* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiomyopathy - Lock Haven University
Management of acute coronary syndrome wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Echocardiography wikipedia , lookup
Aortic stenosis wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
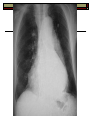
Cardiomyopathy Craig Ernst MHS, PA-C Lock Haven University Cardiomyopathy General term indicating disease of cardiac muscle resulting in abnormal function Divided into three types: Dilated cardiomyopathy-ventricular dilation Hypertrophic cardiomyopathy-myocardial hypertrophy Restrictive cardiomyopathy-impaired ventricular filling Can have characteristics of more than one Dilated Cardiomyopathy (DCM) Characterized by dilation and impaired systolic function of left &/or right ventricle Most common DCM is ischemic cardiomyopathy Idiopathic (ICM) next most common Familial autosomal dominant in 20% of cases. Role of coxsackie/adenovirus and immune mediated etiology unknown. DCM Many cases of systemic heart muscle disease present with features of DCM including: Ischemic/rheumatic CVD Generalized disease- hemochromatosis, sarcoid Connective tissue disease-SLE, systemic sclerosis Neuromuscular disease-Friederich’s ataxia etc Glycogen storage disease Primary heart muscle disease- amyloidosis Alcohol excess Cytotoxic drugs-doxorubicin, cyclophosphamide Pregnancy Starling Curve Contractility Starling Curve Volume DCM Clinical features: R/L heart failure Arrhythmia Emboli Cardiomegaly Tachycardia JVD 3rd/4th heart sounds basiler crackles displaced PMI DCM Evaluation CXR: cardiomegaly EKG: diffuse non specific ST-T wave changes, LBBB common, tachycardia, conduction abnormalities, arrhythmias Echo: poor chamber contraction and dilated chambers If CAD suspected, cardiac catheterization Endomyocardial biopsy for research only. DCM Treatment Rx failure & arrhythmias Ace Inhibitors a must in failure management Non-specific Beta blockade: Carvedilol, ??, ?? Anticoagulation for A.fib/mural thrombus. CRT-D (Bi-V AICD) Transplant Sudden death – Due to V. Tach. or V. Fib Hypertrophic Cardiomyopathy (HCM) Complex heart disease due to the asymmetric left ventricular hypertrophy, left ventricular stiffness, mitral valve changes and cellular changes (myocardial disarray) 60 % inherited 40 % sporadic HTN, Aging, Unknown Most autosomal dominant w/ variable penetrance Other Terms Hypertrophic Obstructive Cardiomyopathy (HOCM) Idiopathic hypertrophic subaortic stenosis (IHSS) Asymmetrical septal hypertrophy (ASH) Systolic anterior motion (SAM) of mitral apparatus Pathophysiology HOCM is a subvalvular obstruction! Distinct from valvular Aortic Stenosis (pressure gradient across valve) Gradient/obstruction increases with lower LV volume HOCM pts here do better when full and slow Standing after squatting/Valvsalva lower venous return & increase outflow obstruction and intensity of murmur MV leaflet HCM without obstruction HCM with obstruction HOCM) HOCM: Clinical Features: Chest pain Dyspnea Syncope/Pre-syncope (typically with exertion) Palpitations Sudden Death (arrhythmia) Typically occurs in asymptomatic young adults or adolescents (10-35 y/o) Family history of sudden death, sustained ventricular tachycardia, & B/P response to exercise are recognized risk factors Diastolic dysfunction with impaired filling Outflow tract obstruction occurs in 1/3 of cases Physical Exam Systolic murmur; with little to no radiation to neck vessels (increased by maneuvers that decrease preload such as Valvsalva or squatting) Decreases ventricular filling May hear systolic murmur of MR Weak late carotid pulse (late obstruction) Diagnosed by echocardiogram. Evaluation EKG-LVH with ST-T wave changes CXR-normal ECHO indicated if PE suggests IHSS Pedigree analysis (ECHO to screen 1st relatives) Genetic analysis XST/Holter Treatment of HOCM Relief of symptoms, prevention of endocarditis, arrhythmias and sudden death B-Blockers or verapamil Amiodarone or procainamide for A Fib need atrial kick to adequately fill LV Avoid afterload reducing agents and vasodilators (no ACEI/A2RB, NITRO)-refractory hypotension better filling, slow, bigger heart-less obstruction These agents increase outflow obstruction actually do better with increased SVR Slow controlled emptying from increased SVR SBE prophylaxis Treatment of HOCM Implantable defibrillators may be indicated if at risk for SCD Dual-chamber pacemakers: reverse of resynchronization therapy for LVEF Surgical: myotomy & myomectomy Non surgical ablation of the septum (alcohol ablation through cath) Sudden Cardiac Deaths 2-3 % per year Sudden & unexpected Sudden death may be the initial (only) presentation Risk for SCD: NPR link Extreme LVH Family history of SCD History of Vtach or syncope Failure of BP to rise with exercise Treatments that lower gradient do not prevent SCD Restrictive Cardiomyopathy (RCM) May cause systolic & diastolic dysfunction All increase LV stiffness Characteristic ventricle filling pressures Over time filling dramatically ceases Restrictive Cardiomyopathy Some cardiomyopathies do not present with dilation or hypertrophy but rather restricted ventricular filling (as with pericarditis) Amyloidosis Sarcoidosis Hemochromoatosis Endomyocardial fibrosis Atrial dilation, atrial fibrillation and clot formation common in restrictive Restrictive Cardiomyopathy Clinical Features Dyspnea Fatigue Embolic phenomena Elevated venous pressures JVD Hepatomegaly Edema Ascites Restrictive Cardiomyopathy CXR=cardiac enlargement EKG-low voltage and ST-T wave abnormalities (Exaggerated Septal Q’s – Think MI) Echo-symmetrical myocardial thickening Endomyocardial biopsy may be useful. Is it restrictive pericarditis? Pre-op effusion Post op effusion Restrictive Cardiomyopathy Treatment No specific treatment Treat underlying cause… results? Those with amyloidosis may recur after transplant Amyloidosis Systemic disorder, but if DHF occurs usually from multiple myeloma Fibrillar protein deposited throughout the myocardium leading to rubbery consistency and concentric hypertrophy RV & LV hypertrophy Absence of high voltage QRS on EKG despite LVH on ECHO Appearance on Echo Amyloidosis Fat pad aspirate or tissue biopsies for systemic amyloidosis Endomyocardial biopsy if questionable etiology Poor prognosis Hemochromatosis Hereditary disorder characterized by excess dietary iron absorption and deposition in tissues with resulting endorgan damage. Affects liver first and most frequently Pancreatic involvement results in DM Cardiac deposits leads to dilated cardiomyopathy Skin deposits leads to bronze discoloration that results from increased melanin production. Hyperpigmentation Remember: liver, pancreas, heart Dx: AST, ALT, serum iron, TIBC, ferritin