* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 11 Heart - bloodhounds Incorporated
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
Artificial heart valve wikipedia , lookup
Electrocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
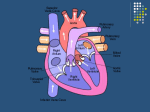
Physiology Cardiovascular System Cardiac Muscle and the Heart Myocardium Heart muscle Sits in the media stinum of the thoracic cavity Left Axis Deviation May have a right axis deviation with obesity and/or pregnancy May hang in the middle of the thoracic cavity if the individual is very tall The Heart The heart has four chambers Right and left atrium Atria is plural Right and left ventricle Blood Flow Through the Heart Deoxygenated blood enters the right atrium of the heart through the superior and inferior vena cava Deoxygenated blood Has less than 50% oxygen saturation on hemoglobin Hemoglobin Quaternary Structure Four Globin proteins Four Heme attach to each Globin Globin carries CO2, H+, PO4 Heme binds O2 and CO Heme contains an Iron ion About 1 million hemoglobin molecules per red blood cell Oxygen carrying capacity of approximately 5 minutes Heart Valves Ensure One-Way Flow of Blood in the Heart Atrioventricular Valves Located between the atria and the ventricle Labeled Right and Left Right Valve is also called Tricuspid Left Valve is also called Bicuspid or Mitral Heart Valves Papillary muscles are attached to the chordae tendinae Chordae tendinae are also connected to the AV valves Just prior to ventricular contraction the papillary muscles contract and pull downward on the chordae tendinae The chordae tendinae pull downward on the AV valves This prevents the valves from prolapsing and blood regurgitating back into the atria. Follow Path of Blood through Heart Blood Flow Due to gravity deoxygenated blood enters the right/left atrium (by way of the pulmonary veins) and flows through the open AV valve directly into the ventricles The filling of the ventricles with blood pushes the AV valve upward They are held in place by the chordae tendinae Right before the valves shuts completely the atria contract from the base towards the apex of the heart in order to squeeze more blood into the ventricle The AV valves snapping shut creates the “Lub” sound of the heart beat Blood Flow When the AV valves are shut the Pulmonary and Aortic semi-lunar valves are also shut Diastole Quiescence of the heart Myocardial Contraction (Systole) After Diastole occurs the ventricles begin to contract from the apex towards the base of the heart The deoxygenated blood on the right side of the heart is pushed through the pulmonary trunk after opening the semi-lunar valve to the pulmonary arteries into the lungs to become oxygenated. The oxygenated blood on the left side of the heart is pushed through the aorta after opening the semi-lunar valve into the systemic circulation Blood Flow The Ventricles do not have enough pressure to push all of the blood out of the pulmonary trunk and aorta The blood falls back down due to gravity The semi-lunar valves snap shut The “Dup” sound of the heart beat Blood Flow Blood is always flowing from a region of higher pressure to a region of lower pressure Atrial and Ventricular Diastole The heart at rest The atria are filling with blood from the veins The ventricles have just completed contraction AV valves are open Blood flow due to gravity Atrial Systole: Completion of Ventricular Filling The last 20% of the blood fills the ventricles due to atrial contraction Early Ventricular Contraction As the atria are contracting Depolarization wave moves through the conducting cells of the AV node down to the Purkinje fibers to the apex of the heart Ventricular systole begins AV Valves close due to Ventricular pressure First Heart Sound S1 = Lub of Lub-Dup Isovolumic Ventricular Contraction AV and Semilunar Valves closed Ventricles continue to contract Atrial muscles are repolarizing and relaxing Blood flows into the atria again Ventricular Ejection The pressure in the ventricles pushes the blood through the pulmonary trunk and aorta Semi-lunar valves open Blood is ejected from the heart Ventricular Relaxation and Second Heart Sound At the end of ventricular ejection Ventricles begin to repolarize and relax Ventricular pressure decreases Blood falls backward into the heart Blood is caught in cusps of the semi-lunar valve Valves snap shut S2 – Dup of lub-dup Isovolumetric Ventricular Relaxation Semilunar valves close AV valves closed The volume of blood in the ventricles is not changing When ventricular pressure is less than atrial pressure the AV valves open again The Cardiac Cycle begins again Cardiac Circulation Blood flowing through the heart has a high fat content Curvature as well as diameter of the arteries is important to blood flow through the heart Vasoconstriction due to sympathetic nervous system input Norepinephrine/Epinephrine Alpha Receptors not Beta Myocardial Infarction Heart Attack Due to plaque build up in the arteries Decrease in blood flow to myocardium Depolarization of muscle cannot occur due to myocardial death Myocardium doesn’t work as a syncytium any longer Destruction of gap junction or “connexons” Atherosclerosis Plaque in the arteries Elevated Cholesterol in the blood Cholesterol is cleared by the liver HDL – High Density Lipoprotein LDL – Low Density Lipoprotein H for healthy L for Lethal Omega 3 fatty acids “Rotorooter” for the arteries If a Patient Has a Left Atrial Infarction Then What happens to heart contraction and blood flow through the heart? What type of symptoms might your patient have? What recommendations might you give the patient to live a better life? There are some things they better not do or they will die. What are these things (in general)? Angioplasty/Open Heart Surgery Cardiac Muscle & Heart Heart muscle cells: 99% contractile 1% autorrhythmic Cardiac Muscle Cells Contract Without Nervous Stimulation Autorhythmic Cells Pacemaker Cells set the rate of the heartbeat Sinoatrial Node Atriventricular Node Distinct from contractile myocardial cells Smaller Contain few contractile proteins http://www.youtube.com/watch?v=7K2icszdxQc Excitation-Contraction (EC) Coupling in Cardiac Muscle Contraction occurs by same sliding filament activity as in skeletal muscle some differences: AP is from pacemaker (SA node) AP opens voltage-gated Ca2+ channels in cell membrane Ca2+ induces Ca2+ release from SR stores Relaxation similar to skeletal muscle Ca2+ removal requires Ca2 -ATPase (into SR) & Na+/Ca2+ antiport (into ECF) [Na+] restored via? http://www.youtube.com/watch?v=rIVCuC-Etc0 Cardiac Contraction Action Potentials originate in Autorhythmic Cells AP spreads through gap junction Protein tunnels that connect myocardial cells AP moves across the sarcolemma and into the t-tubules Voltage-gated Ca +2 channels in the cell membrane open Ca +2 enters the cell which then opens ryanodine receptor-channels Ryanodine receptor channels are located on the sarcoplasmic reticulum and Ca +2 diffuses into the cells to “spark” muscle contraction Cross bridge formation and contraction occurs Myocardial Contractile Cells In the myocardial cells there is a lengthening of the action potential due to Ca +2 entry http://www.youtube.com/watch?v=OQpFFiLdE0E AP’s in Contractile Myocardial Cells Phase 4: Resting Membrane Potential is -90mV Phase 0: Depolarization moves through gap junctions Membrane potential reaches +20mV Phase 1: Initial Repolarization Na+ channels close; K + channels open Phase 2: Plateau Repolarization flattens into a plateau due to A decrease in K + permeability and an increase in Ca +2 permeability Voltage regulated Ca +2 channels activated by depolarization have been slowly opening during phases 0 and 1 When they finally open, Ca +2 enter the cell At the same time K + channels close This lengthens contraction of the cells AP = 200mSec or more Phase 3: Rapid Repolarization Plateau ends when Ca +2 gates close and K + permeability increases again Myocardial Autorhythmic Cells Anatomically distinct from contractile cells – Also called pacemaker cells Membrane Potential = – 60 mV Spontaneous AP generation as gradual depolarization reaches threshold Unstable resting membrane potential (= pacemaker potential) The cell membranes are “leaky” Unique membrane channels that are permeable to both Na+ and K+ Myocardial Autorhythmic Cells, cont’d. If-channel Causes Mem. Pot. Instability Autorhythmic cells have different membrane channel: If - channel allow current (= I ) to flow f = “funny”: researchers didn’t understand initially If channels let K+ & Na+ through at -60mV Na+ influx > K+ efflux Slow depolarization to threshold Myocardial Autorhythmic Cells, cont’d. “Pacemaker potential” starts at ~ -60mV, slowly drifts to threshold AP Myocardial Autorhythmic Cells, cont’d. Channels involved in APs of Cardiac Autorhythmic Cells Slow depolarization due to If channels As cell slowly depolarizes: If -channels close & Ca2+ channels start opening At threshold: lots of Ca2+ channels open AP to + 20mV Repolarization due to efflux of K+ Autorhythmic Cells No nervous system input needed Unstable membrane potential -60mV Ca +2 channels open Calcium influx creates the steep depolarization phase of the action potential At the peak of the action potential Ca +2 channels close and slow K+ channels open Repolarization of the autorhythmic action potential is due to the efflux of K + Pacemaker potential not called resting membrane potential At -60mV If (funny) channels permeable to K + and Na + open Na + influx exceed K + efflux The net influx of positive charge slowly depolarizes the autorhythmic cells As the membrane becomes more positive the If channels gradually close and some Ca +2 channels open The influx of Ca +2 continues the depolarization until the membrane reaches threshold http://www.youtube.com/watch?v=3HvIKsQb6es Autonomic Neurotransmitters Modulate Heart Rate The speed at which pacemaker cells depolarize determines the rate at which the heart contracts The interval between action potentials can be altered by changing the permeability of the autorhythmic cells to different ions Increase Na + and Ca +2 permeability speeds up depolarization and heart rate Decrease Ca +2 permeability or increase K + permeability slow depolarization and slows heart rate http://www.youtube.com/watch?v=OQpFFiLdE0E http://www.youtube.com/watch?v=j2iY1cT2gEE Autonomic Neurotransmitters Modulate Heart Rate The Catecholamines: norepi and epi increases ion flow through If and Ca+2 channels More rapid cation entry speeds up the rate of the pacemaker depolarization Β1-adrenergic receptors are on autorhythmic cells cAMP second messenger system causes If channels to remain open longer http://www.youtube.com/watch?v=3HvIKsQb6es Autonomic Neurotransmitters Modulate Heart Rate Parasympathetic neurotransmitter (Acetylcholine) slows heart rate Ach activates muscarinic cholinergic receptors that Increase K+ permeability and Decrease Ca+2 permeability Electrical Conduction in the Heart Coordinates Contraction Action potential in an autorhythmic cell Depolarization spread rapidly to adjacent cells through gap junctions Depolarization wave is followed by a wave of contraction across the atria from the sinoatrial node on the right side of the heart across to the left side of the heart and then from the base to the apex From AV nodes to the atrioventricular bundle in the septum (Bundle of His) Left and right bundle branches to the apex Purkinje Fibers through the ventricles branches from apex to base and stopping at the atrioventricular septum Pacemakers Set the Heart Rate SA Node is the fastest pacemaker Approximately 72 bpm AV node approximately 50 bpm Bundle Branch Block Complete Heart Block Electrocardiogram Einthoven’s triangle Electrodes are attached to both arms and left leg to form a triangle Lead I- negative electrode attached to right arm Lead II – positive electrode attached to left arm Lead III – Ground attached to the left leg Electrocardiogram ECG (EKG) • Surface electrodes record electrical activity deep within body - How possible? • • Reflects electrical activity of whole heart not of single cell! EC fluid = “salt solution” (NaCl) good conductor of electricity to skin surface Signal very weak by time it gets to skin • ventricular AP = ? mV ECG signal amplitude = 1mV EKG tracing = of all electrical potentials generated by all cells of heart at any given moment ECG P wave Depolarization of the atria QRS complex Ventricular depolarization Atrial contraction begins almost at the end of the P wave Ventricular contraction begins just after the Q wave and continues through the T wave T wave Ventricular repolarization ECG PQ or PR segment Q wave Conduction through bundle branches R wave Conduction through AV node and AV bundle Conduction beginning up the Purkinje Fibers S wave Conduction continue up half way ST segment Conduction up the second half of Ventricles ECG When an electrical wave moving through the heart is directed toward the positive electrode, the ECG waves goes up from the baseline If net charge movement through the heart is toward the negative electrode, the wave points downward Einthoven’s Triangle and the 3 Limb Leads: + I RA – – II III + + LA – Why neg. tracing for depolarization ?? Net electrical current in heart moves towards + electrode Net electrical current in heart moves towards - electrode EKG tracing goes up from baseline EKG tracing goes Down from baseline Info provided by EKG: 1. 2. 3. HR Rhythm Relationships of EKG components each P wave followed by QRS complex? PR segment constant in length? etc. etc. For the Expert: Find subtle changes in shape or duration of various waves or segments. Indicates for example: Change in conduction velocity Enlargement of heart Tissue damage due to ischemia (infarct!) Prolonged QRS complex Injury to AV bundle can increase duration of QRS complex (takes longer for impulse to spread throughout ventricular walls). Heart Sounds (HS) 1st HS: during early ventricular contraction AV valves close 2nd HS: during early ventricular relaxation semilunar valves close Gallops, Clicks and Murmurs Turbulent blood flow produces heart murmurs upon auscultation Plumbing 101: Resistance Opposes Flow 3 parameters determine resistance (R): Tube length (L) 1. 1. Constant in body Tube radius (r) 2. 1. Can radius change? Poiseuille’s law 8L R= r4 Fluid viscosity ( (eta)) 3. 1. Can blood viscosity change?? Blood Flow Rate P/ R R 1 / r4 Velocity (v) of Flow Depends on Flow Rate and Cross-Sectional Area: Flow rate (Q) = volume of blood passing one point in the system per unit of time (e.g., ml/min) If flow rate velocity Cross-Sectional area (A) (or tube diameter) If cross sectional area velocity v = Q /A Blood Flow Mechanistic: Because the contractions of the heart produce a hydrostatic pressure gradient and the blood wants to flow to the region of lesser pressure. Therefore, the Pressure gradient (P) is main driving force for flow through the vessels Blood Flow Rate P/ R Pressure Hydrostatic pressure is in all directions Measured in mmHg: The pressure to raise a 1 cm column of Hg 1 mm Sphygmomanometer Flow is produce by Driving Pressure Pressure of fluid in motion decreases over distance because of energy loss due to friction Blood Flow Rate P/ R Unique Microanatomy of Cardiac Muscle Cells 1% of cardiac cells are autorhythmic Intercalated discs with gap junctions and desmosomes Electrical link and strength SR smaller than in skeletal muscle Signal to contract is myogenic Extracelllar Ca2+ initiates contraction (like smooth muscle) Abundant mitochondria extract about 80% of O2 Cardiac Muscle Cell Contraction is Graded Skeletal muscle cell: all-or-none contraction in any single fiber for a given fiber length. Graded contraction in skeletal muscle occurs through? Cardiac muscle: force to sarcomere length (up to a maximum) force to # of Ca2+ activated crossbridges (Function of intracellular Ca2+: if [Ca2+]in low not all crossbridges activated) http://www.youtube.com/watch?v=OQpFFiLdE0E http://www.youtube.com/watch?v=j2iY1cT2gEE http://www.youtube.com/watch?v=j2iY1cT2gEE Length Tension Relationship In order to increase heart rate at the SA node A. B. C. D. Potassium permeability across the membrane must increase Sodium permeability across the membrane must increase Potassium impermeability across the membrane must increase Sodium impermeability across the membrane must increase The neurotransmitter responsible for increasing potassium permeability at the SA node is A. B. C. D. Norepinephrine Epinephrine Acetylcholine Serotonin The initiation of the heartbeat normally originates from the A. B. C. D. Atrio-ventricular (A-V) node of the heart Sino-atrial (SA) node of the heart Central nervous system Thyroid The systemic circulation A. B. C. D. E. Receives more blood than the pulmonary circulation does Receives blood from the left ventricle Is a high pressure system compared to the pulmonary circulation Both (b) and (c) above are correct All of the above are correct The chordae tendinae A. B. C. D. E. Keep the AV valves from opening in the opposite direction during ventricular contraction Hold the AV valves during diastole Hold the right and left ventricles together Transmit the electrical impulse form the atria to the ventricles Contract when the ventricles contract The aortic valve prevents backflow of blood from the aorta into the left ventricle during ventricular diastole A. True B. False A mammalian heart has __________ chamber(s) A. B. C. D. One Two Three Four Ectopic focus is the place where A. B. C. D. E. An abnormally excitable area of the heart initiates a premature action potential All of the electrical impulses of the heart normally terminate An ECG lead is attached on the outside of the chest A heart valve is attached The chordae tendineae attach to a valve During isovolumetric ventricular contraction A. B. C. D. E. Rapid filling of the ventricles occurs No blood enters or leaves the ventricles The maximum volume of blood is ejected The maximum rate of ejection occurs None of the above is correct The type of intercellular junction that connects cardiac muscle fibers and allows for direct, electrical synapsing is known as a A. Tight junction B. Desmosome C. Plasmodesmata D. Gap junction Cardiac muscle A. B. C. D. E. Has a shortening velocity that is greater than that of glycolytic (white) skeletal muscle fibers Has a more extensive sarcoplasmic reticulum than skeletal muscle Is an electrical syncytium Has a resting potential that depends mainly on sodium distribution All of the above are correct Spontaneous depolarization of the sinoatrial node is produced by A. B. C. D. E. An inward leak of sodium and an increase in the outward leak of potassium An inward leak of sodium and a decrease in the outward leak of potassium Opening of fast sodium channels and a decrease in the outward leak of potassium Opening of fast sodium channels and an increase in the outward leak of potassium Neural impulses from the sympathetic nerves A heart murmur is characterized by A. B. C. D. Rapid heart contraction Irregular heart contraction Mitral valve prolapse Semilunar valve dysfunction The P wave of a normal electrocardiogram indicates A. B. C. D. Atrial depolarization Ventricular depolarization Atrial repolarization Ventricular repolarization Damage to the _______ is referred to as heart block A. B. C. D. SA node AV node AV bundle AV valve Stenosis of the mitral valve may initially cause a pressure increase in the A. B. C. D. Vena cava Pulmonary circulation Left ventricle Coronary circulation The tricuspid valve is closed A. B. C. D. E. While the ventricle is in diastole By the movement of blood from the atrium to ventricle By the movement of blood from atrium to ventricle While the atrium is contracting When the ventricle is in systole