A-V arrhythmias,
with an electronic analogue of the human A-V
node. Amer J Med 20: 334, 1956
14. MARRIOTr HJL, SCHUBART AF, BRADLEY SM: A-
15.
16.
17.
reported.'7
References
18.
1. LEWIS T: The Mechanism and Graphic Registration of the Heart Beat, ed 3. London, Shaw
and Sons, Ltd, 1925, p 178
2. VAN BUCHEM FSP: Dissoziation zwischen Atrium
19.
V dissociation: A reappraisal. Amer J Cardiol
2: 586, 1958
SCHOTT A: Atrioventricular dissociation with and
without interference. Progr Cardiovasc Dis 2:
444, 1959
ScHERF D, COHEN J: The Atrioventricular Node
and Selected Cardiac Arrhythmias. New York,
Grune & Stratton, Inc, 1964 pp. 288-295
MARRIoTT HJL: Interactions between atria and
ventricles during interference dissociation and
complete A-V block. Amer Heart J 53: 884,
1957
SCHUBART AF, MARRIOTT HJL, GORTEN RJ:
Isorhythmic dissociation: Atrioventricular dissociation with synchronization. Amer J Med
24: 209, 1958
AVERILL KH, LAMB LE: Less commonly
Circulation, Volume XLII, October 1970
ISORHYTHMIC DISSOCIATION
recognized actions of atropine on cardiac
rhythm. Amer J Med Sci 237: 304, 1959
20. JACOBS DR, DONOSo E, FRIEDBERG CK: A-V
dissociation: A relatively frequent arrhythmia.
Medicine 40: 101, 1961
21. WALDO AL, VrrIKAINEN KJ, HARRIS PD, ET AL:
The mechanism of synchronization in isorhythmic A-V dissociation. Circulation 38: 880,
1968
22. GESELL RA: Auricular systole and its relation to
ventricular output. Amer J Physiol 29: 32,
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
1911
23. BROCKMAN SK: Dynamic function of atrial
contraction in regulation of cardiac performance. Amer J Physiol 204: 597, 1963
24. SKINNER NS, JR, MITCHELL JH, WVALLACE AG,
ET AL: Hemodynamic effects of altering the
timing of atrial systole. Amer J Physiol 205:
499, 1963
25. MITCHELL JH, GUPTA DN, PAYNE RM: Influence
of atrial systole on effective ventricular stroke
volume. Circulation Research 17: 11, 1965
26. BENCHIMOL A, MAROKO P, GARTLAN J, ET AL:
Continuous measurements of arterial flow in
man during atrial and ventricular arrhythmias.
Amer J Med 46: 52, 1969
27. BENCHIMOL A, STEGALL HF, MAROKO PR, ET AL:
Aortic flow velocity in man during cardiac
arrhythmias measured with the Doppler catheter-flowmeter system. Amer Heart J 78: 649,
1969
28. RUSKIN J, MCHALE PA, HARLEY A, ET AL:
Pressure-flow studies in man: Effect of atrial
systole on left ventricular function. J Clin
Invest 49: 472, 1970
29. BRAUNWALD E, FRAHM CJ: Studies on Starling's
law of the heart: IV. Observations on the
hemodynamic functions of the left atrium in
man. Circulation 24: 633, 1961
30. SAMET P, JACOBS W, BERNSTEIN WH, ET AL:
Hemodynamic sequelae of idioventricular
Circulation, Volume XLII, October 1970
699
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
pacemaking in complete heart block. Amer J
Cardiol 11: 594, 1963
SAMET P, BERNSTEIN W, LEVINE S: Significance
of the atrial contribution to ventricular filling.
Amer J Cardiol 15: 195, 1965
CARLETON RA, PASSOVOY M, GRAE`TTINGER JS:
The importance of the contribution and timing
of left atrial systole. Clin Sci 30: 151, 1966
TSAGARIS TJ, BUSTAMANTE RA, FRIESENDORF
RA: Unusual complication of transvenous
electrical pacing of the heart. Dis Chest 53:
110, 1968
LEINBACH RC, CHAMBERLAIN DA, KASTOR JA,
ET AL: A comparison of the hemodynamic
effects of ventricular and sequential A-V
pacing in patients with heart block. Amer
Heart J 78: 502, 1969
SEGERS M: Les phenomenes de synchronisation
au niveau du coeur. Arch Internat Physiol 54:
87, 1946
NADEAU RA, ROBERGE FA: The mechanism of
A-V arrhythmias: In Electrical Activity of the
Heart, edited by GW Manning, SP Ahuja.
Springfield, Charles C Thomas, Publishers,
1969, pp 117-128
JAMES TN: Pulse and impulse in the sinus node.
Henry Ford Hosp Med Bull 15: 275, 1967
REID JVO: The cardiac pacemaker: Effects of
regularly spaced nervous input. Amer Heart J
78: 58, 1969
LEVY MN, MARTIN PJ, IANO T, ET AL:
Paradoxical effect of vagus nerve stimulation
on heart rate in dogs. Circulation Research
25: 303, 1969
IRIUCHIJIMA J, KUMADA M: Efferent cardiac
vagal discharge of the dog in response to
electrical stimulation of sensory nerves. Jap J
Physiol 13: 599, 1963
IRIUCMJIMA J, KUMADA M: Activity of single
vagal fibers efferent to the heart. Jap J Physiol
14: 479, 1964
The Mechanism of Synchronization in Isorhythmic A-V Dissociation: II. Clinical
Studies
MATTHEW N. LEVY and JOSEF EDFLSTEIN
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Circulation. 1970;42:689-699
doi: 10.1161/01.CIR.42.4.689
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1970 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://circ.ahajournals.org/content/42/4/689
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles
originally published in Circulation can be obtained via RightsLink, a service of the Copyright
Clearance Center, not the Editorial Office. Once the online version of the published article for
which permission is being requested is located, click Request Permissions in the middle column of
the Web page under Services. Further information about this process is available in the Permissions
and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/