* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Сardiac arrhythmias 1. The consequences of continued attack of
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
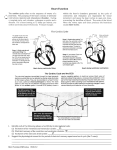
Electrocardiography wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Сardiac arrhythmias 1. The consequences of continued attack of paroxysmal ventricular tachycardia: a) an increase of cardiac output; + b) reduced coronary blood flow; c) increase in systolic blood pressure; d) increasing the stroke volume. 2. To nomotopic arrhythmias does not refer: a) sinus tachycardia; b) sinus bradycardia; c) sinus arrhythmia; d) sick sinus syndrome; +e) ventricular paroxysmal tachycardia. 3. Specify the factors increasing the speed of the slow diastolic depolarization of cell membranes of the sinoatrial node: + a) stimulation of the sympathetic nerves of the heart; b) stimulation of the parasympathetic nerves of the heart; + c) increase in body temperature; d) lowering the temperature of the body; e) an excess of acetylcholine in the blood; + f) administration of epinephrine;+ g) stretching of the sinoatrial node. 4. Specify the factors reducing the speed of the slow diastolic depolarization: a) stimulation of the sympathetic nerves of the heart; + b) stimulation of the parasympathetic nerves of the heart; c) increase in body temperature; + d) lowering the temperature of the body; +e) an excess of acetylcholine; f) administration of epinephrine; g) stretching of the sinoatrial node. 5. Name heterotopic rhythms: + a) Nodal rhythm + b) Migration supraventricular pacemaker c) Sinus tachycardia d) Sinus bradycardia e) Sinus arrhythmia + f) AV-dissociation + g) idioventricular rhythm 6. Specify the factors of formation of ectopic foci: + a) hypercapnia; b) hypocapnia; c) hyperkalemia; + d) hypokalemia; + e) ischemia (hypoxia) of myocardium; f) toxic doses of cardiac glycosides. 7. For premature atrial contraction is characterized by: + a) The presence of P-wave b) The absence of P wave c) Severe deformity ventricular complex + d) Minor changes in ventricular complex e) The full compensatory pause + f) Incomplete compensatory pause 8. For ventricular arrhythmia characterized by: a) The presence of P-wave + b) The absence of P wave + c) Severe deformity ventricular complex d) Minor changes in ventricular complex + e) Full compensatory pause f) Incomplete compensatory pause 9. Name pathogenetic factors of ventricular fibrillation: a) increase in the concentration of intracellular potassium +b) Decrease in the concentration of intracellular potassium +c) Reduction of the membrane potential of cardiomyocytes d) Increase in the membrane potential of cardiomyocytes. 10. Describe the main ECG signs of idioventricular rhythm: a) ventricular complexes has not practically changed; b) ventricular complexes are broadened (more than 0.12 seconds) and strongly deformed; c) the frequency of contractions is 40-60 per minute; + d) the frequency of contractions is 30-40 per minute; + e) rhythm more often regular; f) rhythm more often irregular; g) contractions of atrial and ventricular are coordinated; + h) complete AV-dissociation is typical. 11. For flutter and fibrillation atrial is characterized by: a) Lack of pulses AV-node + b) Partial functional unit of the excitation by AV-node c) The normal conduction of impulses by AV-node 12. Name causes of ventricular fibrillation: + a) passage of electric current through the heart + b) Toxic doses of cardiac glycosides c) Introduction of acetylcholine + d) Severe myocardial hypoxia e) The action of botulinum toxin 13. Extension of PQ interval greater than 0.2 seconds, a constant in a series of subsequent complexes is typical for: a) sinoatrial blockade; b) intraatrial blockade; + c) incomplete AV-blockade of I degree; d) incomplete AV-block II degree with periods of Wenckebach (Mobitts type I); e) incomplete AV-block II degree without periods of Wenckebach (Mobitts type II). 14. Extension of PQ interval greater than 0.2 seconds, increasing in series of subsequent complexes with the loss of one ordinary QRST complex and the appearance the "extra" Pwave is typical for: a) sinoatrial blockade; b) intraatrial blockade; c) incomplete AV-blockade of I degree; + d) incomplete AV-block II degree with periods of Wenckebach (Mobitts type I); e) incomplete AV-block II degree without periods of Wenckebach (Mobitts type II). 15. Regular or chaotic loss of separate ventricular complexes with the constant interval PQ (normal or extended) is characteristic for: a) sinoatrial blockade; b) intraatrial blockade; c) incomplete AV-blockade of I degree; d) incomplete AV-block II degree with periods of Wenckebach (Mobitts type I); +e) incomplete AV-block II degree without periods of Wenckebach (Mobitts type II). 16. Specify the reason of the loss of consciousness, seizures, possibly death at a syndrome of Morgagni-Adams-Stokes a) ventricular fibrillation; + b) transitory asistolia of ventricles. 17. What is characteristic of ventricular fibrillation: a) shortening the diastole and, therefore, deterioration of coronary blood flow; + b) lack of effective ventricular systole. 18. Pacemaker in paroxysmal atrial tachycardia: a) the sinoatrial node; + b) ectopic atrial focus; c) the atrioventricular node; d) several of ectopic foci submitted by individual groups of muscle fibers of the atria. 19. Show pacemaker with paroxysmal ventricular tachycardia: a) the atrioventricular node b) the bundle of His + c) of ectopic foci located in the ventricles d) Some of ectopic foci submitted by individual groups of muscle fibers of the ventricles 20. Show pacemaker when atrial fibrillation: a) the atrioventricular node b) the bundle of His c) of ectopic foci located in the ventricles + d) Several of ectopic foci submitted by individual groups of muscle fibers of the ventricles 21. Specify the pacemaker in atrial flutter: a) the sinoatrial node; + b) ectopic focus located in the atria; c) the atrioventricular node; d) several of ectopic foci, submitted by individual groups of muscle fibers of the atria. 22. Specify the pacemaker when ventricular flutter: a) the atrioventricular node; b) the bundle of His; + c) ectopic focus located in the ventricles; d) several of ectopic foci submitted by individual groups of muscle fibers of the ventricles. 23. Specify the pacemaker when ventricular fibrillation: a) the atrioventricular node; b) the bundle of His; c) ectopic focus located in the ventricles; + d) several of ectopic foci submitted by individual groups of muscle fibers of the ventricles. 24. Show source of impulses at a nodal rhythm: a) the sinoatrial node + b) atrioventricular node c) the bundle of His d) of ectopic foci located in the ventricles 25. Specify the source of impulses when idioventricular rhythm: a) the atrioventricular node; + b) the bundle of His; c) ectopic focus located in the ventricles; d) several of ectopic foci, submitted by individual groups of muscle fibers of the ventricles. 26. Name conditions necessary for the formation of the mechanism of excitation of re-entry (re-entry): a) Accelerated impulse conduction in a small portion of the conductive system (in the twig A Purkinje cells) + b) Delayed impulse conduction in a small section of wire system (a twig A Purkinje cells) + c) One-way flow of excitation in the twig B Purkinje cells d) two-way flow of excitation in the twig B Purkinje cells 27. Fully independent activity of the atria and ventricles, where the impulse from the atria to the ventricles is not carried out, atrial waves do not have constant communication with ventricular complexes thereby the PQ intervals vary continuously along the length and wave P fall into different places and often superimposed on other elements of the electrocardiogram, is typical for: a) sinoatrial blockade; b) intraatrial blockade; c) incomplete AV-blockade I degree; d) incomplete AV-block II degree with periods of Wenckebach (Mobitts type I); + e) AVblockade III degree (complete transverse blockade). 28. Splitting, serration and extension (more than 0.12 seconds) of ventricular complexes with deviation of electrical axis to blocked ventricle, ST-segment shift down, asymmetric negative T waves in leads corresponding to a blocked ventricle, and reverse picture in the opposite leads, is typical for: a) sinoatrial blockade; b) intraatrial blockade; c) incomplete AV-blockade I degree; d) incomplete AV-block II degree with periods of Wenckebach (Mobitts type I); + e) intraventricular blockade. 29. Atrial paroxysmal tachycardia is characterized by: + a) paroxysmal rapid (160-220 per min), the right rhythm from ectopic focus with the presence of ectopic P waves and QRS complexes of correct form; b) paroxysmal rapid (120-220 per min), the right rhythm from ectopic focus with deformed and widened ventricular complexes and P waves, which are completely independent of complexes QRS (atrioventricular dissociation). 30. Ventricular paroxysmal tachycardia is characterized by: a) paroxysmal rapid (160-220 per min), the right rhythm from ectopic focus with the presence of ectopic P waves and QRS complexes of correct form; +b) paroxysmal rapid (120-220 per min), the right rhythm from ectopic focus with deformed and widened ventricular complexes and P waves, which are completely independent of complexes QRS (atrioventricular dissociation). 31. Atrial flutter is characterized by: + a) rhythmical waves F without isoelectric intervals with frequency 220-350 per minute, same height, width and shape; rhythmic and right ventricular complexes; partial functional AV-block (2: 1 or 4: 1); b) chaotic, non-uniform shape, width and height waves f with frequency 350-600 per minute; indiscriminate unchanged ventricular complexes; partial functional block of AVnode. 32. Atrial fibrillation is characterized by: a) rhythmical waves F without isoelectric intervals with frequency 220-350 per minute, same height, width and shape; rhythmic and right ventricular complexes; partial functional AV-block (2: 1 or 4: 1); +b) chaotic, non-uniform shape, width and height waves f with frequency 350-600 per minute; indiscriminate unchanged ventricular complexes; partial functional block of AVnode. 33. Ventricular flutter is characterized by: + a) relatively rhythmic, without isoelectric interval, high and wide, almost identical amplitude of waves, can not be distinguished the complex QRS, ST-segment and the tooth T, with the excitation frequency 150-300 per minute; b) non-rhythmic, low, varying heights and widths, uneven shape, without isoelectric interval waves, forming a chaotic, bizarre curve. 34. Ventricular fibrillation is characterized by: a) relatively rhythmic, without isoelectric interval, high and wide, almost identical amplitude of waves, can not be distinguished the complex QRS, ST-segment and the tooth T, with the excitation frequency 150-300 per minute; +b) non-rhythmic, low, varying heights and widths, uneven shape, without isoelectric interval waves, forming a chaotic, bizarre curve. 35. Specify nomotopic rhythms: a) nodal rhythm; b) migration of supraventricular pacemaker; + c) sinus tachycardia; + d) sinus bradycardia; + e) sinus arrhythmia; f) AV-dissociation; g) idioventricular rhythm. 36. Specify the hemodynamic abnormalities that are typical of early, frequent and group extrasystoles, paroxysmal tachycardia, atrial flutter and atrial fibrillation: a) extend the time of diastolic filling of the heart, significant stretching of muscle fibers at the end of diastole by large amount of blood, intensive work of the heart to expel excess blood volume and, as a consequence, hypertrophy and dilatation of the ventricles; + b) short diastole with reduced filling of the ventricles by blood, reduced stroke volume and cardiac output, ischemia of vital organs, reduction in renal, cerebral, coronary blood flow up to cardiogenic shock. 37. Specify the hemodynamic abnormalities that are typical of full transverse blockade: a) extend the time of diastolic filling of the heart, significant stretching of muscle fibers at the end of diastole by large amount of blood, intensive work of the heart to expel excess blood volume and, as a consequence, hypertrophy and dilatation of the ventricles; + b) short diastole with reduced filling of the ventricles by blood, reduced stroke volume and cardiac output, ischemia of vital organs, reduction in renal, cerebral, coronary blood flow up to cardiogenic shock. 38. Specify the hemodynamic abnormalities that are typical for ventricular fibrillation: a) short diastole with reduced filling of the ventricles by blood, reduced stroke volume and cardiac output, ischemia of vital organs, reduction in renal, cerebral, coronary blood flow up to cardiogenic shock in severe cases; + b) reduction in stroke volume to almost zero, the critical drop in blood pressure and death within minutes. 39. Specify the pathogenetic factors of formation of ectopic foci: a) the excess of acetylcholine in the blood; + b) an excess of adrenaline in the blood; c) increasing the tone of the parasympathetic cardiac nerves; + d) increasing the tone of the sympathetic cardiac nerves. 40. Specify the mechanism of formation of incomplete compensatory pause: + a) emanating excitation from ectopic focus reaches retrogradely sinus node and destroys there formed charge. Since then again begins to form the next normal sinus impulse. Thus, the interval after the beats is equal to one normal RR intervals, plus the time necessary that extrasystolic impulse travels distance from the ectopic source to the sinus node; b) an extraordinary impulse does not pass through the atrioventricular node and does not destroy the charge of sinus node, but as a regular sinus impulse reaches the ventricles when they are covered by the extraordinary contraction and are in the refractory period, ventricles are responsible by contraction only the next sinus impulse.