* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 10 Slides
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
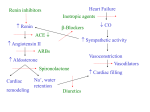
HESS 509 Chronic Heart Failure C H A P T Chronic heart failure (CHF) is a serious, debilitating, and costly non communicable condition that presently affects an estimated 5.8 million Americans. E R T E Currently, there are more than 670,000 new (incidence) cases of CHF every year in the United States; the prevalence is projected to increase to more eight million over the next 20 years. N By 2030, it is expected that one in every 33 (3%) Americans will have CHF, with the direct and indirect costs of medical management projected to increase from $39 to $70 billion per year. HESS 509 C Chronic Heart Failure Basic Pathophysiology H A P T E R T Chronic heart failure, broadly defined as the inability of the heart to adequately deliver oxygen to the body, is a not a disease but rather a clinical syndrome that affects virtually all organ systems. This syndrome occurs when cardiac output is reduced at rest, or especially during exertion, and attributable to left ventricular systolic or diastolic dysfunction or both. (not mentioned by text, but common cause is chronic hypertension.) E N Systolic Dysfunction – Impairment of left ventricular function likely due to myocardial ischemia, myocardial infarction or Idiopathic (often post-viral) Cardiomyopathy. Systolic Dysfunction causes a reduction in left ventricular ejection fraction (LVEF) and an increase in left end systolic volume. Thus, the result is a hypo-effective heart in maintaining systemic circulation HESS 509 C Chronic Heart Failure Basic Pathophysiology H A P T E R T E N Diastolic dysfunction: resistance to filling is increased in one or both ventricles, causing elevated diastolic pressure in the ventricles, generally because of reduced ventricular compliance (possibly due to scar tissue from past myocardial infarction of ventricular hypertrophy from chronic hypertension). These systolic (contractile) and diastolic (relaxation or lusitropic [rate of myocardial relaxation]) changes to heart function have both peripheral and central hemodynamic consequences. The central circulation effects include the following: • Decreased cardiac output during exercise • Compensatory ventricular volume overload (high preload) • Elevated pulmonary and central venous pressures • In severe cases, elevated left ventricular filling pressures when the person is resting Chronic Heart Failure HESS 509 C H In addition to central hemodynamic abnormalities, the reduced cardiac output in CHF results in peripheral circulatory effects as well: A P T E R • Major disturbances in skeletal muscle metabolism • Impaired vasodilation • Renal insufficiency (from poor perfusion), leading to • Abnormal neuro-hormonal responses, and • Pulmonary – ventilatory dysfunction T E N The consequences of this constellation of physiological changes result in the cardinal signs and symptoms of CHF: • • • • Fluid retention (resulting in pulmonary or peripheral edema) Orthopnea (due to pulmonary edema) Dyspnea on exertion (also from pulmonary edema) Fatigue (generalized or localized to leg skeletal muscles, or both) Reduced exercise tolerance (from all the above Chronic Heart Failure HESS 509 C H A P T E R T E Management and Medications Treatment of Chronic Heart Failure Treatment for people with CHF has several key features: • • • • Identifying and treating the underlying causes and risk factors Regulating sodium and fluid balance Pharmacologic therapy to reduce symptoms Reducing adrenergic stimulation (decreasing cardiac stimulation and afterload) N As CHF becomes more and more severe, more invasive approaches to managing symptoms include the following: (see text for details on each category below) • • • • Oral or infused inotropic agents to improve contractility Ventricular pacing to improve cardiac performance Left ventricular assist device implantation Cardiac transplantation HESS 509 C H A P Chronic Heart Failure Effects on the Exercise Response The CHF syndrome results in a number of central, peripheral, and ventilatory abnormalities that adversely influence the exercise response, irrespective of the cause of CHF, including these: T E R T E N • Reduction in cardiac output • Mismatching of lung ventilation to perfusion (perfusion to ventilation ratio), causing shortness of breath • Leg fatigue during exercise due to inadequate blood flow to skeletal muscle Altered baroreceptor reflexes have also been observed and may contribute to diminished chronotropic responses or to reduced systolic pressure and reduction in peripheral perfusion. Peripheral abnormalities, including the following, also influence the response to exercise in individuals with CHF • Reductions in muscle blood flow • Abnormal redistribution of blood flow • Reduced vasodilatory capacity • Endothelial dysfunction • Abnormal aerobic metabolism biochemistry in skeletal muscle Chronic Heart Failure HESS 509 C H A P T E R T E Effects on the Exercise Response Abnormalities in skeletal muscle metabolism include reduced mitochondrial enzyme activities, reduction of type I aerobic fibers and reduced contribution of oxidative phosphorylation; the result is more metabolic acidosis. As a consequence of these central and peripheral maladaptation, exercise tolerance and quality of life are dramatically reduced in people with CHF. They achieve only ~50% of the age-predicted VO2peak of healthy individuals, impairing their ability to participate in activities of daily living N Journal Article - Congestive Heart Failure More Bad News From Exercising Muscle? HESS 509 C H A P T E R T E N Chronic Heart Failure Effects of Exercise Training Improvements after endurance training in CHF because of peripheral adaptations: • Improved skeletal muscle metabolism (strength training may also be of benefit to help prevent muscle wasting) • Improved endothelial function • Increased vasodilatory capacity and redistribution of cardiac output These peripheral changes overshadow central hemodynamic changes, which include cardiac chamber volumes, ejection fraction, and pulmonary pressures at rest and during exercise. Exercise therapy for individuals with CHF improves physical functioning, quality of life, and morbidity and mortality. HESS 509 C H A P T E R T E N Chronic Heart Failure Recommendations for Exercise Testing Exercise testing can be valuable in objectively characterizing the severity of CHF and evaluating the efficacy of therapeutic interventions. The standard exercise ECG usually offers little insight, and exercise intolerance can be more appropriately characterized via these methods: • Respiratory gas exchange response to exercise • Quantification of work capacity • Identification of the pathophysiological abnormalities HESS 509 C H A P Chronic Heart Failure Recommendations for Exercise Testing The following considerations relate to exercise testing with this population (see also table 10.1 – next slide): T E R T E N • Symptoms are frequently observed under 5 metabolic equivalents (METs). • Lower-level, moderately incremented, individualized protocols are recommended (Naughton or ramp). • Unstable or acutely decompensated CHF is a contraindication. • Respiratory gas exchange measurements (including VO2peak, VT, VE/VCO2 slope) increase precision, optimize risk stratification, and permit assessment of breathing efficiency and patterns. • Six-minute walk tests supplement the graded exercise test but are not a surrogate for measured respired gas analysis. • Exertional hypotension, clinically significant dysrhythmias, and chronotropic incompetence may occur in CHF, so 12-lead ECG should be monitored during testing. • Test endpoints should focus on symptoms, hemodynamic responses, and standard clinical indications for stopping (not a target heart rate). HESS 509 Chronic Heart Failure C H A P T E R T E N Exercise Testing Considerations for CHF (FYI) HESS 509 Chronic Heart Failure C H A P T E R T E N Recommendations for Exercise Programming Most individuals with CHF should: • Be referred to cardiac rehabilitation, • Follow the Basic Exercise Prescription Recommendations, • and graduate to a home-based program aimed at maintaining physical functioning. Potential complications and outcomes for individuals with CHF differ significantly compared to the standard cardiac rehabilitation population, including the following: • • • • Many individuals with CHF will deteriorate irrespective of interventions. Risk of sudden death is higher. Prevalence of psychosocial and vocational problems is higher. Some individuals experience prolonged fatigue after only a single exercise session. Absolute contraindications to exercise in CHF include: • Left ventricular outflow obstruction • Decompensated CHF • Unstable dysrhythmias Chronic Heart Failure HESS 509 Special Considerations for CHF C H A P T E R T E N • Status can change quickly, and clients should be reevaluated frequently for signs of acute decompensation, rapid changes in weight or blood pressure, worse than usual dyspnea or angina on exertion, or increases in dysrhythmias. • Warm-up and cool-down sessions should be prolonged. Some clients may tolerate only limited work rates and may need lower-intensity and longer-duration exercise sessions. • Duration of activity may need to be adjusted to allow clients more opportunity to rest and to progress at their own pace. • Some clients may better tolerate discontinuous training involving shorter sessions of exercise interspersed with periods of rest. • Perceived exertion and dyspnea scales should take precedence over heart rate and work rate targets. • Isometric exercise should be avoided. • Electrocardiogram monitoring is required for persons with a history of ventricular tachycardia, cardiac arrest, or exertional hypotension. • Consider ancillary study data (e.g., exercise echocardiogram, radionuclide studies, hemodynamic studies, ventilatory gas analysis) when developing the exercise program. In general, do not exceed a work rate that produces wall motion abnormalities, a drop in ejection fraction, a pulmonary wedge pressure greater than 20 mmHg, or the ventilatory threshold. END