* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Fatty acid oxidation inhibition with PPARa activation (FOXIB/PPARa
Coronary artery disease wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Heart failure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
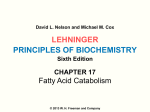
Cardiovascular Research 66 (2005) 423 – 426 www.elsevier.com/locate/cardiores Editorial Fatty acid oxidation inhibition with PPARa activation (FOXIB/PPARa) for normalizing gene expression in heart failure? Heinz Rupp*, Thomas P. Rupp, Bernhard Maisch Molecular Cardiology Laboratory, Department of Internal Medicine and Cardiology, Philipps University of Marburg, Marburg, Germany Received 23 March 2005; accepted 31 March 2005 Available online 19 April 2005 See also article by Lionetti et al. [7] (pages 454 –461) in this issue. 1. Gene expression of overloaded cardiomyocytes In the majority of patients with heart failure, the left ventricle is overloaded and cardiac hypertrophy occurs, which is associated with a dysregulated gene expression. A hallmark of hypertrophied animal hearts is the fetal phenotype, which has been characterized on the basis of a reduced or inadequate expression of a-myosin heavy chain (a-MHC) and the Ca2+ pump (SERCA2) of the sarcoplasmic reticulum (SR) that appears to be a marker of a great number of dysregulated genes [1] also involving Na+ –Ca2+ exchange [2]. During progression of heart failure involving neuroendocrine activation, reprogramming of an even larger group of genes ensues. Microarray data has revealed at least 251 genes that are up- or downregulated upon heart failure [3]. The finding that many of the differentially expressed genes code for enzymes involved in energy metabolism might not be unexpected, since they are also reduced in the fetal period. Repression of genes that are responsible for the oxidation of fatty acids was particularly pronounced [1,4], which is indicative of reduced fatty acid utilization. Glucose oxidation is increased, which might nevertheless be inadequate when insulin resistance occurs [5]. Since PPARa was reduced as a consequence of pressure overload, the switch in * Corresponding author. Molecular Cardiology Laboratory, Department of Internal Medicine and Cardiology, Karl-von-Frisch-Strasse 1, 35033 Marburg, Germany. Tel.: +49 6421 286 5032; fax: +49 6421 286 8964. E-mail address: [email protected] (H. Rupp). fuel metabolism has been attributed to a reduced influence of PPARa [6]. Which of these many alterations represent initial events and are causative for the progression of heart failure? Which represent a compensatory reprogramming of gene expression? Until recently, it was still a matter of dispute whether the overloaded cardiomyocyte contributes to heart failure, and it was thought that deterioration of pump function arises primarily from an adverse remodeling of the extracellular matrix. This controversy can be settled by examining drugs that interfere with the altered gene expression of cardiomyocytes and by assessing consequences for the progression of heart failure. In these experiments, the overload of the heart should not be reduced by the treatment. As an example, antihypertensive ACE inhibitor treatment of infarcted overloaded heart reduces the overload and defects in gene expression of cardiomyocytes, therefore, cannot be traced. Ideally, a given compound should not have acute inotropic or vasodilatory actions. As reported in this issue of Cardiovascular Research, Lionetti et al. [7] studied such a compound in a large animal model of severe heart failure. They addressed the question whether partial inhibition of fatty acid oxidation of the heart in a rapidly progressing model of heart failure due to rapid pacing accelerates or slows heart failure. Keeping in mind that fatty acids are the main fuel for the heart and that the failing heart might already be energy starved [5], the outcome is not straightforward. By blocking mitochondrial carnitine palmitoyltransferase I (CPT I) activity, the already reduced fatty acid utilization is impaired further and an even more prominent shift to glucose utilization is expected. 0008-6363/$ - see front matter D 2005 European Society of Cardiology. Published by Elsevier B.V. All rights reserved. doi:10.1016/j.cardiores.2005.03.023 424 H. Rupp et al. / Cardiovascular Research 66 (2005) 423 – 426 2. Oxfenicine treatment in a dog model of ischemic heart failure Lionetti et al. [7] provide clear evidence that the CPT I inhibitor oxfenicine slowed progression of heart failure and preserved pump function. The treatment delayed the onset of failure by approximately 1 week, reduced left ventricular remodeling and prevented various changes in protein phenotype. In particular, activation of matrix metalloproteinase (MMP)-2 and -9, which are known to be involved in cardiac dilatation, was prevented and enddiastolic diameter was reduced. Since the hearts still failed, it has to be concluded that activation of MMP-2 and -9 only partly contributes to cardiac dilatation, but certainly does not represent an epiphenomenon. The beneficial effects can most probably not be attributed to putatively antioxidative properties of oxfenicine. Another CPT I inhibitor, etomoxir, also retarded dilatation of the pressure-overloaded heart [8], and this compound is not expected to exhibit antioxidative effects. Since the reduction in the mRNA levels of the genes PPARa, RXRa, GAPDH, citrate synthase, m-CPT I, PDK-4 and UCP3 of untreated dogs with heart failure were prevented by oxfenicine, the question emerges whether these genes belong to the group of causative genes for heart failure progression or represent a compensatory reprogramming due to the impaired heart function. At first glance, the findings on oxfenicine might be puzzling. Mechanisms underlying the improvement in heart function become apparent when comparing oxfenicine with etomoxir. Insulin receptor Mitochondrion Etomoxir has been developed as a hypoglycemic and hypolipidemic compound. In contrast to the physiological inhibitor malonyl-CoA, etomoxir inhibits irreversibly a certain proportion of CPT I molecules and thereby reduces the mitochondrial uptake and oxidation of fatty acids (Fig. 1). CPT I inhibition alone, however, would reduce an already diminished fatty acid oxidation of pressure-overloaded hearts. As in the case of statins, the compound appears to have a pleiotropic action. As a consequence of CPT I inhibition, cytoplasmic triacylglycerols and fatty acids are increased and thereby provide additional endogenous PPARa ligands, leading to activation of the important transcription factor PPARa. Because of its fatty acid residue, etomoxir is also expected to be a direct ligand for PPARa. In contrast to established PPARa agonists such as the hypolipidemic fibrates, which increase fatty acid oxidation, etomoxir leads to PPARa activation without increasing fatty acid oxidation; i.e., it belongs to the drug class of ‘‘fatty acid oxidation inhibitors with PPARa activation (FOXIB/PPARa)’’ exhibiting a dual mechanism Glucose Nucleus Sugar intermediates Acetyl-CoA PPARα betaThiolases NADH Acyl-CoA dehydrogenases oxidation Ligand CPT I Malonyl-CoA Oxidation of: inner CPT II Glucose Fatty acids outer membrane CPT I inhibitor Acylcarnitine Carnitine+Acyl-CoA PPARα promoter act. CPT I inhibition +PPARα activation Carnitine + Fatty acid Carnitine Pressure overload PPARα deactivation PPARα promoter act. Carnitine Acylcarnitine Carnitine + Acyl-CoA CACT Gene promoters RXR PDK Citrate Fatty acid oxidation 3. Etomoxir counteracts a dysregulated gene expression of overloaded cardiomyocytes Glucose transporter Glucose PFK Pyruvate Glycolysis Glucose oxidation Although oxfenicine differs in the chemical structure (lhydroxyphenylglycine) from etomoxir (2-[6-(4-chlorophenoxy)hexyl]oxirane-2-carboxylate), both have been developed as CPT I inhibitors and appear to have a similar action in overloaded and failing heart. Fatty acid Endothelial cell Fatty acid Fibrate Fig. 1. Possible protein or metabolite targets (italics) for drugs (underlined) interfering with cardiac energy metabolism. Best characterized is CPT I inhibition, which has a dual mechanism of action by reducing fatty acid oxidation and activating PPARa. Malonyl-CoA is the physiological CPT I inhibitor and can be increased by inhibiting malonyl-CoA decarboxylase. Etomoxir also inhibits acetyl-CoA carboxylase, which controls fatty acid synthesis thereby limiting triacylglycerol accumulation. Lipid-lowering interventions reduce fatty acid supply to the heart and fatty acid oxidation and enhance glucose utilization (Randle cycle) if glucose uptake is not limited due to insulin resistance. Gene promoter mechanisms possibly involving sugar intermediates, PPARa and other metabolic signals are summarized in Refs. [11,16]. Abbreviations: PDK, pyruvate dehydrogenase kinase; CACT, carnitine-acylcarnitine translocase; CPT, muscle-type carnitine palmitoyltransferase; PFK, 6-phosphofructo-1-kinase; PPAR, peroxisome proliferator-activated receptor; RXR, retinoid X receptor; PPARa promoter act., activity of gene promoters with response elements for PPARa. H. Rupp et al. / Cardiovascular Research 66 (2005) 423 – 426 of action. In this respect, an intriguing observation of Lionetti et al. [7] was the marked upregulation of pyruvate dehydrogenase kinase-4 (PDK-4) mRNA, which is a typical response to PPARa activation. However, PPARa activation on its own with an established PPARa agonist had detrimental effects in the pressure-overloaded heart [9]. The dose used was high enough to counteract the reduction of fatty acid oxidation of the pressure-overloaded heart and actually appeared to enhance fatty acid oxidation beyond control values [9]. Chronic etomoxir treatment rescued the down-regulated SERCA2 of hypertrophied, pressure-overloaded hearts back to near normal levels. The SR Ca2+ ATPase activity, Ca2+ uptake rate, number of active Ca2+ pumps [E¨P] and SERCA2 protein and mRNA abundance were increased (see Refs. [10,11] and references therein). Since a reduction in SERCA2 expression results in an impaired Ca2+ handling by the cardiomyocyte, it appears to be a causative defect leading to depression of pump function. Etomoxir also increased the proportion of a-MHC or myosin V1 (2 a-MHC), demonstrating a coordinated expression of genes required for fast relaxation and contraction of the heart. Based on putative regulatory sequences on the SERCA2 promoter, the transcriptional effects of etomoxir have been attributed to a shift in energy metabolism with increased glucose utilization and/or PPARa activation [11]. The etomoxir-induced increase in gene expression of SERCA2 and a-MHC was associated with an improved pump function of the pressure-overloaded heart [8]. Since the high afterload arising from constriction of the ascending aorta cannot be reduced by a drug, direct actions on the cardiomyocyte have to be inferred. At low dosage, etomoxir had a selective influence on the pressure-overloaded left ventricle. Both myocardial working capacity and rates of contraction and relaxation of isovolumically beating hearts were increased. Etomoxir also influenced the transition from apparently compensated to decompensated cardiac hypertrophy [12]. After severe constriction of the ascending aorta, the pronounced left ventricular hypertrophy was associated with pulmonary congestion indicating heart failure. The SR Ca2+ uptake rate per gram wet weight was reduced, which was independent of phospholamban phosphorylation and the inhibition of the SR Ca2+ release mechanism. The SERCA2 protein amount was likewise reduced. The SR Ca2+ uptake rate was inversely correlated with left ventricular weight, but was not influenced by the occurrence of pulmonary edema. Since the calculated SR Ca2+ uptake rate of the whole ventricle was not reduced, a hypertrophy proportional dilution of SR Ca2+ pumps that precedes the occurrence of pulmonary edema appears likely. Etomoxir did not affect left ventricular weight, but reduced right ventricular hypertrophy, which is a consequence of pulmonary edema. In parallel, the SR Ca2+ uptake rate and the proportion of myosin V1 increased. It was concluded that etomoxir represents a candidate drug for the prevention of heart failure pro- 425 gression by increasing the SR Ca2+ uptake rate. In accordance, selective restoration of SERCA2 by adenoviral gene transfer resulted in functional improvement in pressure overload-induced heart failure and normalization of 51 gene transcripts [3], demonstrating the occurrence of compensatory reprogramming of gene expression as a result of impaired function. 4. CPT I inhibition in patients with heart failure Heart failure is a disease with many causes and one cannot simply extrapolate from animal experiments to heart failure in general. Nonetheless, the study by Lionetti et al. [7] is unique because it demonstrates its effects in a largeanimal model of severe heart failure, which follows a predictable time course of transition to decompensation. Thus, compounds referred to as CPT I inhibitors represent not only an effective therapy for heart failure in rat models. Based on the animal experiments, clinical trials in heart failure appear to be a rational consequence. In a pilot study on etomoxir in 10 patients with impaired heart performance but without diabetes mellitus type II, an improved cardiac function was observed after a 3-month treatment [13]. Based on echocardiographic data, it was concluded that the etomoxir treatment had no influence on left ventricular muscle mass. Also, no significant side effects were observed. In acute studies, etomoxir showed neither a positive inotropic effect nor vasodilatory properties [13]. A randomized, placebo-controlled trial including heart failure patients of NYHA classes II – III with no metabolic or other severe diseases was terminated prematurely, however, because side effects had occurred in a small number of patients. Should this drug approach be pursued further? The observed adverse events do not argue against the validity of basic mechanisms underlying the beneficial effects observed in the dog and rat. One should, however, take into account that irreversible CPT I inhibition has its risks if the dosage cannot be maintained due to an impaired drug elimination. Obviously, excessive CPT I inhibition has adverse consequences. Thus, etomoxir can cause lipid accumulation in the rat liver [14]: 125 mg/kg/day of active enantiomeric (+)etomoxir was administered, which is much higher than the dose [15 mg/kg/day racemic (T)-etomoxir corresponding to 7.5 mg/kg/day of active (+)-form] with selective effects in overloaded rat hearts and which only moderately increased lipid droplets in the heart [10]. Lipid accumulation due to CPT I inhibition is expected to be counteracted by the hypolipidemic action of etomoxir [15] arising from a reduced de novo fatty acid synthesis. In future trials, therefore, blood levels of CPT I inhibitors should be determined to detect accumulation of the compound due to possible drug interactions. In summary, the study by Lionetti et al. [7] represents another important step in the search for drugs that not only 426 H. Rupp et al. / Cardiovascular Research 66 (2005) 423 – 426 interfere with neuroendocrine activation but target defects within the overloaded or failing cardiomyocyte. Such studies also help in dealing with the misconception that heart failure is just a symptom and not a disease on its own with causative changes within the cardiomyocytes. Efforts should be strengthened to assess signals associated with cardiac energy metabolism for their potential of correcting a dysregulated phenotype of overloaded and failing cardiomyocytes. In particular, studies on promoter interactions of SERCA2 and related genes involving Ca2+ in addition to metabolic signals [11,16] are required for further drug screening. Restoring the function of hypertrophied cardiomyocytes during early asymptomatic progression of heart failure would be of particular relevance in elderly patients with inadequately treated hypertension. References [1] Stanton LW, Garrard LJ, Damm D, Garrick BL, Lam A, Kapoun AM, et al. Altered patterns of gene expression in response to myocardial infarction. Circ Res 2000;86:939 – 45. [2] Schillinger W, Fiolet JW, Schlotthauer K, Hasenfuss G. Relevance of Na+ – Ca2+ exchange in heart failure. Cardiovasc Res 2003;57: 921 – 33. [3] del Monte F, Dalal R, Tabchy A, Couget J, Bloch KD, Peterson R, et al. Transcriptional changes following restoration of SERCA2a levels in failing rat hearts. FASEB J 2004;18:1474 – 6. [4] Sack MN, Rader TA, Park S, Bastin J, McCune SA, Kelly DP. Fatty acid oxidation enzyme gene expression is downregulated in the failing heart. Circulation 1996;94:2837 – 42. [5] van Bilsen M, Smeets PJ, Gilde AJ, van der Vusse GJ. Metabolic remodelling of the failing heart: the cardiac burn-out syndrome? Cardiovasc Res 2004;61:218 – 26. [6] Barger PM, Brandt JM, Leone TC, Weinheimer CJ, Kelly DP. Deactivation of peroxisome proliferator-activated receptor-alpha during cardiac hypertrophic growth. J Clin Invest 2000;105: 1723 – 1730. [7] Lionetti V, Linke A, Chandler MP, Young ME, Penn MS, Gupte S, et al. Carnitine palmitoyl transferase-I inhibition prevents ventricular remodeling and delays decompensation in pacing-induced heart failure. Cardiovasc Res 2005;66:454 – 61. [8] Turcani M, Rupp H. Modification of left ventricular hypertrophy by chronic etomoxir treatment. Br J Pharmacol 1999;126:501 – 7. [9] Young ME, Laws FA, Goodwin GW, Taegtmeyer H. Reactivation of peroxisome proliferator-activated receptor alpha is associated with contractile dysfunction in hypertrophied rat heart. J Biol Chem 2001;276:44390 – 5. [10] Rupp H, Schulze W, Vetter R. Dietary medium-chain triglycerides can prevent changes in myosin and SR due to CPT-1 inhibition by etomoxir. Am J Physiol 1995;269:R630 – 40. [11] Zarain-Herzberg A, Rupp H. Therapeutic potential of CPT I inhibitors: cardiac gene transcription as a target. Expert Opin Investig Drugs 2002;11:345 – 56. [12] Rupp H, Vetter R. Sarcoplasmic reticulum function and carnitine palmitoyltransferase-1 inhibition during progression of heart failure. Br J Pharmacol 2000;131:1748 – 56. [13] Schmidt-Schweda S, Holubarsch C. First clinical trial with etomoxir in patients with chronic congestive heart failure. Clin Sci (Colch) 2000;99:27 – 35. [14] Steiner S, Wahl D, Mangold BL, Robison R, Raymackers J, Meheus L, et al. Induction of the adipose differentiation-related protein in liver of etomoxir-treated rats. Biochem Biophys Res Commun 1996;218:777 – 82. [15] Rupp H, Elimban V, Dhalla NS. Modification of myosin isozymes and SR Ca2+-pump ATPase of the diabetic rat heart by lipid-lowering interventions. Mol Cell Biochem 1994;132:69 – 80. [16] Rupp H, Zarain-Herzberg A, Maisch B. Drug development based on functional genomics of overloaded cardiomyocytes: CPT1 vs. PPARalpha effects of etomoxir. In: Dhalla NS, Chockalingam A, Berkowitz HI, Singal PK, editors. Frontiers in cardiovascular health. Boston’ Kluwer Academic Publishers; 2003. p. 177 – 94.