* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download anomalous pulmonary venous return with stenosis in
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Aortic stenosis wikipedia , lookup
Echocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Congenital heart defect wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
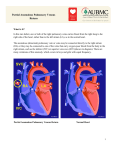
PRENAT CARDIO. 2013 MAR;3(1):22-27 Ewa Góra et. al. Case Report ANOMALOUS PULMONARY VENOUS RETURN WITH STENOSIS IN COMPLEX LEFT HEART DEFECT - LETHAL ANOMALY - 3 CASES REPORT. Authors: Ewa Góra1, Hanna Moczulska2,3, Ewelina Litwińska4, Maciej Słodki2,5, Maria Respondek – Liberska2 NZOZ”Sonomedika”, 2 Department for of Diagnosis and Prevention of Congenital Defects, Polish Mother’s Memorial Hospital, Research Institute in Lodz & Medical University of Lodz (ZDiPWW, ICZMP) 93-338 Łodz, ul. Rzgowska 281/289, 3 Department of Genetic , Medical Univesity in Lodz, 4 Department of Perinatology and Gynecology , Polish Mother’s Memorial Hospital, Research Institute in Lodz 5 Institute of Health Science of Public High School in Plock 1 PRENAT CARDIO 2013 MAR;3(1):22-27 DOI 10.12847/03134 Abstract In prenatal cardiology center 3 cases of anomalous pulmonary venous return with pulmonary venous stenosis were diagnosed on the basis of continues Doppler blood flow (V max >100 cm/sec). In each of 3 cases left heart defect was diagnosed at 29th, 35th and 36th week of gestation. In each case newborn died on the 1st or 2nd day of life before qualification to cardiac surgery. At present, anomalous pulmonary venous return with pulmonary venous stenosis and complex heart defect in fetus seems to be lethal cardiac defect. Key words: anomalous pulmonary venous return, pulmonary venous stenosis, left heart defect, lethal cardiac defect. INTRODUCTION was registered by continues Doppler. In subsequent two examinations these findings were confirmed and additionally holosystolic tricuspid valve insufficiency was detected (2 m/s) (Graph.1). Abnormal pulmonary venous return was first described as total anomalous pulmonary venous return (TAPVR) by Willson in 17891. In this cardiac defect pulmonary At 39 th week of gestation veins do not enter into left atrium, there was spontaneous delivery. but to different parts of systemic Female newborn’s birth weight venous tract. How to cite this article: was 2900 grams and Apgar was It leeds to life risk of newborn, Góra E, Moczulska H, Janiak K, 4/7. Despite prostin infusion and especially when outlets of Słodki M, Respondek-Liberska M. intensive care on the 2nd day of pulmonary veins are stenotic. In Anomalous pulmonary venous return with life the newborn died. Autopsy literature we can find only few stenosis in complex left heart defect – revealed the same diagnosis case reports of prenatal diagnosis lethal anomaly – 3 cases report. as in prenatal examination of TAPVR but none with venous Prenat Cardio. 2013 Mar;3(1):22-27 (two chamber heart: common stenosis. We would like to present (morphologicaly right) ventricle, 3 cases, based on our own residual left atrium, total anomalous pulmonary venous experience of Prenatal Cardiology Center of ICZMP in return to persistent left superior vena cava, dilatation of Lodz, indicating that pulmonary vein stenosis in fetus pulmonary trunk and its branches with widly opened with left heart defect may suggest lethal cardiac defect. ductus arteriosus. Case report 1 (year 1995) Case report 2 (year 2006) Gravida 2, para 2 with high risk pregnancy with family A 36-year old woman, gravida 2 para 1, with high risk history of mild aortic valve insufficiency (C1 – male of aneuploidy in threefold test, after amniopunction without surgical treatment) was admitted to our unit at with fetuses Robertson translocation - 45, XX,der(14;15) 28th week of gestation. Echocardiography showed left (q10;q10 ) was admitted to our unit to perform fetal heart hypoplasia (HLHS) with double outlet right ventricle echocardiography due to ascites, pericardial effusion and (DORV) and total anomalous pulmonary venous return abnormal four chamber view suggesting left heart defect . to common collector flowing into persistant left superior At 28 th week of gestation by targeted echocardiography vena cava (LSVC). Behind left atrium wall abnormal we confirmed situs solitus, cardiomegaly (HA/CA 0,5), flow in venous vessel (accelerated to V max 100 cm/s) pericardial effusion, aortic valve atresia with restriction of Corresponding author: [email protected] 22 Unauthenticated Download Date | 6/17/17 10:03 PM Anomalous pulmonary venous return with stenosis in complex left heart defect – lethal anomaly – 3 cases report. foramen ovale (FOC) and additionally anomalous pulmonary venous return with collector was detected. This anomalous confluence formed conglomerate in pericardium in region of left atrium imitating tumor (Fot.1). Flow in pulmonary veins was abnormal high up to 100 cm/sec. Systemic peripheral flows (UMB A,V; MCA) were normal with regular fetal heart rate. After patient couselling transplacental pharmacological treatment with Digoxine was undertaken with echocardiological monitoring. In next 2 weeks not only there was no improvement in fetal circulation but also total foramen ovale closure and opening of numerous ventricular septum defects with right-left flows were detected (Graph.2). Pict.1. Schematic drawing of the fetal heart case nr 1 These findings forced us to withdrawal transplacental pharmacology. At 36th week of gestation hydrothorax and right pyelectasis were detected. One week later cesarean section was performed because of premature labour and female newborn was born with birth weight of 2400 grams and Apgar score of 5. Baby died the same day because of circulatory and respiratory failure. Autopsy confirmed prenatal diagnosis: closure of foramen ovale, excess of ventricular septum and anomalous “receiver” of pulmonary veins with numerous overgrowth diverticuli in region of left atrium. Case report 3 (year 2012) In 35-year old woman, gravida 2, para 2 (C1- healthy female), in low risk pregnancy, three ultrasonographical examinations were performed at 10th, 14th, 19th week of gestation described as normal. At 34 th week of gestation patient was referred to our unit for detailed echocardiography due to abnormal four chamber view. We described: In 2D presentation: situs solitus, abnormal axis of the heart - 91°, normal heart size (HA/HC 0,3, AP 36 mm); four chamber view with 2 symmetrical atria and 2 asymmetrical ventricles – thick, small contracted LV, dominant RV; FO of 3,2 mm ( small) with left-right blood flow; interventrical septum without defect; connections A-V and V-A concordant; mediastinum abnormal: 2 vessels (PV – 11 mm, SVC – 6 mm); thymus present; wide ductal arch was present but aortic arch was difficult to assess with Y sign indicating aortic arch interruption. Descending aorta was 7 mm; systemic veins flow with wider superior vena cava (SVC – 6 mm, IVC – 3,4 mm); anomalous pulmonary venous return with collector deflecting to left atrium, probably with inflow to SVC. In 2DD +CD presentation: intracardiac flows: tricuspid valve insufficiency, normal pulmonary valve flow ; bilateral blood flow in narrowed (2 mm) pulmonary veins; UMB A,V flow normal with regular fetal heart rate (140/min). Pict.2. Schematic drawing of the fetal heart case nr 2 Based on these findings diagnosis was established such Unauthenticated Download Date | 6/17/17 10:03 PM 23 PRENAT CARDIO. 2013 MAR;3(1):22-27 Ewa Góra et. al. day he died of circulatory and respiratory failure. He was excused from autopsy on parents’ request. Specification of the 3 cases data are presented in Table 1. DISCUSSION The incidence of total anomalous pulmonary venous return (TAPVR) is 1:17000 life born and accounts for 1,5 % of all congenital heart defects. The condition appears in 1% of cases operated on in pediatric cardiosurgical centres and can be found in 4% newborns during autopsy. This heart defect is one of the most difficult anomalies to detect prenatally what was confirmed in UOG in 2012 where only 8 (1,9%) of 424 TAPVR cases were diagnosed in fetuses before the delivery2. We registered 3 cases of TAPVR with obstruction in our centre (Table 1). All these cases ended up with death in 1st or 2nd day of newborns life. We recorded a very special Doppler tracings in each case with typical sound of turbulent blood flows. These anomalies are extremely rare (that is why we presented also an individual year of each diagnosis) and prenatal diagnosis very essential to predict early demise of the newborn (in contrast to similar heart defects without anomalous pulmonary venous connection, which can be operated on in 2nd – 3rd week after delivery). Pict.3. Schmatic drawing of the fetal heart case nr 3 a s : Generally we oblige to Darling’s 3 classification of total anomalous pulmonary venous return which hypoplastic left heart (HLHS), tricuspid insufficiency (TR), interrupted aortic arch (IAA type B) and partial anomalous pulmonary venous return (PAPVR) (supracardiac) probably with inflow to SVC and collector “closing” FO (Graph 3). Circulatory system was efficient in fetus, cardiovascular profile score was 10. Cesarean section was performed at 37th week of gestation after amniotic sac rupture and contraction appearance. Male birth weight was 2570 g (10th – 25th percentile range) and Apgar score 9. After admission to Intensive Care Unit newborn was followed a course of Prostin 0,01 µg/kg/min. Next Fot.1. 4 ch fetal heart with pericardial effusion 24 Unauthenticated Download Date | 6/17/17 10:03 PM Anomalous pulmonary venous return with stenosis in complex left heart defect – lethal anomaly – 3 cases report. Case 1 Year Age of gravida High risk pregnancy Case 2 1995 2008 2012 29 36 35 yes Week of gestation during diagnosis Case 3 yes 28 Type of heart defect HLHS+ DORV+TR multipe VSD, pericardial effusion HLHS + IAA + TR Type of anomalous pulmonary venous return no 28 34 Aortic valve atresis, FO closure, HLHS + IAA + TR total /supracardiac total/cardiac partial/supracardiac V max for PV 80 cm/sec 100 cm/sec 100 cm/sec Pericardial effusion no yes no Delivery SN CS CS Weigh of newborn Apgar 2900 2400 2570 4/7 5 9 Gender Decease 2nd day 1st day 2nd day Table 1. Specification of data – 3 cases with anomalous pulmonary venous return from our unit : Department for Diagnosis and Prevention of Congenital Malformations (Polish Mother’s Memorial Hospital & Medical University of Lodz) Unauthenticated Download Date | 6/17/17 10:03 PM 25 PRENAT CARDIO. 2013 MAR;3(1):22-27 divide TAPVR into 4 types, depending on site which pulmonary veins are connect to: supracardiac, cardiac, infracardiac or multiple. In supracardiac connection (41%) pulmonary veins join into common vessel and drain into vena cava, vena azygos or left cephalobrachial truncus. In cardiac connection (31%) they drain directly to right atrium or coronary sinus. The infracardiac connection (24%) can be through common vessel to the inferior vena cava, hepatic vein, portal vein, or gastric vein. The mixed type (4%) is a combination of two or three connections earlier described. In our cases vein collector was anomalous and crated an image of “tumor” behind left atrium (case 2) or alteration bulging into left atrium with pressure on to atrial septum (case 3). In current literature there is little data about total anomalous pulmonary venous return in fetuses because it is rare and difficult to detect prenatally. There are indirect echocardiographic criteria, such as: small left atrium, right ventricular and right atrial dominance and dilated pulmonary artery. But these signs can appear also in typical and common heart defects. We should pick up an anomalous alterations behind left atrium which can suggest TAPVR4,5,6,7,8,9. Also dilatation of superior vena cava can support the diagnosis10 as in the case 3. Diagnosis of TAPVR using only one ultrasonoghraphic marker can lead to false positive identification. Characteristic echocardiographic abnormal the 4 chamber view, dominant RV and abnormal the 3VT view was observed in all cases with left heart defect (2 x HLHS, 1 x aortic atresia with Fo obliteration). Our findings confirm Al-Naami’s observation, that there is common appearance TAPVR with other structural heart defects, especially left heart defects 9. One of the theories of left heart anomalies (eg. HLHS, aortic stenosis) is limited flow through foramen ovale 11. Primary Fo occlusion may lead to right heart enlargement and right heart failure, cardiomegaly and fetus oedema (Case 2 – pericardial effusion, hydrothorax). The probable reason for fetus survival was due to “opening” of multi VSDs, which enabled right-left flow replacing closed Fo. The most important in each case was auscultation of intracardiac flows by electronic stethoscope – Doppler and registration of abnormal spectra over 100 cm/sec in left atrium region. These findings should be differentiated with reverse blood flow in venous vessels of fetus lungs observed in Fo restriction or other anomalous resistance in pulmonary circulation. Traditionally HLHS, AS, aortic valve atresia are qualified as critical heart defects or planned to Prostin administration after delivery in order to maintain permeability of arterial duct till cardiac surgery is performed 10,12,13. 26 Ewa Góra et. al. But described cases were different. These complex heart defects despite of echocardiographic supervision and deliveries performed in main obstetric center, caused quick hemodynamic deterioration and demises of newborns before surgery. Similar natural history/course of pulmonary veins restriction was described by colleagues from Korea14. Maybe in future prenatal diagnosis of this specific cardiac condition can lead to stent insertion into described pulmonary veins restriction just after delivery. CONCLUSION At present prenatal anomalous pulmonary venous return with stenosis in left heart diseases seems to be a features of rare lethal cardiac defect. References: 1. Wilson J. A description of a very unusual formation of the human heart, Philos. Trans. R. Soc. Lond. 1798, 88,346 2. Gardiner M, Mellander M, Roughton M, Simpson J, Tometzki A, Uzun O, S. A. Webber SA and Daubeney PEF, on behalf of the British ongenital Cardiac. Total anomalous pulmonary venous connection: impact of prenatal diagnosis. Ultrasound in Obstetrics & Gynecology 2012, 40, 3, 310–318 3. Darling R. C., Rothney W. B., Craig J. M. Total pulmonary venous drainage into the right side of the heart, Lab. Invest. 1957, 6,44 4. Allan L.D., Sharland G.K. The echocardiographic diagnosis of totalny anomalous pulmonary venous connection in the fetus. Heart 2001;85:433–437 5. Allan LD., Cook AC., Huggon IC. Fetal echocardiography: a practical guide. London, 2009 6. Seale AN, Uemura H, Webber SA, Partridge J, Roughton M, Ho SY, McCarthy KP, Jones S, Shaughnessy L, Sunnegardh J, Hanseus K, Berggren H, Johansson S, Rigby ML, Keeton BR, Daubeney PE; British Congenital Cardiac Association. Total anomalous pulmonary venous connection: morphology and outcome from an international population-based study. Circulation. 2010 Dec 21;122(25):2718-26 7. Valsangiacomo ER, Hornberger LK, Barrea C, Smallhorn JF, Yoo SJ. Partial and total anomalous pulmonary venous connection in the fetus: two-dimensional and Doppler echocardiographic findings. Ultrasound Obstet Gynecol. 2003 Sep;22(3):257-63 8. Berg C, Georgiadis M, Geipel A, Gembruch U. The area behind the heart in the four-chamber view and the quest for congenital heart defects. Ultrasound Obstet Gynecol. 2007 Oct;30(5):721-7 9. Al-Naami GH, Al-Mesned AA. Total anomalous pulmonary venous drainage to coronary sinus combined with left-sided obstructive lesions: a previously unreported association. Congenit Heart Dis. 2009 Nov-Dec;4(6):469-73 10. Respondek-Liberska M., Janiak K., Moll J., Ostrowska K., Czichos E. Prenatal diagnosis of partial anomalous pulmonary venous connection by detection of dilatation of superior vena cava in hypoplastic left heart. A case report. Fetal Diagnosis and Therapy. 2002 SepOct;17(5):298-301 11. Papa M, Camesasca C, Santoro F, Zoia E, Fragasso G, Giannico S, Chierchia SL. Fetal echocardiography in detecting anomalous pulmonary venous connection: four false positive cases.Br Heart J. 1995 Apr;73(4):355-8 Unauthenticated Download Date | 6/17/17 10:03 PM Anomalous pulmonary venous return with stenosis in complex left heart defect – lethal anomaly – 3 cases report. 12. Szymkiewicz-Dangel J. Kardiologia Płodu. Zasady diagnostyki i terapii. Poznań, 2007 13. Respondek-Liberska M. Atlas Wad Serca Płodu. 2011, Adi Art., Łódź 14. Choi E. S, Won H. S., Shim J. Y., Lee P. R., Kim A. Prenatal echocardiography of total anomalous pulmonary venous connection (TAPVC) : isolated or accompanied by pulmonary venous stenosis . Ultrasound in Obstetrics & Gynecology, 2007, Special Issue: 17th World Congress on Ultrasound in Obstetrics and Gynecology, 30, 4, 574 Conflict of interest: The author declares no conflict of interest and did not receive any remuneration Unauthenticated Download Date | 6/17/17 10:03 PM 27