* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download A Look Into Congestive Heart Failure
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Rheumatic fever wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
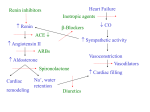
A Look Into Congestive Heart Failure By Tim Gault Definition • Congestive heart failure (CHF) is a condition in which the cardiac muscle does not pump blood efficiently through the circulatory system. Causes • The causes of congestive heart failure can vary greatly. • All forms of heart disease can lead to heart failure Primary Disorders • Cardiomyopathy • Heart muscle disorders cause the heart to lose its contracting ability. • Common conditions include coronary atherosclerosis, arterial hypertension, and inflammatory or degenerative muscle disease. Dysrythmias • The heart cannot properly contract. • Some of these conditions include tachycardia, atrial dysrythmias, and asynchronous contractions. Systolic and Diastolic Heart Failure • In diastolic dysfunctions of CHF the heart is unable to relax and there is abnormal filling of the ventricles. • Systolic dysfunctions are due to the heart being unable to create a force great enough to eject blood normally. • The left ventricle systolic dysfunction is the most common cause of CHF, occurring in 60% of patients Secondary Disorder • CHF can also be caused by other systemic alterations such as an increase in metabolic rate, hypoxia, hypoxemia, and anemia. • These problems require the heart to increase the cardiac output to meet the need for more oxygen. • This causes the heart to lose some of its oxygen supply increasing the risk of CHF. Pathogenesis • The first problem that occurs in the heart is a lesion to the heart muscle itself. This results in the heart being unable to cause the correct amount of velocity for the load placed on the heart. • Once this occurs and cardiac output is decreased the compensatory mechanisms kick in. • These mechanisms include the sympathetic mechanism, renin-angiotensin system, and ventricular hypertrophy. • These mechanisms include the sympathetic mechanism, renin-angiotensin system, and ventricular hypertrophy. • Sustains cardiac function for a while. • Lead to a feed-back loop causing more cardiac failure . Symptoms • A patient with CHF will notice several different changes in their bodies. • One of the most common signs of CHF is swollen legs or ankles and difficult breathing. Signs • The physician will listen to the heart for distinct sounds that can indicate CHF. • The patient might be tachycardic, pale in color, have inspiratory rales, or heart murmurs. • If the physician hears murmurs, it can indicate that there is mitral or tricuspid regurgitation. Diagnostic Tests • Echocardiography: Most useful test for diagnosis. • Uses sound waves to see a moving picture of the heart. • Able to distinguish between systolic and diastolic dysfunction. • Cardiac Catheterization checks the coronary arteries for atherosclerosis to see if it is the cause of CHF. • Exercise Stress Test gives an overall view of how well your heart is performing under stress. Treatments for CHF • Beta-blockers stop the sympathetic nervous system from activating. • This will prevent the release of catecholamines, which in turn will reduce heart rate, blood pressure, and contractility. • Calcium channel blockers: Help to control the myocardial cells involved in pacing the heart. • The result of this agent is a decreased heart rate, contractility, and causes vasodilatation. • Nitrates: Dilate the arteries and the veins in the heart reducing the filling time for the ventricles as well as increase cardiac output. • Ace Inhibitors: Blocks the renin-angiotensin mechanism. • Improve mortality, heart failure symptoms, left ventricle ejection fraction, as well as exercise tolerance. • Heart Rate Recovery (HRR) • Experimental program which tries to improve the heart rate in patients with CHF. • Short term aerobic exercise showed an increase in the HRR in some patients that were unable to exercise very well. Outcome • Patients who have heart failure will have a low chance of survival. • 50% of patients with severe heart failure will die within 12 months and those with moderate CHF will die within 3-4 years. • About 30-40% of patients will die suddenly with CHF and those with left ventricle dysfunction have a mortality rate of 10% per year.