* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Digestion is fundamentally a three stage process that begins with
Survey
Document related concepts
Transcript
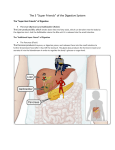
Digestion is fundamentally a three stage process that begins with the initial breakdown of food in the mouth and stomach. It continues through the small intestine where foods are broken down into minute particles and simultaneously absorbed. The process is completed in the large intestine with the re-absorption of water and the elimination of feces. Any dysfunction in any of these three stages decreases our intake of nutrients, compromises other systems of the body and can affect the intestinal environment seriously enough to foster more serious problems. This mechanical and enzymatic process of breaking foods down and absorbing their nutrients yields waste products and toxins. The integrity of the digestive tract tissue must be intact to prevent these toxins from entering the blood stream. If the strength of the intestinal tissue is compromised, toxins are able to filter into the bloodstream. Over time, this weakens the body and makes it conducive for many illnesses. Breakdowns in the digestive process and protective barrier of the intestinal tract are responsible for the vast majority of today’s health problems including cancer, arthritis, autoimmune diseases, allergies, asthma, eczema, chronic fatigue and recurring infections, especially in children. How does one know if this is relative to them? Even the mildest of digestive symptoms which we accept as “normal” may be reflective of digestive imbalances. For example, any form of bloating or distension within 30 minutes or 2 hours of eating signals an incomplete or imbalanced digestive process. Other signs may include malodorous stools, undigested food, mucous or blood in the stool, flatulence, bad breath, coating on your tongue, light-colored or green stools, constipation (inability to move your bowels 1-2 times daily) and/or incomplete evacuation. Chronic inflammation is almost always an indicator of bowel dysfunction. These symptoms may be reflective of minor imbalances that require changes in ones diet or possibly an adjustment in combining the proper foods together. The removal of certain foods that elicit allergic or hypersensitive reactions may be warranted. In more serious situations it may signal a decrease in your body’s ability to produce adequate levels of digestion chemicals, the possibility of pathogens such as parasites or a condition known as candidiasis (fungal overgrowth), malabsorption or an inflammatory state of the bowel (quite often, several of these conditions are found together). Phase 1: Digestion begins in the mouth. The mechanical action of chewing serves several functions. It tears the food into small pieces, thereby increasing its surface area. This gives the acids and enzymes greater access to work more effectively on the food. Simultaneously, it releases enzymes that start the digestive process immediately. The saliva secreted serves as a lubricant and makes it easy to swallow the food. Finally, there is the cephalic response. This is a brain signaling mechanism that prepares the body for food. It is involved with the quality and quantity of saliva produced, thermogenesis, insulin and glucagons response (see article on insulin for its importance) and the full spectrum of digestion, absorption and utilization. Once the food enters the stomach it signals for the release of Hydrochloric acid (HCl) and a protein digesting enzyme called pepsin. The acid kills harmful microbes (viruses, bacteria etc.) and churns the food into a liquid-like substance termed 'chyme'. There is also a mechanical-type contraction of the stomach that assists in this phase and subsequently passes the chyme into the small intestine for phase 2 of digestion. If there is a deficiency in the chemical production of the stomach, it will diminish the efficacy of the entire digestive process because phase 2 is dependent upon the acidic nature of the chyme. It is the acid content of the chyme that sends signals to the gall bladder and the pancreas to perform the next phase. When HCl production is decreased, it compromises the rest of digestion. This is noted by gas, bloating or indigestion within 30 minutes of eating, bad breath, a coated tongue, acid reflux possibly and the sense of hyperacidity (Hyperacidity is not common. It usually results from long term hypoacidity and irritation to the mucosal lining of the stomach due to poor mucous production. Without this mucosal protection, any amount of acid can create irritation.). HCl is also necessary for vitamin B-12 and iron absorption. Decreased levels may lead to anemia. Some other signs may include constipation, ridged fingernails, undigested food particles in the stool, allergies, arthritis, and sinus problems. Influences on HCl production include the bacteria H. pylori (often involved with gastric ulcers), hypoglycemia, malabsorption syndrome, adrenal and thyroid dysfunction and deficiencies in vitamin B6 and zinc. Correction of these conditions should be done before the use of HCl becomes apart of anyone’s regular program. It is important to recognize our ability to produce HCl decreases as we get older. This is one of the contributing factors why digestive problems get worse with age. Supplementation with the various forms of HCl can be of benefit. Temporary use of HCl may be part of the solution, but for younger people, it should not be part of any permanent regimen if possible. For the elderly, it may be in their best interest to make it a regular part of their nutrition program. However, it is better to establish healthy eating habits and correct any form of bowel dysfunction than to rely on HCl supplementation. Phase 2: As the chyme enters the small intestine, numerous signals are sent off simultaneously. The pancreas is stimulated to perform two digestive functions. First, it produces and releases bicarbonate into the small intestine. This helps to protect the small intestine by making the pH level more alkaline and neutralizing the acid content of the chyme. The second job of the pancreas is to produce and release digestive enzymes into the small intestine. These substances continue the digestive process and break down the fats, proteins and carbohydrates into tiny particles to be absorbed through the intestinal lining and into the blood and lymph vessels. These substances will go through scores of biochemical changes before they are eventually used by the cells of the body. These pancreatic enzymes are most effective when the pH is at the proper alkaline level. If the pancreas is unable to produce the necessary bicarbonate level or if it is not properly stimulated because of a deficiency of HCl production from the previous stage, then the enzymes will be unable to fulfill their function efficiently. Typically, those with decreased enzyme function will develop bloating, gas, and/or abdominal distension within 45 minutes to two hours after eating. They may have undigested food in their stool, constipation, diarrhea, fatigue, food allergies or sensitivities, skin conditions, and floating stools. Usually, the use of a plant derived, broad spectrum enzyme formula proves effective. It is believed that overeating and poor food choices contribute to poor enzyme production. Assisting the pancreas during this phase is the gall bladder. The gall bladder is the storage area for bile. Bile is produced by the liver and serves two basic functions. When acid or fat enters the small intestine, it signals the production of a chemical called cholecystokonin (CCK) that signals the gall bladder to release its bile. Upon release, the bile enters the small intestine and helps the bicarbonate create an alkaline environment for the enzymes. At the same time, the bile also emulsifies the fats. This breaks the fats into small particles, allowing the fat-digesting enzymes (known as lipases) better access to them, increasing enzyme efficacy and fat digestion. The second function of the gall bladder involves detoxification. As toxins are neutralized by the liver, they are excreted in the bile. When the bile is released in the digestive process the toxins are excreted with it and removed in the feces. Any compromise in the liver’s ability to produce bile or the gall bladder’s function to release the bile increases the toxicity of the body and increases the risk of many illnesses. The traditional warning signs that determine who is in the high risk category for gall bladder problems are the four Fs: female, fat, fertile and over forty. A main reason for these factors is their relationship to estrogen metabolism problems, i.e. PMS, fibroids, endometriosis, ovarian and breast cysts etc. Obesity (fat) (Obesity primarily results from insulin dysfunction-see articles on blood sugar regulation and stress) is involved because the extra body fat now becomes a second sight that produces estrogen (female & fertile). This excess estrogen, along with the imbalances created by bad food selection, increases the toxic load for the liver and gall bladder. As we get older (over 40), our poor life-style habits catch up with us. Eventually, the liver is depleted of its reserves and can no longer detoxify adequately. The bile becomes viscous and becomes more difficult to excrete. This may pre-dispose a person to form gall stones. Toxins also remain in the system too long and place an increased burden on this already overworked process, hindering it even further. Other contributing risk factors to gall bladder dysfunction appear to be a diet containing high levels of fats, low fiber intake and refined carbohydrates and stress. Important signs of a gall bladder problem include light or clay-colored stools, headaches, usually above the eyebrows along the frontal sinuses, an inability to handle greasy foods, pain along the right shoulder blade area, tenderness to the right thumb web area when palpated firmly, possible discomfort under the right rib cage area, skin conditions, hemorrhoids, bowel dysfunction and jaundice. A common ailment previously mentioned is gall stones. If left unattended, they can lead to serious problems including pancreatitis. However, surgery is usually not the best way to remedy the situation. Many alternative practitioners have developed expertise it “flushing out” the stones through specific programs. That remedy is beyond the scope of this article and should never be tried without being under the supervision of an experienced practitioner. Any flushing program needs to be accompanied with lifestyle changes regarding diet, exercise and stress management. However, the use of phosphatidyl choline, have been utilized to keep the bile thin, allowing it to exit the gall bladder more easily and perform its function. Other remedies include vitamin C, taurine, beet root concentrate, pancreatic enzymes, specifically lipases, dandelion and milk thistle. Dietary changes are critical and a decrease in dietary fats and refined carbohydrates, accompanied by an increase in quality fiber is the first step. Those who have had their gall bladder removed need to keep their bile thin and possibly take bile salts. The inability to produce these salts places the individual at a higher risk for colon cancer. Before supplementing yourself, please check with your practitioner. Phase 3 After the small intestine completes its job of breaking down the food and absorbing the nutrients, it passes the remaining chyme to the large intestine through a sphincter termed the ileocecal valve (ICV). Proper function of this sphincter is critical to the well-being of the digestive tract because it regulates the chyme entry into the colon and protects the small intestine from the backwash of bacteria from the large intestine. As the chyme passes through the large intestine, the body reabsorbs water from this mass (up to 2 liters/day) and stores the fecal material in the distal part of the colon until the signal to defecate is given. The large intestine is colonized by bacteria collectively termed microflora (MF) (MF lives throughout the entire digestive tract, but it is predominant in the large intestine.). A healthy adult’s gut will contain approximately between 5 to 15 pounds of MF. There are over 400 different forms of these bacterial microorganisms, both friendly and harmful, and there numbers total in the trillions. The symbiotic balance between these groups of bacteria is critical to one’s health. Stool is largely comprised of these bacteria. The MF breaks down the fiber in our foods and produces short-chain fatty (SCFA) acids as part of its metabolism. SCFA are the fuel supplied to the colon cells to keep them functioning. This is one of the reasons fiber is so critical to our health. It provides the substrate by which nourishment for the colon cells is provided. This in turn creates a healthy environment for the MF to flourish. Though this feedback mechanism may appear simple, it is highly regulated and influenced by the previous stages of digestion, diet, stress, food quality, environmental factors, toxicity etc. It is critically important because research has shown that individuals who develop serious bowel ailments, i.e. colitis and colon cancer, have a markedly decreased level of these SCFA in their systems. The MF is also responsible for the production of certain B vitamins i.e. pantethine, choline and vitamin K. Imbalances in the MF colonies can lead to nutrient deficiencies and affect many biochemical pathways that utilize these nutrients. Other benefits of MF are its ability to limit the numbers of unhealthy microbes, support the immune system and reduce the harmful effects of cholesterol. Disturbance in the ecological balance of these MF colonies is called dysbiosis. It is reflective of and a contributor to a compromised immune system. In addition to the above mentioned functions being impaired, dysbiosis is involved in many of today’s serious illnesses including cancer, autoimmune diseases, allergies, asthma, IBS, chronic fatigue syndrome, recurring infections, and learning disorders in children. Though gut ecology is overlooked by mainstream health care professionals, its integrity can not be emphasized enough. Dysbiosis results from any one or combination of influences. Starting with poor dietary habits and the overconsumption of refined foods, many of the contributing factors include too much alcohol, stress, laxatives, NSAIDS, birth control pills, poor digestion, metal toxicity, formula fed babies, and acquired food sensitivities and allergies from all the above stressors. In infants and children, cow’s milk, dairy and refined carbohydrates are the main culprits. Also, giving infants solid foods prematurely, especially animal proteins and grains, can disrupt the developing intestinal tract. Sanitary and environmental conditions, trauma, infections, radiation, chemotherapy, age, and genetics may also contribute to this malaise. But the most common denominator causing dysbiosis is antibiotics. When antibiotics are given to attack any invasive bacteria, it can not discriminate between the beneficial bacteria of the body (MF) and the invading pathogen. It will eliminate any form it comes in contact with. This diminishes the colon’s functional capacity. It is especially harmful in children because the function of the GI system is not fully developed and is much more susceptible to insults. And what is so critical is that approximately 60% of our immune system resides in the gut. This aspect of the digestive tract is known as the GALT: gut-associated lymphoid tissue. GALT The GALT consists of specialized cells and lymphatic tissue in the gut lining. These specialized cells produce antibodies and are our first line of defense. These antibodies, known as Secretory IgA (SIgA), exist wherever there is mucosal tissue, including the mouth. SigA will attack anything it perceives as a potential threat. In conjunction with other specialized cells in the gut lining and blood, the GALT determines which food nutrients are allowed to pass through the gut wall into the body. Simultaneously, it neutralizes and removes invading pathogens and food particles too large to cross the intestinal barrier. When this capability is diminished, pathogens can pass through the intestinal barrier and different types of reactions can occur. If the immune system overreacts, food allergies and asthma are possible consequences. Sometimes, the immune system can not recognize the difference between the body’s tissues and the invading pathogen. In turn, it attacks the tissue it believes to be the pathogen i.e. the myelin sheaths of nerves are destroyed in multiple sclerosis, intestinal tissue in Crohns, etc. And when the immune system is too weak to defend the body properly, it can not protect against illnesses such as cancer. Healthy development of the GALT starts at the moment of birth. In utero, the baby’s digestive tract contains no MF and is sterile. As the baby exits the vaginal canal, it is exposed to the bacteria of the mother’s vagina and the rectum. This stimulates the infant’s immune system to start producing its own MF, primarily bifidobacterium. This process is carried on via breast feeding (There is evidence that shows formula-fed babies have a greater susceptibility to infections from microbes causing diarrhea.). Breast milk contains peptides, immune factors, fats, and nutrients necessary for the infant’s development, including the maturation of the digestive system. As the child is weaned from breast milk and starts to eat solid foods, a different form of flora, typical for an adult, develops. This is of the lactobacillus variety. Maintenance of the GALT does not end with infancy or childhood. Our lifestyle choices have a direct impact on its integrity. Diets consisting of large quantities of vegetables and moderate amounts of whole grains and fruits will provide a good source of fiber for the MF and assure It was mentioned that antibiotics are the most common disruptive force to the MF and GALT. This is most clearly seen with children suffering from recurrent ear infections. With each episode, they are given a course of antibiotics. Though the medication temporarily knocks out the infection, the child’s digestive and immune system are actually weakened by the antibiotics. This sets up an environment more conducive for the next infection to take hold. And with each subsequent infection and round of antibiotics, these systems function at a diminished capacity, making the child even more susceptible to get sick. It becomes a vicious, negative feedback cycle. These individuals are the most likely candidates for digestive and chronic illnesses during childhood and as an adult. Some children have received so much antibiotic therapy their body no longer responds to treatment because there immune systems have been too highly compromised by the overmedication. Too often the bacteria have developed a resistance. These are the children who end up with surgery to place tubes in their ears to provide drainage and hopefully stop further infections. Yet this never addresses the original problem of a weakened digestive-immune system and further cripples it by not correcting the damage inflicted by the antibiotics. To further elaborate on this relationship between antibiotics, the digestive system and health, the Journal of the American Medical Association recently released their findings of a study conducted with a Seattle-based health plan that enrolled more than 10,000 women over a 17 year period. They found that the higher the antibiotic use, the higher the risk of breast cancer. Newsday reports, “One explanation for the increased cancer risk could be that antibiotics can alter bacteria in the digestive system, possibly interfering with the metabolism of foods that fights diseases”. Anytime antibiotics are used, the eliminated MF must be replaced. The most common replacement is lactobacillus acidophilus and bifidobacteria. If there is diarrhea associated with the antibiotic regimen, S. boulardii works well. These should be taken on an empty stomach (30 minutes prior to eating or 2-plus hours after eating; some prefer before bed and upon arising) for a minimum of two weeks. Increased fiber intake should accompany MF replacement. Many products come with FOS orinulin to provide nourishment for the MF. At first, FOS may produce gas. If so, reduce the amount and slowly build up over a few weeks. Eventually the gas subsides. If not, it may indicate a more severe dysbiosis and need further examination. Long term antibiotic therapy may require more than MF replacement. The integrity of the intestinal lining may be highly compromised and require more serious, individualized attention. Leaky Gut Syndrome When the lining of the gut has been compromised sufficiently, it becomes porous, allowing toxic particles to enter the blood stream. At this point, the SigA and GALT can no longer keep up with the toxic load. This leads to inflammation of the intestinal wall, exacerbating the condition and further permitting more toxins and large food particles entrance into the blood. This is quite often the scenario in food allergies and sensitivities and can be the trigger for autoimmune problems. The increased toxic burden is handled by the liver (see article in detoxification). As the liver cleans up the overload, toxic by-products are produced. Normally, these substances are neutralized by the reserves of the liver. With the excess of toxins demanding attention, these reserves can become depleted and the normal detoxification process hampered. This can lead to local problems such as gall stones or set the stage for systemic illnesses including cardiovascular disease, arthritis and cancer. As the gut inflammation increases, malabsorption is a natural consequence. The vital nutrients for maintaining a healthy gut wall are limited. This accelerates the gut lining destruction, increases the leaky gut phenomena and deprives the rest of the body from some of its basic nutritional needs. Other conditions associated with leaky gut are chronic fatigue, eczema, chemical sensitivity, joint pains, emotional symptoms and ADD. Since there is a strong overlap between dysbiosis and a leaky gut, many of the same causes and symptoms are shared. A good way to differentiate is through laboratory testing. Leaky gut is verified by a lactulose/mannitol test. After fasting, you drink a solution containing two different types of sugar molecules, one larger than the other. Urine is then collected for the next six hours. In a healthy gut, the large molecule (lactulose) is not absorbed and excreted in the urine. Mannitol (small molecule) should be absorbed and show up low in the urine. The ratio of the two sugars is examined. If it is skewed towards the lactulose, leaky gut is confirmed. There are also tests for dysbiosis. This is usually done through stool analysis. Quite often both problems are present. Candidiasis One common form of dysbiosis is the overgrowth of the microorganism Candida albicans. Candida competes with the lactobacillus and bifidobacteria for space on the intestinal wall. Their numbers are small so usually there is no harm. When the MF is destroyed by antibiotics or any of the other stressors, candida will make the most of the opportunity and expand its colonies. An overgrowth occurs and when the numbers become large enough many symptoms arise, complicating ones health and diagnostic picture. Diagnosis can be difficult in some cases. Stool tests are not one hundred percent reliable. Sometimes a urinary indican test will pick up candida when a stool test can not. There are times when both are insufficient and the practitioner must use their clinical experience to interpret the individual’s symptoms. There are many remedies on the market to combat candidiasis. Most individuals require more than one and need to be monitored for efficacy. Symptom reduction is not enough. There are times when the remedies can contain or control further growth of the organism. This allows you to feel better but is not necessarily corrective. After a certain period of time re-testing is necessary to determine the microorganism status. As a reduction in candida is indicated, intestinal repair must be done to restore integrity to the intestinal tract. This needs to be accompanied by MF replacement. How this is accomplished can vary widely from individual to individual. During this time dietary measures must be followed. Candida thrives on sugars. All refined foods must be eliminated. The vast majority of fruits should be avoided. In severe cases no fruits should be consumed. Small amounts of legumes and whole grains (avoid gluten foods) are allowed with proteins and vegetables. If severe, grains should also be eliminated and legumes monitored. Avoid dairy. Treating candida is not as simple as it sounds. Remember, there are usually multiple problems occurring simultaneously. One further complication can be parasites. Parasites Parasites are microorganisms that can trigger any of the aforementioned problems. If all the therapeutic attention is directed at eliminating these ailments, correction may be somewhat palliative but will fall far short of any lasting corrections. The parasites will continue to harbor in the intestinal tract preventing any remedies from being effective. Diagnostic testing involves stool and saliva samples. Microscopic stool examination searches for the actual organism. This is not one hundred percent reliable due to collection techniques, laboratory methodology and location of parasitic infestation. The saliva test reveals antibody production in response to the organism. It can be a more sensitive test. Even if the stool inspection is negative, if the antibody test is positive, it indicates the presence of a parasite. Parasites can also be detected through blood and urinary organic acids. Parasite infections have been on the rise. Factors that place you at a higher risk are: • Eat out often • Eat at salad bars for meals • Drink from well water • Have pets • Eat sushi • Travel to other countries i.e., tropical islands • Past history of food poisoning • Use of public swimming pools • Any form of anal sex Parasites often require strong herbal remedies and sometimes antibiotics. All antibiotic therapies must be followed with MF replacement (this holds true for herbs too). Dietary protocol is not as limiting as the candida restrictions (unless candida is also present), but dairy is totally forbidden. Remain off all refined foods. Whole grains, fruits and legumes are permissible. Gluten/Gliadin Intolerance Gluten is a protein found in a variety of grains including wheat and oats. It will create inflammation of the intestinal tract and cause malabsorption. If it is left undetected, it can lead to very serious health issues. Symptoms are similar to those previously mentioned and include weight loss, failure to thrive and a chronic sensitivity to the smallest amount of food with gluten. Approximately ten percent of those afflicted develop a bumpy, itchy skin rash. This condition is not correctable. Foods with gluten must be avoided permanently. Removal of these foods will allow the body to repair when given the proper therapeutic modalities. Gliadin is a tri-peptide molecule within the gluten protein. Its ramifications may not always be as severe but it does cause inflammation, disrupt the intestinal tract and lead to the same dysfunctions. Generally, once the imbalances caused by thegliadin sensitivity are corrected, these foods can be re-introduced into the diet in small quantities without causing any further problems. Those with gluten intolerance are not so fortunate. Gluten foods should be eliminated permanently. With any ongoing digestive disturbance you should be tested for both sensitivities. Hopefully this gives you an idea of the inner workings and complexities of the digestive system. Before starting any program, try to educate yourself in regards to eating healthy, stress reduction and developing a sound exercise regimen. Make small incremental changes and set reasonable short term goals with a long term goal in mind. Many times our complaints will decrease by some basic changes. If you find the results you are getting are not satisfactory, seek out help. Support groups and the referrals of friends can be a valuable source of information and guidance. If you are on any medications and make changes, please inform your doctor.