* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Auscultation of the heart Stethoscope • It should combine a bell
Survey
Document related concepts
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Heart failure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Aortic stenosis wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
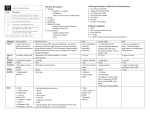
Stethoscope Auscultatory area Locations of auscultatory sites Technique Auscultatoy aids Auscultation of the heart It should combine a bell-‐type chest piece and a diaphragm. High-‐pitched sounds such as aortic diastolic murmurs, systolic murmurs, the 1st and 2nd heart sounds and opening snap are heard better with the diaphragm, and low-‐pitched sounds e.g 3rd and 4th heart sound or mitral diastolic murmurs with the bell Mitral area: corresponds to the apex beat and then outward to the left anterior axillary line. Tricuspid area: just to the left of the lower sternum Aortic area: o 1st aortic area: to the right of the sternum in 2nd ICS. o 2nd aortic area: to the left of the sternum in 3rd ICS Pulmonary area: to the left of the sternum in 2nd ICS. Downward, along the left sternal border (left 3rd and 4th space) and toward the apex (in congenital heart disease e.g VSD) • • • • • • • Additional auscultatory area • Right supraclavicular fossa: venous & arterial sounds and murmurs transmitted from the base of the heart are heard well (e.g A.S & P.S). • A continuous murmur of a PDA: best heard in 1st & 2nd ICS at the left midclavicular line • Rumbling mid-‐diastolic murmur of mitral stenosis: best heard medial to the apex of the heart • The pan systolic murmur of M.R : arise in the mitral area at the apex and propagated toward the left axilla • Systolic murmur of the coarctation of the aorta : in the interscapular area of the back. • Systolic murmur of a ruptured chorda tendinae: over cervical spine and in interscapular area • Murmurs may be heard over the lung fields because of pulmonary arterio-‐venous fistula. • Lung bases: for bilateral fine basal crepitations secondary to left ventricular failure. Area Location Murmur best heard Sounds heard MS LV S3 MR LV S4 Left ventricle Mitral area At apex impulse AS A2 AR MV opening snap IHSS FXnal mid diastolic rumble Tricuspid Lower sternum 2cm to left and TS RV S3 & S4 Right ventricle area right TR TV opening snap VSD Left posterior thorax between Left atrium axillary line and spine at level of scapular tip Right atrium Lower sternum & 2cm to right of TR sternum 1st 2nd 2nd right , 3rd left interspace at AR A2 Aorta aortic area sternal edge AS Aortic ejection click Aortic flow murmur Pulmonary 2nd left interspace at sternal edge PS P2 Pulmonary area PR Pulmonary ejection artery Pulmonary flow murmur click PDA murmur Descending Posterior thorax 2 – 3 cm to Coarctation of the aorta thoracic artery either side of the spine Aortic aneurysm Aortic stenosis • Patient should be examined in a quiet, warm, comfortable room. • You should examine the heart systematically, using both diaphragm and the bell. • Starting listening at the apex à to lower left sternal border (Tricuspid area) à along sternal border à to base of the heart (pulmonary & aortic areas) • In addition to auscultating the patient while lying position, also examined in left lateral position, while standing, squatting, sitting position with the patient slightly leans forward, and during valsalva maneuver and following its release. Auscultatory aids Physiological effects Effect on murmurs Venous return↓ Most murmurs decrease in intensity except: a) Hypertrophic obstructive cardiomyopathy Valsalva maneuver b) MV prolapse (Which increase) Venous return↓ Most murmurs decrease in intensity except: a. Hypertrophic obstructive cardiomyopathy Standing b. MV prolapse (Which increase) Increases venous return, stroke Most murmurs increase in intensity except: Squatting volume & systemic resistance a. Hypertrophic obstructive cardiomyopathy b. MV prolapse (Which decrease) Handgrip Increases systemic resistance & C.O.P Most murmurs across obstructed valves; MR, VSD & aortic regurge increase whereas murmurs of Hypertrophic obstructive cardiomyopathy decrease Potent vasodilators Murmurs of AS & Hypertrophic obstructive Amylnitrate cardiomyopathy increase, whereas murmur of MR, VSD & AR decrease Inspiration Diminishes blood flow through left-‐ LT-‐sided murmur (M & A) decrease sided valves & augments blood flow RT-‐sided murmurs (T &P) increase through RT sided valves Expiration reverse reverse How to listen? • • • Timing Cardiac auscultation aims at listening to Response to amylnitrate is useful in distinguishing: 1. systolic murmur of AS (augmented) from that of MR (diminished) 2. systolic murmur of TR (augmented) from that of MR (diminished) 3. systolic murmur of isolated pulmonary stenosis (augmented) from that of tetralogy of fallot (diminished) 4. systolic murmur of isolated pulmonary stenosis (increased) from that of ventricular septal defect (diminished) 5. Diastolic rumbling murmur of MS (augmented) from the Austin-‐flint-‐murmur of AR (diminished) 6. Early Diastolic murmur of pulmonary Regurge (augmented) from that of aortic regurge (diminished) • Listen to one thing at a time, while focusing all attention on it, and comparing it in various valve areas. • 1st listen to the sounds then between the sounds. • Identify the 1st & 2nd sounds, and listen to them separately: o 1st best heard at mitral and tricuspid areas o 2nd best heard at pulmonary & aortic areas Next, focus on systole then diastole. Listen specifically for extra-‐sounds only (not murmur). Finally, listen for the presence of murmurs first in systole then in diastole, scanning all the precordium. Note the point of maximum intensity and the transmission of any murmur heard. • Easy once the 1st & 2nd heart sounds are identified and the H.R is not rapid. • Systole corresponds to the interval between 1st & 2nd sounds which is shorter in duration than diastole • Systole begins with the beginning of 1st sound and ends at the beginning of 2nd sound. • Diastole begins with the beginning of 2nd sound and extends to the beginning of 1st sound • It is difficult to identify systole and diastole when they become equal in duration with rapid heart rates. Two methods may be of value: o To time the heart sounds either in relation to the apical impulse or carotid artery pulsations (mark systole). o To identify the 2nd sound at the base (loudest) and to “inch” the stethoscope downwards toward the cardiac apex. 1. Heart sounds 2. 2-‐ Additional sounds (click, gallop, opening snaps and pericardial knock). 3. 3-‐ Murmurs Heart sounds First heart sounds Character Site Component Intensity depends on Abnormalities The beginning of systole. Low pitched dull sound and longer (Lubb) than 2nd sound (S2) (dup) which is shorter and sharper Best heard at the apex and at the left lower sternal border 1. Small low-‐frequency vibrations (not audible) which are coincident with the beginning of left ventricular contraction (i.e muscular in origin) 2. large high-‐frequency vibrations (mitral component) related to mitral valve closure (M1). 3. Followed closely by a second high-‐frequency vibrations (tricuspid component) related to tricuspid valve closure (T1). 4. Small low-‐frequency vibrations which coincide with acceleration of blood flow into great vessels (aortic component) and normally is not audible. a) Rate of rise of left ventricular pressure. The faster the rise (hyperdynamic circulation), the louder the first heart sound. b) Position & mobility of the mitral and tricuspid valves at the start of ventricular systole c) Structure & mobility of the mitral and tricuspid valve leaflets. Causes Accentuated 1. M & T stenosis with mobile cusps 5. Sinus tachycardia 1st sound 2. Left atrial myxoma 6. Subjects with thin chest wall 3. MV prolapse 7. Hyperkinetic states 4. Exercise 8. In children Weak 1. Mitral insufficiency (not d.t prolapse) 5. Severe hypotension and shock (Muffled) 2. Bradycardia & hypodynamic circulatory states as states 1st sound 3. myxoedema 6. Condition caused absent apex (e.g 4. Calcification or fibrosis of A-‐V valves pericardial effusion) 7. Impaired myocardial contractility (e.g myocarditis, sever HF) Variable 1. Atrial fibrillation 3. Ventricular tachycardia (d.t A-‐V intensity of 2. A-‐v block (Wenckebach and third-‐degree block) dissociation) 1st sound 4. Pulsus alternans 1. Narrow splitting: normal in which the two major components i.e MI & TI are separated by only 20-‐3-‐ ms and appreciated only a single sound at the bedside 2. Wide splitting: occurs in à o Ebstein’s anomaly of tricuspid valve True o TS splitting 1st o RBBB of proximal type sound o Left ventricular pacing o Ectopic beats and idioventricular rhythms o originating from the left ventricle. 3. Reversed splitting: occurs in à o RT ventricular pacing o Hemodynamically significant obstruction of o mitral valve (e.g MS & left atrial myxoma) o Ectopic beats and idioventricular rhythms o originating from the RT ventricle. Pseudo split 1. Combination of S4 & S1 1st sound 2. Combination of S1 and an ejection click Character Site Component Timing Intensity Abnormalit ies Second heart sounds 1. Sharper in quality and higher-‐pitched than S1 and is recognized as: 2. the “dup” in “Lubb-‐dup” 3. the sound which follows the apical impulse 4. the sound which immediately follows the carotid pulse wave best heard in 2nd RT and LT ICS along the sternal border using the diaphragm. Aortic component (A2) Pulmonary component (P2) • d.t closure of aortic valve, which sets up transient • d.t closure of pulmonary valve, which sets up transient vibrations vibrations in valve leaflets, blood and aortic walls. in valve leaflets, blood and pulmonary walls. • Responsible for 2nd sound at the apex and louder • It is shorter and normally heard only at and around the through the pericordium pulmonary area • Because the left ventricular ejection period is shorter than the RV ejection period, A2 precedes P2. • During inspiration, the eplitting of the 2nd sound widens mainly d.t delaying in pulmonary component, result in increase in VR Depends mainly on closing pressure in the corresponding vessel, so A2 is louder than P2 Loud Loud A2 Loud P2 second 1. Systemic HTN 1. Pulmonary HTN sound 2. Aortic root dilatation (Tmbour S2) 2. Dilatation of pulmonary trunk e.g: 3. Transposition of the great arteries (the aorta is a. Idiopathic pulmonary artery dilatation closer to anterior chest wall) b. Osteum secundum atrial septal defect 4. Pulmonary atresia 3. Decrease antro-‐posterior diameter of the chest w 5. Coarcatation of the aorta place the pulmonary trunk close to chest wall 6. Hyperkinetic circulation 7. in children 8. Tachycardia 1. Reduced mobility of the smilunar valves d.t either calcification, fibrosis or stenosis e.g AS & PS Weak (soft) 2. Low C.O.P or lower systolic pressure in pulmonary or systemic circulation S2 3. Emhysema 1. Tetralogy of fallot 5. Very large VSD (pulmonary pressure equal to 2. Pulmonary atresia (no pulmonary component) systemic pressure) Single S2 3. Truncus arteriosus (no pulmonary component) 6. Severe AS (absent A2) 4. Severe PS (no pulmonary component) 7. Eisenmenger’s complex & aging Delayed pulmonary closure: Early aortic closure: • Normal: especially in children. The splitting • Short left ventricular ejection time. increases by inspiration d.t increase of the • Mitral regurgitation venous return to RT side of the heart. • VSD • Delayed electrical activation of the Rt ventricle: a) Complete RBBB (proximal type) b) Left ventricular spacing Splitting 2nd c) Left ventricular ectopic beats HS (normal or • Prolonged Rt ventricular mechanical systole: exaggerated a) Acute massive pulmonary embolism physiologic b) Pulmonary hypertension with Rt al splitting – ventricular failure wide) c) Pulmonary stenosis (moderate to severe). • Decreased impedance of the pulmonary vascular bed: a) Normotensive atrial septal defect. b) Idiopathic dilatation of the pulmonary artery S2 becomes single during inspiration and split during • Prolonged Lt ventricular mechanical systole: expiration a) LBBB (peripheral type) b) Left ventricular out flow tract obstruction 1. Delayed aortic closure: c) Hypertensive CVD Splitting 2nd • Delayed electrical activation of the left ventricle: d) coronary Ht disease HS a) Complete RBBB (proximal type) (reversed b) Left ventricular spacing • Decreased impedence of the Sustemic vascular bed: splitting ; c) Left ventricular ectopic beats a) Post stenotic dilatation of the aorta Paradoxical secondary to aortic stenosis ) • Delayed electrical activation of the left ventricle: b) PDA a) Complete RBBB (proximal type) 2. Early pulmonary closure: b) Left ventricular spacing Early electrical activation of the right ventricle as in c) Left ventricular ectopic beats WPW (type B). Fixed Wide fixed splitting of S2 in pulmonary area which is not affected by inspiration is pathognomonic of ASD, this splitting of because the Rt & LT ventricular stroke volumes vary in the same way during the respiratory cycles as a result of 2nd HS free communication between Rt & Lt atria. Accentuated 1. Children 4. Tachycardia both heart 2. Thin chest wall 5. Hyperkinetic states sounds 3. Exercise Weak both 1. Apex behind rib 5. Emphysema heart 2. Obesity 6. Pleural effusion sounds 3. Myxoedema 7. Pericardial effusion 4. Scleroderma 8. Impaired myocardial contractility Character Site Character Site Causes Systolic sounds Diastolic sound Third Heart sounds D.t sudden halting of the rapidly expanding ventricles at the end of the rapid filling phase, producing transient vibrations of the mitral cusps and the papillary muscles and the chordae tendinae • low-‐pitched, low frequency sound. • intense than 1st &2nd sound • Short in duration & follows A2 by 120-‐200 ms • Sometimes it is palpable • Best heard with bell pressed lightly against the skin at or near the apex with the patient in left lateral position. • Common in children, adolescents, and young adults Physiologic • Rare above the age of 40 S3 • It increases by inspiration and disappears on sitting or standing Character Is quiet faint & easily overlooked Maneuvers w increase VR (e,g passive leg raising) are helpful in increasing the intensity It persists in sitting position and this differentiate it from physiologic S3. 1. Volume overload e.g Anaemia, thyrotoxicosis, arterio-‐venous fistula, Lt-‐to-‐Rt shunt (e.g VSD, PDA) Pathologic S3 2. Ventricular failure (ventricular diastolic gallop): it can be heard after the S2 in patient with Causes heart failure d.t: a) Idiopathic dilated cardiomyopathy b) Ischemic heart disease c) Congenital heart disease 3. Restrictive myocardial or pericardial disease e.g Constrictive pericarditis (pericardial knock), restrictive & hypertrophic cardiomyopathy nb N.B: ventricular diastolic gallop may be: a. Left ventricular S3 which is heard best at the apex b. Right ventricular S3 which is heard best at the lower left sternal edge and increase in intensity on inspiration Fourth heart sounds • Low frequency, low-‐pitched, dull sound, audible under pathologic conditions just prior to S1 • Audible S4 usually accompanied by palpable pre-‐systolic apical impulse Best heard with bell at the point of maximal impulse with the patient turned in left lateral position (Left atrial sound) and being heard best during expiration while, Rt atrial sound best heard at the lower left sternal edge or in xiphoid area and is usually heard loud on inspiration Physiologic recordable but rarely audible 1. Decreased ventricular compliance: a) Ventricular Hypertrophy i.e systemic or pulmonary HTN , hypertrophic cardiomyopathy b) Ischemic heart disease i.e Angina pectoris, acute MI Pathologic c) Idiopathic dilated cardiomyopathy 2. Excessively rapid late diastolic filling secondary to Vigorous atrial systole: a) Hyperkinetic state e.g anaemia, thyrotoxicosis b) Acute atrio-‐ventricular valve incompetence 3. Arrhythmias e.g heart block Additional sounds or triple rhythm Timing Occur early in systole shortly after S1 d.t sudden tensing of opening of semilunar valve and root of big arteries. Site at the lower left sternal edge and apex • Bicuspid aortic valve Causes • Valvular aortic stenosis Aortic Ejection • Aortic root dilatation Early ejection sounds • Important in diagnosis because it indicates an sounds Clinical valvular aortic stenosis rather than a Includes significance supravalvular or sub-‐valvular stenosis or IHSS is present. • Also suggests that the aortic valve is not severely calcified Site Over 2nd left ICS at the sternal edge Decreases with inspiration (if pulmonary HTN is not Pulmonary Intensity present) and loud with expiration Ejection sounds • Valvular pulmonary stenosis Causes • Pulmonary artery dilatation • Hyperdynamic states Non ejection Timing heard in the middle or late part of systole systolic click Character sharp, high-‐pitched clicky sound Site best heard at the apex, and becomes louder when the patient lies on left side or sits Cause • MV prolapse • Rarely, extra cardiac in origin possibly related to previous pericarditis (remnants of pericardial rub) Opening Site best heard along the lower left sternal border or between this point and the apex snap of Character Short, sharp sound, sometimes confused with S3 (or ventricular diastolic filling mitral valve gallop) but it is earlier and sharper and high-‐pitched than it Cause denotes presence of Mitral Stenosis with mobile cusps, and when it is not heard in patient with mitral stenosis this mean that the mitral valve is calcified and immobile Opening snap Opening Site best heard nearer the midline than mitral opening snap and occasionally along the snap of lower right sternal border tricuspid Cause denotes presence of tricuspid Stenosis valve Gallop sound Pericardial knock Tumour plop nb Ventricular (S3 or protodiastoli c) gallop Atrial (S4 or presystolic) gallop Clinical • The earlier the OS the more severe the valvular stenosis (MS & TS) significance • It denotes (pliable) cusps of opening • Soft or absent OS in the presence of valvular stenosis indicates calcified or poorly snap mobile valve • Appears in early diastole & corresponds to normal S3 • Indicates heart failure or volume overload d.t mitral regurge • Normal in children and young adult but abnormal above age of 40. Appears in late diastole (presystole) & corresponds to normal S4 Normal in elderly In younger patients it indicates: b) Forceful atrial ontraction o Pulmonary or aortic stenosis o Pulmonary or systemic HTN o Coronary heart disease o Cardiomyopathy b) Easily heard atrial ontraction 1st, 2nd, 3rd degree heart block • Occur in conditions of tachycardia where diastole is shortened & both ventricular and atrial gallops are heard superimposed on each other and may be louder than either of two regular heart sounds Summation • May be heard in normal hearts and in patients with both ventricular & atrial gallops gallop • Sometimes called S7 from the sum of S3 & S4 and it can be easily palpated • Location is in early-‐to-‐mid diastole Character • Sharp, snapping, high-‐pitched sound • May be very loud and even louder than the heart sounds • Increase on inspiration Timing Occur early in diastole (from 0.08-‐0.13 second after S2) but later than timing of opening snap and earlier than that of S3 Site Heard best in center of the pericordium Cause In case of constrictive pericarditis Timing Early diastolic sound produced when a left (or Rt) atrial myxoma attached to a stalk prolapse through the mitral (or tricuspid) valve in diastole Character Intermittent sounds varying in intensity and quality from cycle to cycle Site At left lower sternal border Sounds produced by prosthetic heart valve • Early diastolic sound is generated by the opening movement of a mechanical prosthesis in mitral location. • The opening sound is especially prominent with a ball-‐in-‐cage prostehsis (Starr-‐Edwards) and less prominent with a tilting disc prosthesis (Bjork -‐Shiely) • • •