* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download EKG
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Jatene procedure wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
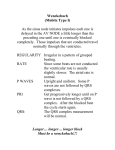
Basic EKG interpretation Janie McCloskey, RN, MSN Objectives Explain the relationship between mechanical and electrical events in the heart Interpret basic dysrhythmias generated from the SA and AV nodes as well as the atria and ventricles Describe appropriate interventions for common dysrhythmias Explain the basics of cardiac pacing Basic Cardiac Review Heart is a muscular organ behind the sternum between the 2nd and 6th rib Bottom tip points the left and is called the apex The atria lie to right Major function is to circulate blood 4 chambers atrial septum ventricular septum Basic Cardiac Review Septa divide the heart into 2 pumping systems, the right and left heart Right heart pumps blood to the pulmonary circulation. Left heart pumps to the body. The heart contracts and relaxes in an organized rhythm by mechanical and electrical factors. Mechanical Activity of the Heart Mechanical power comes from muscular contractions: diastole and systole Diastole occurs when the ventricles receive blood from the atria Systole is the contraction of the ventricles to send blood to the PA and the aorta. Systole and Diastole occur simultaneously between the right and left sides of the heart. Electrical Activity of the Heart Automaticity is the ability of cardiac cells and muscle to generate its own electrical activity Cardiac Conduction System transmitselectrical impulses to cause the heart to contract. Electrical Activity of the Heart Electrical activity is divided into 2 phases: Depolarization-a stimulated state (contraction) Repolarization-a recovery state Depolarization and Repolarization occur because of a cellular shift of – and + charged ions in and around myocardial cells. Electrical Activity of the Heart At rest, K+ in greater amounts intracellularly and Ca+ and Na+ are in greater amounts extracellularly When the cells are electrically stimulated, they change their permeability. Sodium and calcium enter the cell quickly Potassium moves out of the cell Depolarization/Repolarization Depolarization is the active electrical phase associated with systole Toward the end of depolarization, Na stops shifting, Na and K are returned to their proper places to allow the heart to repolarize and wait for the next depolarization Repolarization is a resting state of the muscle when the ventricles fill known mechanically as diastole Refractory Periods Absolute Refractory Period is when cells have depolarized and are starting to repolarize. No impulse can be conducted to cause a contraction Relative Refractory Period is a vulnerable time for the heart Cells are repolarized to the point that a strong electrical impulse would result in contraction Electrical Conduction Components Sinoatrial Node (SA Node) Atrio-Ventricular Node (AV Node) Ventricular System (His Purkinje System) Bundle of His R and L Bundle Branches Purkinje fibers Electrical Conduction Components SA Node Located in RA where the superior vena cava joins the atrial tissue mass The heart’s pacemaker Initiates 60-100 bpm Depolarization and simultaneous contraction of the atria cause a P Wave. Electrical Conduction Components AV Node located in lower R atrium Only “normal” conduction pathway between atria and ventricles Delays transmission of impulse from atria to ventricles to allow ventricles to fill Acts as a back up pacemaker 40-60bpm Electrical Conduction Components Bundle of His: Thick cord of nerve fibers in the first 1/3 of the ventricular septum Divides into 2 bundles R bundle branch has 1 fascicle L bundle branch has 2 fascicles: anterior/superior posterior/inferior Electrical Conduction Component Purkinje Fibers Network that carries electrical impulses deep into ventricular muscle Can also provide an intrinsic rhythm of 20-40 bpm if the nodes fail to conduct and impulse. The His Purkinje System Activates ventricular depolarization - contraction of the ventricles seen as QRS complex Rate of Pacemakers SA node 60-100 BPM AV node 40-60 BPM Ventricles 20-40 BPM EKG’s Monitor electrical activity of the heart on graph paper 12 lead EKG (diagnostic) Continuous cardiac monitoring 5 lead monitoring (most critical care units) 3 lead monitoring (ER’s and Telemetry) Leads Lead refers to the electrodes placed on the patient’s skin to record the electrical activity Each waveform is representative of an electrical event in the heart Leads have conductive adhesive to ensure a good tracing of electrical activity Lead position will determine whether the waveforms are positive or negative Telemetry Monitoring 5-lead or 3-lead system Most common positions are Lead II or MCL1 upright P and clear QRS views Modified Chest lead simulates V1 6 second strips are run at the start of each shift, specific hourly intervals, and prn EKG Paper EKG paper is a collection of small squares inside large boxes. Time is measured horizontally 1 small square = 0.04 seconds There are 5 small squares to each large box 5 squares x 0.04 seconds = 0.20 seconds 1 large box which is dark line to dark line is equal to 0.20 seconds Measuring Time Slashes on the top of the graph paper mark the time There are 15 boxes between each slash mark (15 x 0.20 seconds = 3 seconds) Space between 1st and 2nd slash = 3 seconds Space between 1st and 3rd slash = 6 seconds Measuring Voltage Voltage is measured vertically There is an imaginary baseline called the isoelectric line where the voltage is at zero 1 small vertical square = 0.1millivolt(mV) and 1mm2 1 large square = 0.5 millivolt (mV) 5mm2 EKG paper: how to measure •Each small box = 0.04 sec •Each large box = 0.20 sec •Each small box = 0.1 mV •Each large box = 0.5 mV 0.1 mV 0.5 mV The Cardiac Cycle - ECG Electrical activity can be graphed and measured on paper. Each waveform is related to an electrical event in the heart. Changes in the waves and measured segments indicate alteration in normal electrical conduction system P Waves SA Node fires an impulse to depolarize the atria P waves indicate Atrial Depolarization Rounded in shape, usually upright Usually no more than 0.3 mV high Changes can mean the impulse came from somewhere other than SA node. Absence can mean SA failure See page 7 in graphics booklet PR Interval PR interval = total time of atrial depolarization From the SA to the AV Node impulse is delayed before reaching the bundle of His It is a pause after the P, tracing returns to the isoelectric line Normal PR interval is 0.12 – 0.20 seconds Measured from beginning of P to start of QRS QRS Complex QRS complex is caused by ventricular depolarization Q is the first negative deflection (if present) R is the first upward stroke usually tall S is the negative stroke after the R Normal length of QRS is 0.04 – 0.12 seconds * < 0.12 (Sole 0.06 - 0.10) Wide QRS indicates conduction problems in the ventricles QT Interval QT Interval measures the time for ventricular depolarization and repolarization QT Interval is from the beginning of the QRS complex to the end of the T wave The slower the HR, the longer the QT (usually 0.32-0.44) Not used in Rhythm determination ST Segment Connects the QRS complex with the T wave Segment not a wave Should be isoelectric ST depression is ischemia medication Not measured by itself, but incorporated into the QT interval T Wave Represents ventricular repolarization Ventricles recover rapidly causes a T Wave Occurs after the QRS complex Usually positive, broad, and rounded waveform T waves are not directly measured Relative refractory period Interpreting Rhythms 6 Easy Steps (Any order) Step 1 Look for P and QRS sequence There should be a P before each QRS Are the P’s consistent? Should be a QRS after each P QRS should be followed by T’s Interpreting Rhythms Step 2 ♥ Check PR interval ♥ ♥ Should be 0.12 –0.20 Are PR intervals consistent Interpreting Rhythms Step 3 QRS duration and configuration Normal length of QRS is 0.04 – 0.12 seconds * (Sole 0.06 - 0.10) Q if present is the first negative deflection R is the first positive S is the negative deflection after the R Are the QRS complexes consistent? Interpreting Rhythms Step 4 What is the rate? The rate tells you how fast the heart is depolarizing HR = 300 / # of boxes between R to R interval HR = 1500 / # of small squares between an R to R interval. This only works on regular rhythms! HR = # of QRS complex in a 6 second strip x10 OR…find an R on a black line and count each black line 300, 150, 100, 75, 60, 50 to the next R. Interpreting Rhythms Step 5 Is the rhythm regular or irregular? If P waves are present, its an atrial rhythm Check regularity with calipers or paper and pen Measure P to P and R to R intervals If the marks are off by more than one small box it is irregular Interpreting Rhythms Step 6 Interpret the rhythm Use systematic analysis by applying the rules Each rhythm is a DEFINITION!!!! Let’s learn some rhythms so you can apply what you have learned! Each rhythm has unique characteristics Hence why they each have their own name! Dysrhythmia interpretation is developed through practice First you need to learn Normal, then you will recognize Abnormal! Normal Sinus Rhythm (Sinus Rhythm) The benchmark of all rhythms. Understanding this normal rhythm will help you see abnormal P before each QRS Upright small rounded P waves Atrial and ventricular rate are the same (60-100) Rhythm is essentially regular PR interval is 0.12 – 0.20 QRS is 0.04 to 0.12 seconds * (Sole 0.06 - 0.10) Normal Sinus Rhythm HR = 300 / # of boxes between R to R interval HR = 1500 / # of small squares between an R to R interval. This only works on regular rhythms! HR = # of QRS complex in a 6 second strip x10 OR…find an R on a black line and count each black line 300, 150, 100, 75, 60, 50 to the next R. Learning Dysrhythmias Dysrhythmia and Arrhythmia are sometimes used interchangeably. Dysrhymthia is a better term because it refers to irregularities in Rhythm where as arrhythmia literally means without a rhythm. You have learned the only normal rhythm, now let’s learn some Dysrhythmias!!!! Sinus Dysrhythmias Sinus dysrhythmias involve problems with the SA node or its conduction. They are usually caused by medications, vagal stimulation, ischemia, or hypoxia. Sinus Dysrhythmias include: Sinus Bradycardia Sinus Tachycardia Sinus Dysrhythmia Sinus Arrest/Sinus Exit Block Sinus Bradycardia It’s first name is Sinus so expect: Upright rounded P waves Regular rhythm PR interval 0.12 – 0.20 Normal QRS 0.04 – 0.12 (Sole 0.06 – 0.10) Its last name is Bradycardia so the key is that its rate is less than 60 bpm Sinus Bradycardia Causes and Treatment Causes Increased vagal stimulation Effects of medication SA node ischemia, hypoxia, IICP Normal in some athletes Treatment Pts usually asymptomatic (sleeping) need no Tx If symptomatic, Atropine, Epinephrine, Dopamine or temporary pacemaker Sinus Tachycardia First name is sinus so expect: Upright rounded P waves Regular rhythm PR interval 0.12 – 0.20 Normal QRS 0.04 – 0.12 (Sole 0.06 – 0.10) Its last name is Tachycardia so the key is that its rate is greater than 100 bpm (but less than 150) Sinus Tachycardia Causes and Treatments Causes: Exercise Stimulants Increased body temperature Hypo and Hypervolemia Treatments: Assess reason for tachycardia, if asymptomatic, no tx. If symptomatic, remove stimulus, and give Ca Channel blockers, Beta blockers, vagal stimulation Atrial Dysrhythmias Atrial Dysrhythmias are most often caused by increased automaticity in the R and L atria or both: PAC’s SVT/PAT Atrial Flutter Atrial Fibrillation Premature Atrial Contractions Its name defines it! ♥ Underlying rhythm is regular, usually NSR, PAC causes irregularity ♥ Rate variable, dependent on underlying rhythm and frequency of PACs. ♥ P wave ♥ ♥ ♥ ♥ premature different shape from beat generated from SA node, may be pointed, inverted, missing or a shortened PR interval May impose on the preceding T wave QRS normal PAC Cause and Treatment Cause: Impulses come from various foci in the atria Usually benign Can indicate atrial irritability Treatment PAC’s are usually benign – no treatment If patient is symptomatic withdraw stimuli and if necessary tx with Beta blockers Paroxysmal Atrial Tachycardia Supraventricular Tachycardia PAT and SVT are just that! Impulses originate above the ventricles (atria) Rate greater than 150 bpm P waves are present although can be difficult to detect because of rate. PR is not measurable QRS is usually normal, but fast Paroxysmal means starts and ends suddenly PAT and SVT Causes and Treatments Cause: Usually caused by emotional stress, overexertion, caffeine, tobacco, deep inspiration Also common in Rheumatic heart disease, CAD, or digitalis toxicity Treatment: Vagal Stimulation Medication: Adenosine, Cardizem, or Beta blockers Paroxysmal Atrial Tachycardia - Starts and stops suddenly - Rate greater than 150 Atrial Flutter First name is Atrial – focus is from the atria Last name is Flutter because of characteristic biphasic flutter waves (sawtooth) Irritable foci in the atria fire constantly Atrial rates are 250-350, usually regular Ventricular rate are slower, regular PR interval not measurable QRS is usually normal Qualified as 2:1, 3:1, 4:1 Atrial Flutter Cause and Treatment Cause: Rarely occurs in normal hearts Associated with CAD, HTN, MVP, CHF, PE Treatments: If rapid ventricular response (2:1) medication to control ventricular rate: diltiazem, digoxin, beta blockers Anti-arrhythmic drugs: Pronestyl, Cordarone, Corvert Patients are sometimes Heparinized to prevent stroke Cardioversion, Radiofrequency catheter ablation Atrial Fibrillation First name is Atrial – focus is from the atria Last name is Fibrillation so the atria are quivering not contracting purposefully. Wavy baseline with no discernable P wave Atrial rate is greater than 350, but not measurable Atrial and ventricular rhythms are irregular Ventricular response is usually less than 100 bpm No measurable PR interval QRS is normal Atrial Fibrillation Causes and Treatments Causes: Underlying heart disease, CAD, HTN, cardiomyopathy, ETOH, cardiac surgery Can be chronic or intermittent Most common arrhythmia in US and Canada Incidence increases with age Treatment: Beta blockers, Ca channel blockers and cardioversion Patients are sometimes Heparinized to prevent stroke First Degree AV Block This is a block caused by the AV Node Every SA impulse is conducted but the length of AV conduction is prolonged Conduction is normal through the ventricles What you will see is: Normal rate and rhythm P wave is normal Prolonged PR – greater than 0.20 QRS is normal First Degree AV Block Causes: MI, angina, hyperthyroidism, vagal stimulation Medication like Digitalis, Beta blockers, IV Verapamil Treatment: Usually none Patient is watched if it occurs after a cardiac event because it can be a precursor to more serious blocks Second Degree AV Block Second degree is not a prolonged atrial impulse, it is an interruption of conduction On EKG you will see impulses initiated but no conduction to the ventricles so you have some P waves without QRS following them There are 2 types: Mobitz Type I (Wenckebach) Mobitz Type II Second Degree AV Block Mobitz Type I Occurs within the AV node Less serious of the 2 types Each impulse produces a longer and longer delay until 3rd or 4th beat does not make it through to the ventricles and the beat is dropped P’s normal, PR’s gradually longer Atrial rate is normal (60-100) vent is slower QRS is normal but complex is dropped Second Degree AV Block Mobitz Type I Causes: Usually associated with ischemia in an Inferior wall MI, Digitalis toxicity, medications Usually temporary and tolerated well Treatment: If asymptomatic, observation If symptomatic, medication or temp pacer Second Degree AV Block Mobitz Type II More serious of the 2nd degree AV Blocks Block occurs at or below the AV Node, at Bundle of His, or the bundle branch area 2 or 3 P waves for each QRS P’s are normal, PR remains fixed on conducted beats QRS is widened Often leads to complete block Second Degree AV Block Mobitz Type II Causes: Acute anterior MI Rheumatic Heart Disease Digitalis toxicity CAD Treatment: Pacemaker Atropine, Epi, Isuprel, Dopamine until placement Third Degree Heart Block Called complete heart block No P waves are conducted to the ventricles Conduction is blocked through the AV Node to the Bundle of His, and bundle branches The atria and ventricles beat independently of each other (AV dissociation) Atrial rate is 60-100 Ventricular rate 20-60 Third Degree Heart Block Causes: Fibrosis or calcification of the conduction system, CAD, MI, Myocarditis, cardiomyopathy, open heart surgery Treatment: Pacemaker insertion Dysrhythmias of the Ventricles Ventricular Dysrhythmias occur when depolarization occurs incorrectly We will learn: PVC’s Ventricular Tachycardia Ventricular Fibrillation Idioventricular Rhythm Ventricular Standstill (Asystole) Premature Ventricular Contractions PVC’s Generated anywhere in the ventricles. Unifocal - they look the same Multifocal - they look different Patterns: Bigeminy Trigeminy Quadrigeminy Couplets More on PVC’s P waves usually absent before QRS No PR intervals associated with PVC’s QRS is > than 0.12 seconds and distorted with a pause ST segment is in the opposite direction of QRS Rhythm is made irregular by PVC’s Severity depends on frequency and underlying condition PVC’s Cause and Treatment Cause: Stimulants, stress, MI, MVP, CHF, CAD Treatment: Depends on frequency and symptoms Remove contributing factors Anti-arrhythmic drugs like Lidocaine, Pronestyl, or Amiodorone Ventricular Tachycardia 3 or more PVC’s Rate 100-250, no P, QRS wide and distorted Sustained = more than 30 sec Unsustained = less than 30 sec Can be monomorphic or polymorphic Life threatening dysrhythmia because it reduces Cardiac Output and often progresses to V fib V-Tach Causes: Acute MI, CAD, electrolyte imbalances, MVP, cardiomyopathy, reperfusion, Digitalis toxicity, CNS disorders, Swan insertions, Caths Treatment: Anti-arrhythmic drugs like Procanimide, Lidocaine, Amiodorone Ventricular Fibrillation Quivering of the ventricles caused by multiple foci in the ventricles Total loss of cardiac output – no heart rate Amplitude varies due to electrical activity Coarse vs. fine Course responds better No P,Q,R,S,or T are visible V-Fib Cause: Primary has no obvious cause or heart disease Most are secondary to another illness: MI, CAD cardiomyopathy, reperfusion, Swan insertions Cardiac Catheterization, pacemaker insertions, electrocution Treatment: Defibrillation and drug therapy Idioventricular Rhythm IVR is an escape rhythm generated from the Purkinje fibers when dominant pacers fail Rate is about 20 – 40 bpm usually regular No P or PR QRS is wide usually more than 0.12 Treated by cause Idioventricular Rhythm Cause and Treatment Cause: Escape rhythm, AV blocks, reperfusion, catheterizations, Acute MI, Digitalis toxicity Treatment: Specific to cause Ventricular Standstill (Asystole) Complete cessation of all heart electrical and mechanical activity (flat line) Multiple causes Lethal dysrhythmia that requires immediate medical intervention (ACLS, intubation, defibrillation, IV meds and possible pacing Pacemakers Electronic devices used in place of the SA or AV Nodes when they fail or are damaged Battery provides the electrical impulse that stimulates the myocardial conduction system Temporary or permanent Can be internal or external Permanent demand pacer is the most common kicks in when rate drops below a certain rate Pacing Rhythms Pacers are easily recognized on EKG strips. Atrial Ventricular Both The impulses cause a “spike” on the EKG Pacer malfunction includes: Failure to capture