* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Advance physiology Cardiovascular system
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
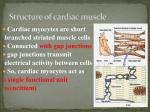
Advance physiology Cardiovascular system ASSIST. PROF. DR. MAJIDA A. J. AL-QAYIM Cardiovascular system The cardiovascular system consists of the heart and two vascular systems. The heart consists of two pumps, pumps blood through two vascular systems: the low pressure pulmonary circulation in which gas exchange occurs the systemic circulation, which delivers blood to organs,. The heart as a pump The heart is a cone shape muscular organ located in the thoracic cavity. The heart wall consist of three distinct layers ; Endocardium Myocardium Pricardium The myocardium, or heart muscle, receives nutrients via the coronary circulatation. Heart valves Special structures of the heart 1-Valves are outgrowths from the endocardium which prevent backflow of blood. Heart valves ensure unidirectional blood flow through the heart Atrioventricular (AV) valves lie between the atria and the ventricles AV valves prevent backflow into the atria when ventricles contractSemilunar Aortic semilunar valve lies between the left ventricle and the aorta Pulmonary semilunar valve lies between the right ventricle and pulmonary trunk Valves contain three components. a. Endothelium covers the valve. b. chordae tendineae attach the flaps of the AV valves to the heart wall at the apex of the heart.. C. papillary muscles Heart Valves 5 Chapter 18, Cardiovascular System Figure 18.8a, b 2- The conducting system The heart contains specialized cardiac musclefibers that can self-generate an action potential, and are therefore called autorhythmic fibers. These cells do not require extrinsic neural input, and they can continue to generate an action potential even when the heart is removed from the body 1- SA nodeThe heart normally has a selffiring unit, located in the right atrium, called the sinoatrial node or sinus node (pacemaker cells), 2-The electric signal from the sinus node activates the atrial walls to contraction, and then reaches the main conduction system at the level of the atrioventricular node (AV node). 3-From the bundle of His, the signal is transmitted down a rapid conduction pathway 4- These bundle branches divide into a network of conducting Purkinje fibres just below the endocardial surface. Purkinje fibres are large diameter cells without Ttubulesbundle of his Molecular structure of the cardiac muscle Cardiac muscle cells orcardiomyocytes(also known asmyocardiocytes[1]or cardiac myocytes[2]) are the muscle cells (myocytes) that make up thecardiac muscle • cardiac muscle has myofibrils that contain actin & myosin filaments almost identical to those found in skeletal muscle these filaments lie side by side & slide along one another during contraction in the same manner a occurs in skeletal muscle The cells are Y shaped and are shorter and wider than skeletal muscle cel They are predominatly mononucleated. The cardiac muscles, unlike skeletal ones, cannot rest, even for a moment. They must work continuously. cardiac muscle fibers arranged in a latticework, with the fibers dividing, recombining, & then spreading again • cardiac muscle is striated in same manner as in skeletal muscle Each myocardiocyte contains one nucleus. The density of mitochondria (the energy generators of the body) in these cells is high, which lets th produce an abundance of ATP molecules through aerobic respiration, to drive the muscle's functioning. This is the reason why a heart's muscle tissue can work without fatigue and ensures a lifetime of service. The flexibility of the cell, along with the integrity of the cytosol is maintained by two proteins, calle vimentin and desmin These muscles have a very marginal store of glycogen, which is the raw material for energy production in anaerobic conditions. So, in case of a heart attack, when the heart muscles fall short oxygen, they simply die. Recent studies have shown that regeneration in heart cells is possible The coronary arteries useful for the heart to be , rely on an available blood and electrical supply to deliver oxygen and nutrients and remove waste products such as carbon dioxide The myocardium work as a Syncytium The syncytium of cardiac muscle is important because it allows rapid coordinated contraction of muscles along their entire length. Action potentials propagate along the surface of the muscle fiber from the point of synaptic contact, through intercalated discs. Although a syncytium, cardiac muscle differs because the cells are not long and multinucleated. Cardiac tissue is therefore described as a functional syncytium, as opposed to the true syncytium of skeletal muscle. There is an atrial syncytium and a ventricular syncytium that are connected by cardiac connection fibres.[4]Electrical resistance through intercalated discs is very low, thus allowing free diffusion of ions. The ease of ion movement along cardiac muscle fibers axes is such that action potentials are able to travel from one cardiac muscle cell to the next, facing only slight resistance. Each syncyntium obeys the all or none law.[5] Intercalated discs are complex adhering structures that connect the single cardiomyocytes to an electrochemical syncytium Under light microscopy, intercalated discs appear as thin, typically dark-staining lines dividing adjacent cardiac muscle cells. The intercalated discs run perpendicular to the direction of muscle fibers Intercalated discs are described to consist of three different types of cell-cell junctions: the actin filament anchoring adherens junctions, the intermediate filament anchoring desmosomes , and gap junctions. They allow action potentials to spread between cardiac cells by permitting the passage of ions between cells, producing depolarization of the heart muscle intercalated discs consist for the most part of mixed-type adhering junctions named area composita (pl. areae compositae) representing an amalgamation of typical desmosomal and fascia adhaerensproteins Cardiac muscle cells orcardiomyocytes are the muscle cells that make up thecardiac muscle • cardiac muscle has myofibrils that contain actin & myosin filaments almost identical to those found in skeletal muscle – these filaments lie side by side & slide along one another during contraction in the same manner as occurs in skeletal muscle The cells are Y shaped and are shorter and wider than skeletal muscle cells. They are predominatly mononucleated. The cardiac muscles, unlike skeletal ones, cannot rest, even for a moment. The density of mitochondria (the energy generators of the body) in these cells is high, which lets them produce an abundance of ATP molecules through aerobic respiration, to drive the muscle's functioning. This is the reason why a heart's muscle tissue can work without fatigue and ensures a lifetime of service. These muscles have a very marginal store of glycogen, which is the raw material for energy production in anaerobic conditions. So, in case of a heart attack, when the heart muscles fall short of oxygen, they simply die. Recent studies have shown that regeneration in heart cells is possible The syncytium of cardiac muscle is important because it allows rapid coordinated contraction of muscles along their entire length. Action potentials propagate along the surface of the muscle fiber from the point of synaptic contact, through intercalated discs. Although a syncytium, cardiac muscle differs because the cells are not long and multinucleated. Cardiac tissue is therefore described as a functional syncytium, as opposed to the true syncytium of skeletal muscle. Cardiac muscle Molecular structure of the myocardium Myocardiocyte contraction Main contractile elements : •Myosin: thick filaments with globular heads evenly spaced along their length; contains myosin ATPase. •Actin: smaller molecule (thin filaments) consisting of two strands arranged as an alpha-helix, woven between myosin filaments. Regulatory elements: •Tropomyosin: double helix that lies in the groove between actin filaments. It prevents contraction in the resting state by inhibiting the interaction between myosin heads and actin. •Troponin: complex with three subunits that sits at regular intervals along the actin strands. •Troponin T (TnT) – ties troponin complex to actin and tropomyosin molecules. •Troponin I (TnI) – inhibits activity of ATPase in actin-myosin interaction. •Troponin C (TnC) – binds calcium ions that regulate contractile process. Ionic basis of cardiac muscle contraction The mechanism of contraction of cardiac muscle fibers is similar to that in skeletal muscle fibers. As intracellular Ca 2+ concentrations increase, Ca 2+ binds to troponin, causing the tropomyosin to move and thus uncovering the myosin binding sites on the actin fi laments. Myosin then binds to actin, and the actin is pulled across the myosin fi lament. Drugs that alter the movement of calcium into the cardiac muscle fibers can affect the strength of heart contraction. Molecular basis of cardiomyocyte contraction Excitation-contraction coupling in a cardiac fibre The electrocardiogram (ECG) · The electrocardiogram (ECG) is a surface recording of the electrical field generated in the entire body by the heart. The sinus node is a minimal muscle mass, and there is no potential difference (wave in the ECG) before the atria depolarise with a P-wave. When the propagating wave is directed towards the electrode (as in lead II) the atrial depolarization will produce a positive P-wave. · The P-waves correspond to the impulse distribution in the atria, and the QRS-complex origin from depolarisation of the strong ventricular myocardium. · The QRS deflections in two of the three standard leads can be drawn graphically in a triangle and their resultant is the mean QRS-axis of the heart. · The T-wave is caused by the spread of repolarization over the ventricles. · The small propagating wave moving away from the electrode at the apex and to the right to reach the right ventricle, is responsible for the small, negative S-wave. Cardiac cycle The total of events associated with the movement of blood during one heartbeat is called the cardiac cycle Diastole represents the period of time when the ventricles are relaxed ,blood is passively flowing from LA and RA into the LV and RV, respectively . The blood flows through atrioventricular valves (mitral and tricuspid) that separate the atria from the ventricles. Systole represents the time during which the left and right ventricles contract and eject blood into the aorta and pulmonary artery Heart sounds Four sounds are created during each heart beat, and two of these sounds are clearly audible. These sounds are typically described as "lub-dup. The first sound, lub, is louder and longer is the AV valves closing. This occurs at the beginning of systole as the ventricular pressure increases above the atria pressure, causing the AV valves to close as blood begins returning to the atria. The dup sound is caused by the semilunar valves closing at the beginning of ventricular diastole. The two other sounds, which are less audible, are due to the blood turbulence during ventricular filling and atrial systole. Heart murmurs include clicking, rushing, or gurgling sounds. Although not always due to a problem, heart murmurs generally indicate a valve disorder. If the valve is stenotic, meaning it has a narrowed opening, a click may be audible when the valve should be fully opened. In contrast, if a swishing sound is heard when the valve should be closed, it may indicate that blood is able to backfl ow through the valve. Cardiac output Heart rate Autonomic nervous system Circulating catecholamine Chemoreceptors Mechanoreceptor(priopro receptor) Baroreceptor Temperature Cations: Ca, Na, K Stroke volume Preload End diastolic volume Venousreturn Body position Muscular pumping Venous pressure Contractility Force of contraction Catecholamines [Ca] Hypertrophy Afteload Arterial pressure Valve stenosis Cardiac output(CO) The amount of blood pumped by the heart per minute, is a measure of how much work heart is doing. CO is equal to stroke volume (SV), the amount of blood pumped by the ventricle per single heart beat multiplied by the heart rate: CO (mL/min) = SV (mL/beat) × HR (beats/min). SV is equal to end diastolic volume (EDV) minus end systolic volume (ESV). The heart pumps approximately 60% of the blood in its chambers with each beat. Circulating system A- Arteries:There are types of arteries: 1. Elastic or conducting arteries, Largest in diameter , Have high pressure fluctuations ,Provide pressure reservoir 2. Muscular or medium arteries distribution vessels. Smooth muscle allows vessels to regulate blood supply by constricting or dilating 3. Arterioles Transport blood from small arteries to capillaries resistance vessels;, Control the amount of resistance. Greatest drop in pressure occurs in arterioles which regulate blood flow through tissues B- Capillary Beds Capillaries form networks called capillary beds, the capillaries are exchange vessels C- venules and veins are capacitance vessels. The venous system can be expanded to contain more than 75% of the total blood volume. The veins function as capacitance vessels, and become very distended. Severe exercise and loss of blood cause an increase in venous tone, which for a period actually can increase the circulating blood volume. During hard work the muscular venous pump provides up to 1/3 of the energy required for blood circulation (the peripheral venous heart). The venous system also plays an important role by its graded venous return to the heart. Blood flow The total blood volume (5 l) is distributed with 60-75% in veins and venules, 20% in arteries and arterioles, and only 5% in capillaries at rest. Of the total blood volume only 12% are found in the pulmonary low-pressure system. The differences in BP within the vascular system provide the driving force that keeps blood moving from higher to lower pressure areas Blood flow (F) is directly proportional to the difference in blood pressure (ΔP) between two points in the circulation, flows down a pressure gradient Flow = ΔP /R F = flow rate of blood through a vessel ΔP = pressure gradient R = resistance of blood vessels R is more important than ΔP in influencing local blood pressure Blood vessels show resistance against blood flow, the affective resistance from peripheral blood vessels resistances which is regulated by: 1- Radios of blood vessel(SM activity) 2- Viscosity of blood(RBCs ) 3-Length of blood vessel , which is fixed Regulation of Blood pressure Blood pressure (BP) is the pressure exerted by circulating blood upon the walls of blood vessels. Pressure of arterial blood is regulated by blood volume, TPR, and cardiac rate. MAP=CO ´ TPR Arteriole resistance is greatest because they have the smallest diameter. Capillary BP is reduced because of the total cross-sectional area. 3 most important variables are HR, SV, and TPR. Increase in each of these will result in an increase in BP. Long-Term Regulation of Blood Pressure There are 5 mechanisms by which blood pressure is regulated over the long term: 1. Renin-Angiotensin-Aldosterone Mechanism This mechanism detects a fall in blood pressure and initiates a series of events that help to bring blood pressure back to normal. For details on the RAA mechanism. 2. Antidiuretic Hormone (ADH or Vasopressin) Mechanism ADH is released by the posterior pituitary when osmoreceptors in hypothalamus detect an increase in plasma osmolality Dehydration or excess salt intake: Produces sensation of thirst Stimulates water reabsorption from urine in kidneys, elevating blood volume . Atrial Natriuretic Peptide Mechanism Produced by the atria of the heart in response to increased blood pressure Stretch of atria stimulates production of ANP. Antagonistic to aldosterone and angiotensin II. Promotes sodium and water excretion in the urine by the kidney. Promotes vasodilation 4. Fluid Shift Mechanism: Administration of hypertonic fluids e.g. mannitolor hypertonic saline solution Administration of plasma proteinssuch as albumin 5. Epinephrine/Norepinephrine Mechanism Are produced by cells in the adrenal medulla in response to emergency or stressful situations These hormones increase heart rate and blood vessel constriction, result in an increase in blood pressure Regulation of Blood Pressure Short-Term Regulation of Blood Pressure Baroreceptor Reflexes Baroreceptors are sensory receptors that detect changes in blood pressure Baroreceptors are located in the carotid sinus, aortic arch, and other arteries Changes in peripheral resistance, heart rate, and stroke volume occur in response to changes in blood pressure Chemoreceptor Reflexes Chemoreceptors are sensory receptors sensitive to oxygen, carbon dioxide, and pH levels of blood Pressure of arterial blood is regulated by blood volume, TPR, and cardiac rate. Arteriole resistance is greatest because they have the smallest diameter. Capillary BP is reduced because of the total cross-sectional area. 3 most important variables are HR, SV, and TPR. MAP=CO ´ TPR Increase in each of these will result in an increase in BP. BP can be regulated by: Kidney and sympatho-adrenal system Intrinsic Regulation of Blood Flow (Autoregulation) Most tissues (Kidneys, skeletal muscle, brain, liver , and myocardium) have an intrinsic capacity to compensate for moderate changes in perfusion pressure by changes in vascular resistance so blood flow remains constant. Blood flow can increase 7-8 times as a result of vasodilation of metarterioles and precapillary sphincters . Metabolic controle mechanism: Response to increased rate of metabolism Intrinsic receptors sense chemical changes in environment Vasodilator substances produced as metabolism increases Accumulation of metabolites [ increased CO2, H, adenosine/ k from tissue cells, lactic acid, or decrease O2,pH, and ATP ], leads to vasodilation ↓BF→ accumulation of metabolites (adenosine, K+, lactate, ATP) → VD →↑BF Myogenic control mechanism::-Occurs because of the stretch of the vascular smooth muscle - maintains adequate flow.:Depends on the length- tension reletionship ↑ABP→ ↑ BF → stretch of vascular smooth muscle → stretch-induced ms contraction → ↓ BF back to normal) ↓ ABP → ↓BF→ inhibition of smooth ms→ vasodilatation→ ↑BF back to normal A decrease in systemic arterial pressure causes vessels to dilate. A increase in systemic arterial pressure causes vessels to contract Endothelium secretions: Nitric Oxide (NO) causes vasodilation NO diffuses into smooth muscle: Activates cGMP (2nd messenger). Endothelin-1 causes vasoconstriction Extrinsic Regulation of Blood Flow Extrinsic Regulation of Blood Flow 1- Neural regulation Sympathoadrenal Increase cardiac output Increase TPR: Alpha-adrenergic stimulation - vasoconstriction of arteries in skin and viscera Parasympathetic Parasympathetic innervation limited, less important than sympathetic nervous system in control of TPR. Parasympathetic endings in arterioles promote vasodilation to the digestive tract, external genitalia, and salivary glands 2- Hormonal: Vasodilator Vasoconstrictor Kinin Adr & Nor-Adr ANP Angiotensine II VIP ADH ,Natriuretic Blood flow during excersize Heart failure In a normal healthy heart, during each heartbeat a set amount of blood enters the heart and is pumped out again, in heart failure, the heart cannot cope with pumping the full amount of blood in each heartbeat. . Symptoms include fluid retention, breathlessness and tiredness . Heart failure is usually classified on which heart function or which side of the heart is most affected . Systolic heart failure. This means that the ventricles of the heart do not contract properly during each heartbeat so blood is not adequately pumped out of the heart. In some cases there is only a slight reduction in the power of the ventricle, which causes mild symptoms. If the power of the pumping action is more reduced then symptoms become more severe. Diastolic heart failure. This occurs when the ventricle does not fill up with blood enough when the heart rests in between each heartbeat. This can sometimes be due to the wall of the ventricle being stiffer than usual. This makes it more difficult to stretch. .Ischaemic heart disease (IHD) IHD (also called coronary heart disease) is the most common cause of heart failure. In this condition, the blood flow to the heart muscle is reduced by narrowing of the coronary arteries that supply the heart muscle with blood and oxygen. The heart muscle may then not function as well as normal. Other symptoms of IHD may occur such as angina (heart pains Other causes Diseases of the heart muscle (cardiomyopathy). High blood pressure. Diseases of the heart valves. Diseases of the pericardium - Some types of abnormal heart rhythms (arrhythmias). Drugs or chemicals that may damage the heart muscle - for example, alcohol excess, cocaine and some types of chemotherapy. Various non-heart conditions that can affect the function of the heart - for example, severe anaemia. Shock is a clinical condition characterized by a gradual fall in arterial pressure rapid heart rate and Respiration pale, moist and grey skin. cardiac insufficiency Vascular insufficiency circulatory insufficiency the blood flow to vital tissues to be inadequate delivery of oxygen and other nutrients as well as elimination of waste products is insufficient Cardiogenic shock can be caused by restricted ventricular filling (bi- or tricuspidal stenosis, pericardial fibrosis myocardial disorders (infarctions, myocarditis etc) Restricted ventricular ejection in cases with semilunar stenosis/insufficiency or shunts. Vascular shock caused by Absolute hypovolaemia is caused by blood loss, plasma loss (burns , ascites, hydrothorax etc) or dehydration (water deprivation, severe diarhoea or vomiting, excessive sweating, intestinal obstruction with luminal fluid accumulation, urinary loss of proteins/salt/water, excessive use of diuretics). Relative hypovolaemia, vasodilatation , sometimes with universal vasodilatation, is released by endotoxins (septic shock from viral or bacterial infections), anaphylactic shock or by a neurogenic vasodilatation (neurogenic shock by severe pains or stress, anaesthetics or brain stem lesions close to the vasoconstrictor centre). Oedema Oedema is an abnormal clinical state characterised by accumulation of interstitial or tissue fluid. Cutaneous oedemas can be diagnosed by the simple test: pitting on pressure Theoretically, oedemas are caused by three different mechanisms: 1. A hydrostatic pressure gradient, which is too great (so-called high pressure oedema or cardiac oedema at heart failure with increased venous and central venous pressure), 2. A colloid-osmotic pressure gradient, which is too low and caused by too low concentrations of plasma proteins (so-called hunger oedema and renal oedema), 3. Leakage in the capillary endothelium (so-called permeability oedema with too much protein in the oedema fluid). Burns cause increased capillary permeability for proteins, by infections or by allergy. Chronic or congestive cardiac failure Congestive heart failure (CHF) is a condition in which the heart's function as a pump is inadequate to meet the body's needs. The symptoms of congestive heart failure vary, but can include fatigue, diminished exercise capacity, shortness of breath, and swelling. In chronic cardiac failure The weakened heart muscles may not be able to supply enough blood to the kidneys, which then begin to lose their normal ability to excrete salt (sodium) and water. This diminished kidney function can cause the body to retain more fluid. This causes loss of fluid into the interstitial fluid volume. Accumulation of abnormal volumes of interstitial fluid is the definition of oedema.