* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diastolic LV function and HFNEF
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
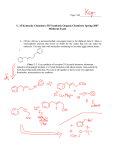
Mitral insufficiency wikipedia , lookup
Diastolic LV function and HFNEF FRIJO JOSE A • Approximately 50% of pts with HF have a normal or near normal LVEF Mayo Clinic registry • • • • • • Women Hypertension (up to 88%) Obesity (BMI >30 kg/m2 → 40%) Renal failure Anemia AF • Diabetes (30%) • CAD (40%-50%) similar to that in HF patients with impaired LVEF • Lower overall mortality in HFNEF v/s SHF patients (2.8% vs 3.9%; P = 0.005) • Symptom burden, duration of ICU stay & hospital stay, long-term mortality – similar ADHERE database- 52,187 patients Clinical ∆ of HF (Framingham criteria) and an LVEF > 50% • True- typically excluded – “significant” CAD(most often clinically assessed) – Hypertrophic cardiomyopathy – Valvular heart disease Morphologic Features • Higher cardiomyocyte diameter • Higher myofibrillar density • Collagen volume fraction was similar D/D to the Syndrome of HFNEF Diastolic function • Major factors influencing relaxation – Cytosolic Ca level must fall- requires ATP & phosphorylation of phospholamban – Inherent viscoelastic properties of myocard – (hypertrophied heart -↑fibrosis, relaxation – slower) – ↑ phosphorylation of troponin I – Influenced by systolic load- ↑ the systolic load, the faster the rate of relaxation Diastolic function • SHF pts →LV pressure–volume analysis →less steep slope of end-systolic LV pressure– volume relationship • HFNEF pts → – Upward and leftward shifted end-diastolic pressure–volume relationship – End-systolic pressure–volume relationshipunaltered or even steeper HFNEF • ↑LV stiffness – Very small changes in LVEDV→ Marked ↑ in LVEDP & pulm venous P→ dyspnea during exercise, even pulm edema – Impaired LV filling and inability to use FrankStarling mech→ Failure to ↑CO during exercise→ Exercise intolerance Is diastolic dysfunction the only explanation? • TDI - ↓ systolic mitral annular amplitudes—in HFNEF pts V/S controls • These changes – not as pronouncd as in SHF pts • ? initial abn compensated for by ventri hypertrophy & neurohormonal activation →hypercontractile LV state with abn relaxation →resistance to LV filling →progress →phenotype characteristic of SHF • However, data lacking & progression have been shown to occur rarely • 2,042 participants • Incidence of mod-sev LV diast dysf in presence of an LVEF >50% - 5.6% • Only ~ 1% of study population had symptoms of HF & an LVEF >50%. Redfield MM et al. JAMA 2003;289:194 –202. – 37 HFNEF pts (prev pulm edema, LVEF >50%) – 40 pts with hypertensive LVH without HF – 56 control subjects • HFNEF V/S HTN LVH and control - ↑LV mass index, ↑conc LV geometry, ↑E/E’ ratio, ↑LA volume • Distinguished HFNEF pts very well from control but not from asymptomatic hypertensive LVH • Product of LV mass index and LA volume highest accuracy for predicting HFNEF Melenovsky V et al. J Am Coll Cardiol 2007;49:198–207 • Anemia, renal dysf • ? Volume overload rather than an intrinsic abn of LV diastolic function -pathophysio of HFNEF LV systolic function • LVEF as a measure of LV systolic function questioned-load dependence • Annular peak syst velocity (TDI) ↓in HFNEF • Still controversial- whether LV syst function is N in HFNEF Ventriculovascular coupling in HFNEF • Effective art elastance- global measure of art stiffness(LVESP/SV)- ↑ HFNEF pts • Combined ventri-art stiffening contributes to HFNEF Mechanisms – 1) exaggerated↑ SBP after small ↑ in LVEDV – 2) a marked ↑ SBP after a further ↑ in art elastance in presence of a high ES elastance – 3) limited systolic reserve due to ↑ baseline ES elastance – 4) ↑ cardiac work to deliver a given CO – 5) a direct influence of ↑ art elastance on LV diast functn First 2 also explain sensitivity of these pts to overdiuresis & aggr vasodilator therapy Role of Atrial Fibrillation Atria • Blood-receiving reservoir chamber • Contractile chamber • Conduit • Volume sensor of the heart, releasing ANP in response to intermittent stretch • Contains receptors for afferent arms of various reflexes – mechanoreceptors that ↑sinus discharge rate, thereby contributing to the tachycardia of exercise as the venous return increases (Bainbridge reflex) Role of Atrial Fibrillation • The prevalence of AF in HFNEF ≈ 20% to 30% • Fung et al- HFNEF pts with AF (29%) had ↓ functional class & quality of life than without AF • CHARM - AF →adv CV outcomes irrespective of baseline LVEF – High HR, loss of atrial systole, irr cycle length with implications of the Frank-Starling mechanism, episodic nature • Echocardiographic assess challenging – Fung et al - similar E/E’ ratios in HFNEF with and without AF but larger LA size in AF – Melenovsky et al - LA emptying fraction ↓in HFNEF pts than hypertensive LVH & during handgrip, late diastolic annular tissue velocity - unchanged in HFNEF but ↑ in control (5% vs. 35%) Role of Coronary Artery Disease • Ischemia affects early diastole by ↑ Tau • Reversed after removal of ischemic burden by CABG ?Considerable no of pts with atypical presentation of ischemia (silent/dyspnea) labeled as HFNEF • 15% incidence of hospital admission due to UA in pts previously ∆ with HFNEF -38/12 Volume overload • HF with either ↓/N EF is a Na-sensitive condition • HFNEF- ↑ likely to have multiple comorbidities that may contribute to volume overload – Renovascular disease, obesity, OSAHS, anemia • Plasma volumes of HTN HFNEF - ↑ by an average of 16% compared with N controls despite daily diuretic use • UNLOAD -ultrafiltration -186 pts -45 NEF→½ ultrafiltration, other ½ IV diuretics • Volume expansion precedes sympt, volume removal alleviates sympt without inducing hypotension/end-organ dysf • HFNEF → ↑ risk of recur of fluid overload • A/c pulm edema - common manifestation of HFNEF→ diuretics remain mainstay • Diuretics & dietary salt restrict- paramount to care of HFNEF pts Venoconstriction/volume redistribution • ≈ 85% of blood vol- venous circulation • Small alterations in venous tone & capacitance (esp splanchnic bed) → impact the distri of intravasc vol - imp determinant of LVED filling P – Data lacking – Most imp drugs used in a/c pulm edema → venodilators & diuretics ? Improvements-at least partly due to ↓autonomic tone & resulting ↑in venous capacitance Diagnosis of HFNEF 2007- European Working Group on HFNEF 3 conditions must be fulfilled – 1) symptoms & signs of HF – 2) LVEF >50% in a nondilated LV (LVEDV<97 ml/m2) – 3) evidence of ↑LV filling P 3 ways to ∆ ↑ LV filling P – invasive measurements – unequivocal TDI findings – combination of ↑natriuretic peptides & echo indices of LV diastolic function/LV filling P Paulus Wjet al -European Society of Cardiology. Eur Heart J 2007;28:2539 –50 Symptoms & Signs of HF Invasive Diagnostics • Prolonged & ↑ Tau- require sophist measurement • ↑ LVEDP /PCWP - suggested to be appropriate for ∆ of HFNEF in the presence of HF sympts & LVEF>50% • The rate of isovolumic relaxation - best measured by negative dP/dtmax at invasive catheterization • The -dP/dtmax, which gives the isovolumic relaxation rate- measured either invasively or by a CW Doppler velocity spectrum in AR • Isovolumic relaxation is ↑when rate of Ca uptake into the sarcoplasmic reticulum (SR) is ↑ • Tau- time constant of relaxation- describes rate of fall of LV pressure during isovolumic relaxation -also req invasive for precise determination Isovolumic pressure decay • Simplest way of quantifying the time course of LV pressure decline - peak -dp/dt • Peak -dp/dt - altered by myo relaxation & changes in loading conditions – For eg, LV peak -dp/dt ↑ when Ao pressure ↑ - ie, ↑ in LV peak -dp/dt from -1,500 to -1,800 mm Hg/sec could be caused by an ↑ in rate of myo relaxation, a rise in Ao pressure, or both • LV peak -dp/dt is ↓during myo ischemia & is ↑ in response to – β adr stimulation & phosphodiesterase inhibitor milrinone • It is not ↑ by digitalis glycosides Echocardiography • Currently most sensitive & widely available technique for assessment of LV diastolic function –TDI • Whereas the ratio of early to late diastolic peak mitral inflow velocities exhibits a J-shaped relationship with LVEDP, TDI velocities continuously decline from N to advanced LV diastolic dysfunction • As a consequence, E’ ↓ & E/E’ ratio continuously ↑with advanced LV diastolic dysfunction • E/E ’ ratio >15 → mean diastolic LV pressure >12 mm Hg • E/E ’ ratio >15 - ∆ of ↑ LV filling pressure and thus HFNEF • An E/E ’ ratio 8 – 15- asso with very wide range of mean LV diastolic pressures, thus, further measurements suggested • Values for E ’ at the lateral annulus are generally higher than at medial annulus, resulting in lower E/E ’ ratios at the lateral annulus Diastolic Dysfunction Grade 1 Grade 2 Grade 3 Grade 4 LV pressure Mitral flow Tissue Doppler E e’ Pulmonary vein E/e’ < 10 10 -15 >15 >15 As LV filling pressure Mitral E Annulus e E/e Nagueh et al: JACC, 1997 Ommen et al: Circ, 2000 • Measurement of velocity of mitral annular ascent during early diastole (e′vel) with TDI → relatively preload-independent measure of LV relaxation that correlates inversely with tau • E/e′ ratio is a fairly accurate predictor of the presence of elevated filling pressures Area-length method for calculation of LV mass LVmass=1.05[5/6(A1xL1)-5/6(A2xL2)] Divide by body surface area to get LV mass index Reichek et al. Circulation 1983;67:348-52 Natriuretic peptides • BNP & NT-proBNP- established tools for exclusion of possible HF in patients presenting to the emergency room with dyspnea of unclear origin • Among patients with preserved LVEF but not necessarily HF, BNP & NT-proBNP levels – related to severity of LV diastolic dysfunction • Used to distinguish a N from a “pseudonormal” LV filling pattern Treatment • Aggressive treatment of hypertension and diabetes • Diuretic therapy & dietary salt restrictions is paramount • Compelling indication for ACEI/ARBs in many patients (DM +LVH), But, – Candesartan (the CHARM-PRESERVED trial) – Irbesartan (the I-PRESERVED) – Perindopril (the PEP-CHF) Did not reveal a survival benefit VALIDD [VALsartan In Diastolic Dysfunction] study) • SBP lowering in pts with HTN & LV diastolic dysfunction • Either with a valsartan-based regimen or a regimen not including inhibitors of the RAAS • Similar reduction in BP & an ↑diastolic relaxation • Suggests that BP control may be a key factor in determining the response to treatment Solomon SD et al. Lancet 2007;369:2079–87 • The Digitalis Investigation Group • Evaluated effects of digoxin on all-cause mortality and HF hospitalization in patients with HF regardless of EF • LVEF >45% (n = 988) –ancillary study parallel to main trial • Digoxin - no effect on all-cause mortality/CV hospitalization • Trend toward a ↓ in HF related hospitalizations ↔↑in hospitalizations for UA Ahmed A et al. Circulation 2006, 114:397–403. TOPCAT trial • A trial for HF pts with preserved systolic function • Multi-center, international, randomized, double blind placebo-controlled trial • Spironolactone • 4500 adults with HF &LVEF >45% • Enrollment started -Aug 2006 & is ongoing ACC/AHA Guidelines for Treatment of Patients with Heart Failure and Normal Left Ventricular Ejection Fraction-2005 update Class l • Control systolic & diastolic HTN • Control ventricular rate in pts with AF • Diuretics to control pulm congestion & periph edema Class lla • Cor revascularization in pts with CAD in whom sympt/demonstrable myo ischemia is judged to be having an adverse effect on cardiac function • Restoration & maintenance of SR in pts with AF might be useful to improve symptoms • Class llb • Use of β-blockade, ACEIs, ARBs, or CCA may minimize heart failure sympt • Use of digitalis to minimize sympt is not well established HFNEF—the Future? • Elucidate the mech responsible for HFNEF – Ischemia, uncontrolled HTN, AF must be clearly defined – In particular, inducible ischemia must be searched actively Possible therapeutic strategies • Active relaxation - Ca uptake into the sarc reticulum - sarc reticulum Ca ATP-ase type 2 – Gene transfer –suggested possible strategy – Percutaneous delivery of a modified phospholamban encoded in an adenovirus Studeli R et al. Am J Transplant 2006;6:775– 82 • Passive LV stiffness - Advanced glycation end products cross-links breaker, Alagebrium- Pilot study in 23 HFNEF pts - ↓LV mass & an ↑ in E‘ -currently evaluated in a multicenter study Little WC et al. J Card Fail 2005;11:191–5. • Role of Sympath nervous system & RAAS in HFNEF is largely unknown given that LVH is asso with ↑sympath activity & more severe LVH seems to be asso with ↑ likelihood of HFNEF • Sympathetic NS may play a role in the pathogenesis of HFNEF • Candesartan has been shown to ↓ the sympath activity • Β-blockers & negatively chronotropic CCBs – HR lowering & prolongation of diastole results in better LV filling and output • Study evaluating purely HR-lowering agent ivabradine in HFNEF is currently ongoing