* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 12
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Rheumatic fever wikipedia , lookup
Artificial heart valve wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
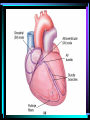
Chapter 12 The Heart Introduction • All cardiovascular function depend on the heart. • It beats 100,000/day • Pumps 8000 liters of blood/day The Heart and Circulatory System • The circulatory system can be subdivided into the pulmonary circuit and the systemic circuit. • Arteries carry blood away from the heart and • Veins return blood to the heart. • Capillaries are tiny vessels between arteries and veins. • The heart has four chambers – The right atrium – The right ventricle – The left atrium – The left ventricle The Anatomy and Organization of the Heart • The heart is surrounded by the pericardial cavity • The visceral pericardium (epicardium) covers the heart’s outer surface. • The parietal pericardium lines the inner surface of the pericardial sac which surrounds the heart. Surface anatomy of the heart • The coronary sulcus, a deep groove, marks the boundary between the atria and ventricles. The Heart Wall • The bulk of the heart consists of the muscular myocardium • The endocardium lines the inner surfaces of the heart • The fibrous skeleton supports the heart’s contractile cells and valves. • Cardiac muscle cells are interconnected by intercalated discs, which convey the force of contraction from cell to cell and conduct action potentials. Internal Anatomy and Organization • The atria are separated by the interatrial septum and the ventricles are divided by the interventricular septum • The right atria receives blood from the systemic circuit via two large veins, the superior vena cava and inferior vena cava • Blood flows from the right atrium into the right ventricle through the right atrioventricular (AV) valve (tricuspid valve. • The opening is bounded by three cusps of fibrous tissue braced by the tendinous chordae tendineae with are connected to papillary muscles. • Blood leaving the right ventricle enters the pulmonary trunk after passing through the pulmonary semilunar valve. • The pulmonary trunk divides to form the left and right pulmonary arteries. • The left and right pulmonary veins return blood to the left atrium • Blood leaving the left atrium flows into the left ventricle through the left atrioventicular valve (bicuspid valve) • Blood leaving the left ventricle passes through the aortic semilunar valve and into the systemic circuit via the aorta. • Anatomical difference between the ventricles reflect the functional demands on them • The walls of the right ventricle is relatively thin, while the left ventricle has a massive muscular wall. • Valves normally permit blood flow in only one direction preventing regurgitation(backflow) of blood. The Blood supply to the Heart • Coronary circulation meets the high oxygen and nutrient demands of cardiac muscle cells • The coronary arteries originate at the base of the aorta THE HEARTBEAT In a single heartbeat, the entire heart (atria and ventricles) contract in a coordinated manner so that blood flows in the correct direction at the proper time. Two general classes of cardiac cells are involved in the normal heartbeat: contractile cells and cells of the conducting system Contractile Cells Uses a similar method of contraction as skeletal muscle cells, but Ca2+ ions enter the muscle fiber for a longer period creating delaying repolaization and lengthening the muscle contraction. The Conduction System • The conducting system includes nodal cells and conducting cells both of which do not contract.. • The conduction system initiates and distributes electrical impulses in the heart. • Nodal cells establish the rate of cardiac contraction • Pacemaker cells are nodal cells that reach threshold first. • Conducting cells distribute the contractile stimulus to the general myocardium • Unlike skeletal muscle, cardiac muscle contracts without neural or hormonal stimulation. • Pacemaker cells in the sinoatrial (SA) node normally establish the rate of contraction. • From the SA node, the stimulus travels to the atrioventricular (AV) node . • From the AV node the stimulus travels to the AV bundle, which divides into bundle branches. • From there Purkinje fibers convey the impulses to the ventricular myocardium The Electrocardiogram • A recording of the electrical activities in the heart is an electrocardiogram (ECG or EKG) • Important landmarks of an ECG include: the P wave (atrial depolarization) – QRS complex (ventricular depolarization – T wave (ventricular repolarization) The Cardiac Cycle • The cardiac cycle consists of systole (contraction) followed by diastole (relaxation) • Both ventricle contract at the same time, and they eject equal volumes of blood. • The closing of the heart valves and the rushing of blood through the heart cause characteristic heart sounds. Heart Sounds • The first heart sound (“lubb”) is produced as the AV valves close and the semilunar valves open. • The second heart sound (“dupp”) occurs when the semilunar valves close. • What is going on in the heart during each of these sounds? HEART DYNAMICS • Heart dynamics refers to the movements and forces generated during contractions. • The amount of blood ejected by a ventricle during a single heat is the stroke volume (SV) • The amount of blood pumped each minute is the cardiac output (CO) Factors Controlling Cardiac Output • The major factors that affect cardiac output are: – blood volume reflexes , – autonomic innervation, – and hormones. • Blood volume reflexes are stimulated by changes in venous return, the amount of blood entering the heart. • The atrial reflex accelerates the heart rate when the walls of the right atrium are stretched. • Ventricular contractions become more powerful and increase stroke volume when the ventricular walls are stretched. • The basic heart rate is established by the pacemaker cells but it can be modified by the autonomic nervous system. • Acetylcholine released by parasympathetic motor neurons lowers heart rate and stroke volume. • Norepinephrine released by sympathetic neurons increases the heart rate and stroke volume • Epinephrine and norpinephrine, hormones released by the adrenal medullae during sympathetic activation, increase both heart rate and stroke volume. • Thyroid hormones and glucagon also act to increase cardiac output. • The cardioacceleratory center in the medulla oblongata activates sympathetic neurons; • The cardioinhibitory center governs the activities of the parasympathetic neurons. • These cardiac centers receive inputs from higher centers and from receptors monitoring blood pressure and the levels of dissolved gases.