* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Correlates of Comorbid Antisocial Personality Disorder in
Deinstitutionalisation wikipedia , lookup
Personality disorder wikipedia , lookup
Depersonalization disorder wikipedia , lookup
Antipsychotic wikipedia , lookup
Moral treatment wikipedia , lookup
Political abuse of psychiatry in the Soviet Union wikipedia , lookup
Factitious disorder imposed on another wikipedia , lookup
Child psychopathology wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Substance dependence wikipedia , lookup
Conversion disorder wikipedia , lookup
Anti-psychiatry wikipedia , lookup
Asperger syndrome wikipedia , lookup
Dementia praecox wikipedia , lookup
Mental disorder wikipedia , lookup
Narcissistic personality disorder wikipedia , lookup
Spectrum disorder wikipedia , lookup
Critical Psychiatry Network wikipedia , lookup
Schizoaffective disorder wikipedia , lookup
Substance use disorder wikipedia , lookup
Mental status examination wikipedia , lookup
Abnormal psychology wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Conduct disorder wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Cases of political abuse of psychiatry in the Soviet Union wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Causes of mental disorders wikipedia , lookup
History of mental disorders wikipedia , lookup
Political abuse of psychiatry in Russia wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Antisocial personality disorder wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Political abuse of psychiatry wikipedia , lookup
History of psychiatry wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Schizophrenia wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
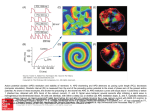
The Correlates of Comorbid Antisocial Personality Disorder in Schizophrenia by Paul Moran and Sheilagh Hodgins cent of the men and 17 percent of the women with schizophrenia met criteria for DSM-III-R APD, in a sample of male forensic patients with schizophrenia the prevalence of APD was estimated to be 27 percent, and in a sample of incarcerated offenders with schizophrenia the prevalence of APD was 63 percent (Hodgins et al. 1996). APD indexes a pattern of antisocial behavior that emerges early in life and that remains stable across the life span. The diagnosis is given when an individual presents a "pervasive pattern of disregard for and violation of the rights of others occurring since age 15 years" (APA 1994, p. 649) and behaviors present before age 15 that meet criteria for a diagnosis of conduct disorder as indicated by "a repetitive and persistent pattern of behavior in which the rights of others or major age-appropriate societal norms or rules are violated" (APA 1994, p. 90). Data from the ECA Study indicate that the risk of schizophrenia increases in a linear fashion with the number of conduct disorder symptoms (Robins and Price 1991). Furthermore, a prospective investigation of a New Zealand birth cohort revealed that 40 percent of the cohort members who developed schizophreniform disorders by age 26 presented conduct disorder as children and/or adolescents (Kim-Cohen et al. 2003). Consistent with these findings are the results of prospective studies of children at high risk for schizophrenia (by virtue of having a mother with the disorder) that have identified a subgroup of boys with behavior problems (Asarnow 1988). In the Copenhagen High-Risk project, it was boys with behavior problems who developed predominately positive-symptom schizophrenia (Cannon et al. 1990). Findings from other prospective investigations (see, e.g., Hodgins and Janson 2002) and several retrospective studies of clinical samples of men with schizophrenia confirm that a subgroup of males who develop schizophrenia dis- Abstract More than 15 years ago, findings from the Epidemiological Catchment Area Study indicated that antisocial personality disorder (APD) is more prevalent among persons with schizophrenia than in the general population. The present study analyzed data from a multisite investigation to examine the correlates of APD among 232 men with schizophrenic disorders, three-quarters of whom had committed at least one crime. Comparisons of the men with and without APD revealed no differences in the course or symptomatology of schizophrenia. By contrast, multivariate models confirmed strong associations of comorbid APD with substance abuse, attention/concentration problems, and poor academic performance in childhood; and in adulthood with alcohol abuse or dependence and deficient affective experience (a personality style indexed by lack of remorse or guilt, shallow affect, lack of empathy, and failure to accept responsibility for one's own actions). At first admission, men with schizophrenia and APD presented a long history of antisocial behavior that included nonviolent offending and substance misuse, and an emotional dysfunction that is thought to increase the risk of violence toward others. Specific treatments and management strategies are indicated. Keywords: Schizophrenia, antisocial personality disorder, treatment, prevention, etiology. Schizophrenia Bulletin, 30(4):791-802, 2004. The prevalence of antisocial personality disorder (APD) is elevated among men and women with schizophrenia as compared to the general population. The Epidemiological Catchment Area (ECA) Study revealed that the prevalence of schizophrenia was 6.9 times higher among men with APD and 11.8 times higher among women with APD than among men and women generally (Robins et al. 1991; Robins 1993). Other studies have confirmed these findings. For example, in a community sample, 23 per- Send reprint requests to Professor S. Hodgins, Box PO23, Department of Forensic Mental Health Science, Institute of Psychiatry, De Crespigny Park, Denmark Hill, London SE5 8AF; e-mail: [email protected]. 791 Schizophrenia Bulletin, Vol. 30, No. 4, 2004 P. Moran and S. Hodgins play a pattern of antisocial behavior both before and after the onset of schizophrenia (Hodgins 2004). Comorbid APD amplifies the suffering of people with schizophrenia. Among men with schizophrenia, comorbid APD is associated with persistent criminality, much of it nonviolent, that begins in adolescence and often leads to imprisonment (Hodgins and Cote 1993), with early-onset substance use, unemployment, and homelessness (Tengstrom and Hodgins 2002). Other studies suggest that the presence of APD among persons with schizophrenia is associated with an increased severity of substance abuse, a greater severity of symptoms of psychosis, higher rates of police contact, and with violent behavior (Mueser et al. 1997, 1999; Gandhi et al. 2001; Moran et al. 2003). Furthermore, a small number of studies have reported that the presence of comorbid APD is associated with poor outcome for the treatment of schizophrenia (Torgalsb0en 1999; Tyrer and Simmonds 2003). The lack of studies of the impact of comorbid APD on response to treatment and outcome in schizophrenia is surprising. This lack may result, at least in part, from the reluctance of individuals with both of these disorders to participate in research (Hodgins et al., in press). Such patients pose enormous difficulties to clinical services, as they fail to comply with treatment and persist in using drugs and alcohol. The association between schizophrenia and APD may also have important implications for understanding the etiology of schizophrenia. For example, consider the evidence on hereditary factors for schizophrenia and for APD. One hypothesis suggests that genetic factors associated with schizophrenia confer vulnerability for antisocial behavior. This hypothesis is supported by findings from family studies demonstrating an elevated prevalence of antisocial behavior and criminality among relatives of persons with schizophrenia (Silverton 1985; Kay 1990) and by the results of two adoption studies showing that schizophrenia in the parental generation increases the risk of criminality among the offspring (Heston 1966; Silverton 1985). An alternative hypothesis suggests that individuals with schizophrenia and APD have inherited a vulnerability for externalizing problems that includes substance abuse. A recent meta-analysis of twin and adoption studies estimated the heritability of externalizing problems at 0.41 (Rhee and Waldman 2002). Children vulnerable for schizophrenia who carry the low-activity variant of the functional polymorphism in the gene encoding monoamine oxidase A genotype could develop stable antisocial behavior as a result of an interaction between this hereditary factor and severe child abuse (Caspi et al. 2002). It has been reported that individuals with schizophrenia spectrum disorders mate disproportionately with antisocial individuals (Parnas 1988). This could be another way in which children inherit one set of genes conferring a vulnerability for schizophrenia spectrum dis- orders and another set conferring a vulnerability for externalizing problems. Just as investigations of hereditary factors associated with schizophrenia have not taken account of antisocial behavior patterns, studies of the role of obstetric complications have not taken account, for example, of the damage that maternal antisocial behavior could do to the developing fetus. Some children with conduct disorder (Frick et al. 2003) and some adults with APD (Cooke and Michie 1997) also display two personality traits included in the syndrome of psychopathy: arrogant and deceitful interpersonal conduct, and deficient affective experience. The first trait does not characterize men with schizophrenia, but deficient affective experience is elevated among offenders with schizophrenia (Tengstrom and Hodgins 2002) and overlaps with negative symptoms. It includes four items: lack of remorse or guilt, shallow affect, lack of empathy, and failure to accept responsibility for one's own actions. It is hypothesized that this trait emerges early in life, contributes to the initiation and maintenance of antisocial behavior, and is associated with repetitive violence (Cooke and Michie 1997; Blair 2003). In summary, there is compelling evidence of an association between schizophrenia and APD and of the harmful consequences for individuals afflicted with both disorders. This association has been the focus of comparatively little research, and the available findings suggest that it may have implications for treatment provision and etiology. The present study was a secondary analysis of data collected from the Comparative Study of the Prevention of Crime and Violence by Mentally 111 Persons (Hodgins et al., in press). The sample included 232 men with schizophrenia who were extensively assessed at discharge from either a general psychiatric hospital or a forensic psychiatric hospital in one of four sites. These men were recruited into a multisite study of community treatment. The four sites (southern British Columbia, Canada; Finland; the state of Hessen in Germany; and southern Sweden) were selected because they all included large catchment areas in which the centralized forensic services treated almost all, if not all, mentally ill persons prosecuted for a criminal offense. The aim of the study was to identify characteristics of persons with schizophrenia and APD that may be of relevance for treatment and service provision, the prevention of criminal behavior, and the etiology of these associated disorders. Method Sample. The sample included 232 men with schizophrenia who had been discharged from either a general psychiatric hospital or a forensic psychiatric hospital in four sites (southern British Columbia, Canada; Finland; the 792 Comorbid Antisocial Personality Disorder Schizophrenia Bulletin, Vol. 30, No. 4, 2004 state of Hessen in Germany; and southern Sweden). One hundred and forty-five (62.5%) of the men had been discharged from a forensic psychiatric hospital, and 87 (37.5%) had been discharged from a general psychiatric hospital. The proportion of the total sample recruited in each site was as follows: Canada, 39 percent (n - 90); Finland, 25 percent (n = 57); Germany, 27 percent (n = 63); and Sweden, 9 percent (n = 22). The mean age of the sample was 38 years (standard deviation [SD] = 11.3), and the principal DSM-IV (APA 1994) diagnoses were schizophrenia (n = 186), schizoaffective disorder (n = 45), and schizophreniform disorder (n = 1). Twenty-two percent of the total sample (n = 51) (95% confidence interval [CI]: 16.7-27.3) met DSM-FV criteria for a comorbid diagnosis of APD: 26 percent (n - 38) of the forensic patients and 15 percent (n = 13) of the general psychiatric patients. In addition, 57 percent (n = 132) (95% CI: 50.5-60.3) of the sample had a diagnosis of alcohol abuse and/or dependence, and 44 percent (n = 101) (95% CI: 37.2^9.9) of the sample had a diagnosis of drug abuse and/or dependence. Psychosocial functioning was low; the mean score on the Global Assessment of Functioning Scale (GAF; Spitzer et al. 1992) for the sample was 49.3 (SD = 13.0), and 60 percent (n = 139) had never had an intimate relationship. The mean age at first admission to the hospital was 24.8 years (SD = 8.8), and the mean number of admissions was 8.0 (SD = 7.1). Three-quarters (n = 173) of these men had been convicted of at least one crime: 99 percent (n - 143) of the forensic patients and 34 percent (n = 30) of the general psychiatric patients. There were 38 participants (16%) who had committed at least one homicide or attempted homicide and all were recruited from a forensic hospital. The mean total number of crimes in the entire sample was 9.9 (SD = 19.2), and the mean total number of violent crimes was 2.6 (SD = 5.0). childhood and adolescence (defined as birth to age 18) was obtained from participants; family members; and school, military, criminal, and medical files. A consensus decision about each variable was made by the research psychiatrist and research assistant after all information had been extracted from files and interviews with patients and family members had been completed. Parents' characteristics. Information on parents was obtained from the participants, family members, and in some cases records. Diagnoses. Primary, secondary, and tertiary diagnoses—lifetime and current—were made using the Structured Clinical Interview for DSM-IV (SCID) for Axis I and II disorders (Spitzer et al. 1992). Experienced psychiatrists who were trained by the developers of the instrument administered the SCID. The psychiatrists in the four sites all spoke English and were trained and tested using videotaped interviews with patients speaking English. Information from participants; family members; school, medical, and social service records; and treatment staff was used to make diagnoses. The use of multiple sources of information was particularly important to corroborate and confirm the diagnosis of conduct disorder. Interrater reliabilities calculated on 38 cases reached K = 1.0 for the principal diagnosis of schizophrenia and K = 0.85 for APD. Psychosocial functioning. Psychosocial functioning was indexed by four variables. Psychiatrists who administered the SCID assessed psychosocial functioning in the 6 months prior to discharge using the GAF. Interrater reliabilities calculated on 33 cases were estimated at K = 0.61. Information about intimate relationships, employment history, and compulsory military service (for the Finnish, German, and Swedish participants) was obtained from participants, family members, and official records. Symptoms. Psychotic symptoms were assessed using the Positive and Negative Syndrome Scale (Kay et al. 1987). Interrater agreement, calculated on 37 cases, reached K = 0.70 for positive symptoms and K = 0.52 for negative symptoms. Personality. Trained research psychiatrists assessed psychopathic traits using the Psychopathy Checklist-Revised (PCL-R; Hare 1991). Three factor scores, as described by Cooke and Michie (2001), were calculated: (1) arrogant and deceitful interpersonal conduct (items 1, 2, 4, and 5); (2) deficient affective experience (items 6-8, and 16); and (3) an impulsive and irresponsible behavioral style (items 3, 9, and 13-15). Interrater agreement, calculated on 38 cases, ranged from K = 0.85 for the total scores, to K = 0.75 for arrogant and deceitful interpersonal conduct, K = 0.75 for deficient affective experience, and K = 0.89 for impulsive and irresponsible behavioral style. Measures Sociodemographic information. Information on sociodemographic characteristics was collected from the participant, family members, and medical files. History of psychiatric treatment. Information on previous psychiatric treatment was extracted from hospital files. Criminality. Information on criminality was extracted from official criminal records. Throughout this article, the term convictions is used broadly to include judgments of nonresponsibility due to a mental disorder. Violent crimes are defined as all offenses causing physical harm, threat of violence or harassment, all types of sexual offenses, illegal possession of firearms or explosives, all types of forcible confinement, arson, and robbery. All other crimes are defined as nonviolent. Childhood and adolescent history of antisocial behavior and academic performance. Information on 793 Schizophrenia Bulletin, Vol. 30, No. 4, 2004 P. Moran and S. Hodgins Procedure. Within each site, each participant with a diagnosis of a major mental disorder being discharged from the forensic hospital was approached and invited to participate in the study. If the participant formally consented to participate, the SCID (Spitzer et al. 1992) was completed. If a diagnosis of a major mental disorder was confirmed, the participant was included in the study and the other interviews and assessments were completed and information was collected from files and collaterals. Patients from general psychiatric hospitals in the same geographical region who had the same sex, similar age (±5 years), and the same principal diagnosis were identified and also invited to participate in the study. If the principal diagnosis was confirmed by the research psychiatrist using the SCID, the same information was collected as for the other participants. APD, compared to those without APD, met criteria for alcohol and drug abuse or dependence. The history of treatment in psychiatric services, psychosocial functioning, and symptoms at discharge did not distinguish those with APD. As would be expected because of the overlap between symptoms of APD and items on the PCL-R, the participants with APD obtained higher mean total PCL-R scores and higher scores on the factor indicating an impulsive and irresponsible behavioral style. Notably, however, they also obtained higher scores on the trait of deficient affective experience, which does not overlap with APD symptoms. The statistical significance of this comparison, however, diminished after applying the Bonferroni correction. Childhood and Adolescent Characteristics. Comparisons of childhood and adolescent characteristics of participants with and without comorbid APD are displayed in table 1. Participants with APD, as compared to those without, were significantly more likely to have experienced attention and concentration problems. While 82 percent of the men with APD abused substances before age 18, so did 41 percent of those without APD. The academic performance of the participants with APD was poorer than that of participants without APD, as early as elementary school, and a significantly greater number of participants with APD had been placed in an institution before 18 years of age. A number of other comparisons were initially statistically significant at the 5 percent level, but the differences failed to meet significance after the Bonferroni correction was applied: earlier onset of symptoms of hyperactivity, depression, and substance misuse; noncompletion of high school education; physical abuse before age 12 years; paternal criminality; and paternal substance abuse. No comparisons of criminality, substance abuse, and mental illness among the mothers and siblings were statistically significant. Data Analysis. All analyses were performed using Stata version 7 (StataCorp 2001). Univariate associations between a DSM-IV diagnosis of comorbid APD and all baseline variables were examined using chi-square tests and, where appropriate, the Fisher exact test for categorical variables and t tests for continuous variables. A Bonferroni correction was applied to account for the use of multiple statistical tests (p = 0.001). Three multivariate models of childhood, adult, and adult criminal correlates of comorbid APD were then determined using forward stepwise logistic regression. To ensure that models were based on exactly the same data, participants with missing values for relevant variables were excluded before modeling. Each model started with the variables that were most significantly associated with comorbid APD at a univariate level. Subsequent variables were then added and likelihood ratio tests were used to determine the significance of adding the new variables to the model. Significant predictors from the childhood/adolescent model and the adult model were then entered into a series of models, to identify the variables that most parsimoniously predicted comorbid APD. History of Criminal Offending. As displayed in table 1, compared to men without APD, participants with APD committed a significantly greater total number of crimes, committed a significantly greater number of nonviolent crimes, and were more likely to have committed a crime before their first admission to general psychiatric services. Notably, neither the mean number of violent crimes nor the proportion of participants in each group who had committed a homicide differed. Results There was no difference in the mean age at entry into the study or the parental occupational status of men with comorbid APD compared to those without comorbid APD (table 1). Adult Mental Disorders, Cognitive Functioning, and Personality. The men with and without comorbid APD did not significantly differ with regard to principal diagnoses, the ages at onset of the prodrome or psychotic symptoms, or the mean number of positive and negative symptoms. A significantly greater proportion of men with Multivariate Models. The first model included the childhood and adolescent variables that significantly distinguished the participants with and without comorbid APD. The analysis included 221 participants with complete data. Four predictor variables were entered into this 794 Schizophrenia Bulletin, Vol. 30, No. 4, 2004 Comorbid Antisocial Personality Disorder Table 1. Comparisons of the characteristics of men with schizophrenia and schizoaffective disorder with and without comorbid APD Variable Sociodemographic characteristics Mean age (yrs) Father's occupation White collar or professional Mother's occupation White collar or professional APD No APD Test P 37.5 (SD= 11.7) 38.3 (SD= 11.2) 4230, n = 232) = 0.5 0.06 16% (7) 30% (47) X 2 (1,n= 199) = 3.6 0.06 15% (7) 19% (31) X 2 (1,n=207) = 0.4 0.05 78% (40) 20% (10) 2%(1) 19.0 (SD = 5.6) 22.3 (SD = 7.9) 81% 19% — 20.3 24.1 (146) (35) X2(2, n = 232) = 3.6 0.2 (SD= 6.7) (SD = 7.7) 498, n = 100) =-0.9 4193, n = 195) = 1.3 0.4 0.2 23.1 (SD = 7.8) 9.1 (SD = 8.6) 25.3 (SD = 9.0) 7.7 (SD = 6.6) 4230, n = 232) = 1.6 4230, n = 232) = 1.2 0.1 0.2 2.1 (SD= 1.9) 2.1 (SD = 2.1) t(225, n = 227) = 0.2 0.9 3.9 (SD = 2.3) 3.8 (SD = 2.3) 4225, n = 227) =-0.1 0.9 77% (39) 65% (33) 5 1 % (93) 38% (68) X 2 (1,n = 232) = 10.2 X 2 1 , n = 232 =11.9 0.001* 0.001* Psychiatric history Had made a previous suicide attempt 55% (28) Mean total length of stay in hospital (mos) 12.9 (SD = 14.7) Mean no. of involuntary admissions 4.2 (SD = 6.1) 49% (88) 12.1 (SD = 20.4) 2.9 (SD = 3.4) x 2 0 . n = 232) = 0.6 4230, n = 232) = -0.2 4230, n = 232) = -2.0 0.4 0.8 0.05 Psychosocial functioning Mean raw score GAF scale Successfully completed military service Employed at least once Has had couple relationship 48.7 22% 86% 39% 49.5 25% 93% 40% 4223, n = 225) = 0.4 x2(2, n = 230) = 0.3 x 2 0 . " = 232) = 2.7 x 2 0 . n = 232) = 0.02 0.7 0.9 0.1 0.9 IQ Mean global IQ Mean verbal IQ Mean performance IQ 89.6 (SD= 12.9) 86.7 (SD = 12.6) 91.0(SD = 14.7) 91.8 (SD = 15.9) 93.4 (SD= 15.5) 89.7 (SD = 17.5) 4174, n = 176) = 0.7 4165, n = 167) = 2.2 4164, n= 166) =-0.4 0.5 0.03 0.7 19.0 (SD = 6.7) 11.9 (SD = 7.4) 4228, n = 230)= -6.1 <0.001* 2.2(SD = 2.1) 4.4 (SD = 2.2) 1.6(SD=1.7) 3.3 (SD = 2.2) 4228, n = 230) = -1.9 4228, n = 230) = -3.0 0.06 0.003 5.7 (SD = 2.3) 4.0(SD = 2.6) 4228, n = 230) = -4.2 <0.001* 73% (37) 8.1 (SD = 3.6) 35% (18) 4.8 (SD = 2.9) 3 1 % (15) 8.5 (SD = 4.8) 38% (68) 9.4(SD = 4.1) 23% (40) 8.6 (SD = 4.3) 30% (53) 11.7 (SD = 4.4) X 2 (1,n = 228)= 18.6 481, n = 83) = 1.6 X 2 (1,n = 228) = 3.4 436, n = 38) = 3.2 X 2 (1,n = 226) = 0.01 459, n = 61) = 2.5 <0.001* 0.1 0.1 0.003 0.9 0.01 Diagnoses Principle diagnosis Schizophrenia Schizoaffective disorder Schizophreniform Mean age of onset of prodrome (yrs) Mean age of onset of psychotic symptoms (yrs) Mean age of first hospitalization (yrs) Mean no. of admissions to hospital Symptoms Mean no. of positive symptoms rated 3 or more on PANSS Mean no. of negative symptoms rated 3 or more on PANSS Comorbid diagnosis Alcohol abuse or dependence Drug abuse or dependence Personality traits Mean PCL-R total score Mean score arrogant and deceitful interpersonal behavior Mean score deficient affective experience Mean score impulsive and irresponsible behavioral style Symptoms before age 18 yrs Attention/concentration problems Mean age of onset (yrs) Hyperactivity Mean age of onset (yrs) Depressive symptoms Mean age of onset (yrs) (SD = 14.4) (11) (44) (20) 795 (SD = 12.6) (45) (169) (73) P. Moran and S. Hodgins Schizophrenia Bulletin, Vol. 30, No. 4, 2004 Table 1. Comparisons of the characteristics of men with schizophrenia and schizoaffective disorder with and without comorbid APD—Continued Variable Substance abuse Mean age of onset (yrs) Anxiety problems Mean age of onset (yrs) APD No APD Test P 2 82% (41) 13.7 (SD = 2.5) 35% (17) 9.8 (SD = 5.6) 4 1 % (73) 14.9 (SD = 2.9) 34% (60) 9.7 (SD = 4.3) X (1,n= 230) = 26.9 /(93, n = 95) = 2.0 X 2 (1,n = 226) = 0.01 /(59, n = 61) = 0.03 <0.001* 0.05 0.9 0.9 Childhood academic performance Below average performance, elementary school Successfully completed high school Placed in an institution before age 18 yrs 48% (24) 16% (8) 49% (25) 2 1 % (36) 40% (69) 24% (43) X 2 (1,n= 224) = 14.8 X 2 (1, n = 222) = 9.9 X 2 (1,n = 229) = 11.7 <0.001* 0.002 <0.001* Childhood victimization Physical abuse before 12 yrs Physical abuse after 12 yrs Childhood sexual abuse Witnessed parental violence 79% 50% 21% 23% 56% 38% 19% 23% X 2 (1,n X 2 (1,n X 2 (1,n X 2 (1,n Paternal history Father with criminal record Father committed violent crime 18% (8) 9% (4) 6% (10) 1%(1) X 2 (1,n = 201) = 5.9 Fisher's exact test 0.02 Father with substance abuse 46% (21) 3 1 % (50) (n=198) X 2 (1,n = 210) = 3.7 0.01 0.05 88% (45) 17.0 (SD = 8.4) 75% (27) 7 1 % (128) 18.7 (SD = 14.6) 36% (40) X 2 (1, n = 232) = 6.4 /(230, n = 232) = 1.1 X 2 (1,n= 146) = 16.3 0.01 0.3 <0.001* 23.3 (SD = 30.0) 5.1 (SD = 8.6) 17.7 (SD = 26.9) 12% (6) 6.1 (SD = 12.53) 1.9(SD = 3.0) 4.0 (SD = 10.6) 18% (32) t(230, n = 232) = -6.0 t{230, n = 232) = 2.6 /(230, n = 232) = 3.6 X 2 (1,n = 232) = 1.0 <0.001* 0.01 0.001* 0.3 Criminal history Convicted of one or more crimes Mean age of first judgment (yrs) Crime before first admission to general psychiatry Mean total no. of crimes Mean total no. of violent crimes Mean total no. of nonviolent crimes At least one judgment for homicide (38) (24) (10) (14) (97) (66) (31) (40) = 220) = 221) = 214) = 217) = = = = 8.2 2.2 0.2 1.0 0.004 0.1 0.7 0.3 Note.—APD = antisocial personality disorder; GAF = Global Assessment of Functioning; PANSS = Positive and Negative Syndrome Scale; PCL-R = Psychopathy Checklist-Revised; SD = standard deviation. * Significant association at p = 0.05 after Bonferroni correction for multiple comparisons. model: attention/concentration problems, substance abuse, below-average performance at elementary school, and being placed in an institution before age 18. Likelihood ratio tests indicated that the best model of childhood correlates of APD included three variables: attention/concentration problems before age 18 (adjusted odds ratio: 2.83; 95% CI 1.34-5.94); substance abuse before age 18 (adjusted odds ratio: 5.44; 95% CI 2.41-12.28); and below-average performance at elementary school (adjusted odds ratio: 2.91; 95% CI 1.39-6.11). This model could not be improved upon to a statistically significant degree by the addition of further variables and yielded an overall likelihood ratio statistic of 46.96 (p < 0.001). The three significant variables often co-occur; therefore, we examined the proportions of participants characterized by these variables. Among the men with comorbid APD, 32 percent were characterized by all three variables; 40 percent were characterized by two variables; 26 percent by one variable; and 2 percent by none of the three variables. The second model included variables that distinguished the participants with and without comorbid APD in adulthood. The analysis included 230 participants with complete data. Lifetime DSM-IV diagnoses of alcohol abuse or dependence and drug abuse or dependence were entered as predictors because they had significantly distinguished the participants with and without comorbid APD in univariate analyses. While the total PCL-R scores and the scores for impulsive and irresponsible behavioral style were significantly different for the participants with and without APD, they were not entered into the model because they overlap with a diagnosis of APD. The score for deficient affective experience may be important in 796 Comorbid Antisocial Personality Disorder Schizophrenia Bulletin, Vol. 30, No. 4, 2004 understanding antisocial behavior among persons with schizophrenia. It was therefore entered into the model even though the univariate comparison was not significant once the Bonferroni correction was applied. Site of recruitment and hospital at discharge (forensic or general) were also entered as covariates. The best model of adult clinical correlates of APD included three variables: adult alcohol abuse or dependence (adjusted odds ratio: 2.92; 95% CI 1.38-6.15); adult drug abuse or dependence (adjusted odds ratio: 2.39; 95% CI 1.21^.72); and deficient affective experience (adjusted odds ratio: 1.25; 95% CI 1.07-1.46). This model could not be improved upon to a statistically significant degree by the addition of any further variables and yielded an overall likelihood ratio statistic of 27.8 (p < 0.001). Notably, among the participants with schizophrenia and co-occurring APD, 37 percent were characterized by all three variables; 41 percent were characterized by two; 18 percent by one; and 4 percent by none of the variables. A final parsimonious model was determined (table 2). This analysis included 220 participants with complete data. The following variables were entered into this model: attention/concentration problems before age 18, substance abuse before age 18, below-average performance at elementary school, DSM-IV lifetime diagnoses of alcohol abuse or dependence and drug abuse or dependence, deficient affective experience, site of recruitment, and type of discharge. The most parsimonious model of comorbid APD included five predictor variables: substance abuse before age 18, below-average performance at elementary school, attention/concentration problems before age 18, adult alcohol abuse or dependence, and deficient affective experience. The model could not be improved upon to a statistically significant degree by the addition of further variables and yielded an overall likelihood ratio statistic of 56.2 (p < 0.001). As with the previous multivariate models, many of the participants with comorbid APD were characterized by the co-occurrence of several of these variables. Among the men with comor- bid APD, 14 percent were characterized by all five predictors, 44 percent by four, 22 percent by three, 18 percent by two, and 2 percent by one. Finally, a model was determined using variables descriptive of participants' criminal careers. The following variables were entered into this model: total number of crimes, total number of violent crimes, total number of nonviolent crimes, having a criminal conviction before first admission to general psychiatry, site of recruitment, and type of discharge. The best model of criminal correlates included only two variables: total number of crimes (adjusted odds ratio: 1.03; 95% CI 1.01-1.05) and having a criminal conviction before first admission to general psychiatry (adjusted odds ratio: 3.13; 95% CI 1.23-7.94). Discussion Among this large sample of men with schizophrenia, those with and without comorbid APD did not differ in their mean age at onset of prodrome, mean age at onset of psychosis, or levels of positive and negative symptoms at discharge. Furthermore, their history of treatment did not differ; mean age at first admission, average number of inpatient stays, and total length of all admissions were similar for the two groups. These findings support results from previous studies (Hodgins et al. 1996, 1998; Hodgins 2000; Tengstrom and Hodgins 2002). While neither the schizophrenic disorder, nor timing and length of hospital care, differed for men with and without APD, criminality did differ. Those with APD, as compared to those without, committed more nonviolent criminal offenses, and significantly more of them began offending before their first admission to a psychiatric ward. This finding supports results from previous studies of offenders with schizophrenia, indicating that the criminal careers of those with APD begin before first admission to psychiatric service and involve primarily nonviolent offending (Tengstrom et al. 2001; Hodgins and Janson 2002; Hodgins 2004). Notably, neither violent offending Table 2. Multivariate model of best predictors of comorbid APD1 Variable Odds ratio (95% CI) p value Substance abuse before age 18 4.48(1.93-10.42) <0.001 Below-average performance at elementary school 2.85(1.33-6.11) 0.007 Attention/concentration problems before age 18 2.70(1.25-5.78) 0.01 Adult alcohol abuse or dependence 2.78(1.23-6.28) 0.01 Deficient affective experience 1.18(1.00-1.40) 0.05 Note.—APD = antisocial personality disorder; CI = confidence interval. 1 All odds ratios are adjusted for the effects of other variables in the model. 797 Schizophrenia Bulletin, Vol. 30, No. 4, 2004 P. Moran and S. Hodgins nor homicide was found to be associated with APD. This finding is consistent with the observation that there are several distinct subgroups of offenders with schizophrenia (Hodgins 2004). The men who developed comorbid APD had experienced numerous difficulties in childhood and early adolescence. In addition to presenting conduct disorder, a significantly greater proportion of those with APD, compared to those without APD, presented attention/concentration problems in childhood and poor academic performance as early as elementary school. Neither of these symptoms is included in the diagnosis of conduct disorder. While truancy from school is a symptom of conduct disorder, it is more common among teenagers than among elementary school children and is not usually the cause of poor performance in elementary school. In our view, the poor early academic performance of this group is related to a combination of factors, including behavior problems, attention and concentration difficulties, and low verbal IQ. Low verbal IQ has been found to characterize children who develop conduct disorder (Moffitt and Caspi 2001). In addition, before the age of 18, a greater proportion of the men with APD had spent time in an institution, had been physically abused, and had fathers who had criminal careers and who abused alcohol and drugs. The significance of some of these associations diminished after the Bonferroni correction was applied, perhaps as a result of insufficient sample size. However, these trends suggest that boys developing both schizophrenia and APD experience multiple problems compounded by an adverse family situation. Given the implications of the findings from the present study, replications with larger samples and prospectively collected data are warranted. Results from the present study highlight the need for early childhood interventions to reduce antisocial behavior and to improve academic performance, family relationships, and parenting practices for children and adolescents at risk for schizophrenia. While interventions for reducing childhood conduct problems have been shown to be effective (Scott et al. 2001), the impact on children with conduct problems who are at risk for schizophrenia is unknown. Eliminating conduct problems among children vulnerable for schizophrenia could prevent future criminality and substance misuse, provide them with skills to cope with schizophrenia if it does develop, and could possibly reduce the likelihood of developing schizophrenia. Conduct-disordered children are exposed to alcohol and drugs at an earlier age than other children and go on to develop more enduring and severe substance abuse problems (Robins and McEvoy 1990; Armstrong and Costello 2002). In light of the recent evidence showing that heavy cannabis abuse during adolescence increases the risk of schizophrenia (Arseneault et al. 2002; Zammit et al. 2002), intervening to reduce conduct disorder among children with a family history of schizophrenia spectrum disorders could reduce cannabis abuse and thereby lower their risk of developing schizophrenia. The effective treatment of conduct disorder during childhood would reduce antisocial behaviors and increase prosocial skills. If schizophrenia did develop, these skills might serve to increase compliance with treatment and prevent substance misuse and crime. While the effective treatment of conduct disorder among children with a family history of schizophrenia would appear to have many benefits, treatment for childhood attention and concentration problems is potentially problematic. Stimulant medications could theoretically alter an already fragile dopaminergic system and increase the risk of later psychoses. Preventing the development of APD in general, and specifically among persons who develop schizophrenia, is a goal worth striving toward. APD is almost always accompanied by substance abuse, and this interferes with treatments for both schizophrenia and antisocial behavior (Buhler et al. 2002; Hunt et al. 2002). Recent evidence also suggests that substance abuse may lead to more severe brain damage among men with schizophrenia as compared to those without (Mathalon et al. 2003). The men with schizophrenia and comorbid APD obtained higher ratings on the trait of deficient affective experience than the men without APD. This trait has been found to be associated with repeated violence toward others (Cooke and Michie 1997; Blair 2003). Animal research has shown that the recognition of distress in potential victims limits aggressive behavior. Individuals who obtain high scores for deficient affective experience are thus unrestrained because they fail to empathize with those they hurt. While this trait is hypothesized to be the core of the syndrome of psychopathy (Cooke and Michie 1997; Blair 2003), it may also occur in conjunction with schizophrenia. The results of the present study have implications for both clinicians and researchers. Men with schizophrenia and comorbid APD require specific interventions not only to ensure compliance with treatment for schizophrenia but also to reduce antisocial behavior and substance abuse and to develop prosocial skills (Hodgins and MiillerIsberner 2000). Specific cognitive-behavioral programs have been found to be effective in reducing offending and increasing prosocial skills with offenders without mental illness (McGuire 1995; Welsh et al. 2002). Preliminary trials of such programs with offenders who have schizophrenia are currently underway. Furthermore, men with schizophrenia and APD require community placements in neighborhoods that support prosocial behaviors and limit access to offenders, weapons, and drugs (Silver 2000). In this study, we found that by the time the men with comor- 798 Comorbid Antisocial Personality Disorder Schizophrenia Bulletin, Vol. 30, No. 4, 2004 bid APD were first admitted to the general psychiatric service, they had a long history of antisocial behavior, substance abuse, poor academic failure, and an adverse family environment, and many already had a criminal record. There was, therefore, ample evidence for general psychiatric services to identify needs for specific treatments and services in addition to those traditionally provided to first onset cases of schizophrenia. Ideally, such patients require thorough assessments once the psychotic symptoms are reduced, to identify comorbid APD. Such patients are likely to require complex treatment plans adapted to their antisocial personality and placement in neighborhoods that support and promote positive change. Currently, general psychiatric services in most Western nations do not have adequate resources and time to provide such assessments and services. Yet the human and financial costs of not providing such services are high. The study has a number of strengths. To the best of our knowledge, it is the first multicenter investigation of comorbid APD in schizophrenia. Previous studies have relied on samples of patients drawn from single centers, thereby reducing the generalizability of their findings. Well-trained, experienced clinical raters made the assessments, using standardized measures, and information on childhood was obtained from multiple sources. Nevertheless, the study has some weaknesses. The sample was weighted for criminal offending, but, based on the results of previous studies, not for APD. Given that the aim of the study was to identify correlates of comorbid APD among men with schizophrenia, the associations in our view are generalizable. The findings from the present study do, however, need to be replicated, preferably in a sample more representative of the population of persons with schizophrenia. Despite the expertise of the research psychiatrists, it proved very difficult to retrospectively identify the age of onset of the prodrome and of psychosis. By contrast, the retrospective diagnosis of conduct disorder was less difficult to make, because multiple sources of information were used to identify externalizing problems in childhood. Although we tried to reduce type I statistical error in the univariate analyses by using the Bonferroni correction, such "playing with p values" may be undesirable. It implies that all outcomes have equal priority and therefore reduces the power to detect real differences. We also acknowledge the limitations of using cross-sectional data to explore etiologic pathways. These data do, however, identify hypotheses for testing in future studies. Armstrong, T, and Costello, E.J. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology, 70:1224-1239, 2002. Arseneault, L.; Cannon, M.; Poulton, R.; Murray, R.; Caspi, A.; and Moffitt, T.E. Cannabis use in adolescence and risk for adult psychosis: Longitudinal prospective study. British Medical Journal, 32:1212-1213, 2002. Asarnow, J.R. Children at risk for schizophrenia: Converging lines of evidence. Schizophrenia Bulletin, 14(4):613-631, 1988. Blair, R.J.R. Neurobiological basis of psychopathy. British Journal of Psychiatry, 182:5-7, 2003. Buhler, B.; Hambrecht, M.; Loffler, W.; an der Heiden, W.; and Hafner, H. Precipitation and determination of the onset and course of schizophrenia by substance abuse: A retrospective and prospective study of 232 populationbased first illness episodes. Schizophrenia Research, 54(Suppl 3):243-251, 2002. Cannon, T.D.; Mednick, S.A.; and Parnas, J. Antecedents of predominantly negative and predominantly positive symptom schizophrenia in a high-risk population. Archives of General Psychiatry, 47:622-632, 1990. Caspi, A.; McClay, J.; Moffitt, T.E.; Mill, J.; Martin, J.; Craig, I.W.; Taylor, A.; and Poulton, R. Role of genotype in the cycle of violence in maltreated children. Science, 297(5582):851-853, 2002. Cooke, D.J., and Michie, C. An item response theory evaluation of Hare's Psychopathy Checklist. Psychological Assessment, 9:2-13, 1997. Cooke, D.J., and Michie, C. Refining the construct of psychopathy: Toward a hierarchical model. Psychological Assessment, 13:171-188,2001. Frick, P.J.; Cornell, A.H.; Bodin, S.D.; Dane, H.E.; Barry, C.T.; and Loney, B.R. Callous-unemotional traits and developmental pathways to severe conduct problems. Developmental Psychology, 39(2):246-260, 2003. Gandhi, N.; Tyrer, P.; Evans, K.; McGee, A.; Lamont, A.; and Harrison-Read, P. A randomised controlled trial of community-oriented and hospital-oriented care for discharged psychiatric patients: Influence of personality disorder on police contracts. Journal of Personality Disorders, 15:94-102,2001. Hare, R.D. The Hare Psychopathy Checklist-Revised: Manual. Toronto, Canada: Multi-Health Systems, 1991. Heston, L.L. Psychiatric disorders in foster-home reared children of schizophrenics. British Journal of Psychiatry, 112:819-825, 1966. References American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: APA, 1994. Hodgins, S. The etiology and development of offending among persons with major mental disorders. In: Hodgins, S., ed. Violence Among the Mentally III: Effective 799 Schizophrenia Bulletin, Vol. 30, No. 4, 2004 P. Moran and S. Hodgins Treatments and Management Strategies. Dordrecht, The Netherlands: Kluwer Academic, 2000. pp. 89-116. Hodgins, S. Criminal and antisocial behaviors and schizophrenia: A neglected topic. In: Gattaz, W., and Hafner, H., Mathalon, D.H.; Pfefferbaum, A.; Lim, K.O.; Rosenbloom, M.J.; and Sullivan, E.V. Compounded brain volume deficits in schizophrenia-alcoholism comorbidity. Archives of General Psychiatry, 60:245-252, 2003. eds. 5th Search for the Causes of Schizophrenia. McGuire, J., ed. What works: Reducing reoffending— Guidelines from research and practice. Chichester, U.K.: Wiley, 1995. Darmstadt, Germany: Steinkopff Verlag, 2004. pp. 315-341. Hodgins, S., and Cote, G. The criminality of mentally dis- Moffitt, T.E., and Caspi, A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology, 13:355-375, 2001. ordered offenders. Criminal Justice and Behavior, 28:115-129, 1993. Hodgins, S.; Cote, G.; and Toupin, J. Major mental disorders and crime: An etiologic hypothesis. In: Cooke, D.; Forth, A.; and Hare, R.D., eds. Psychopathy: Theory, Research and Implications for Society. Dordrecht, The Netherlands: Kluwer Academic, 1998. pp. 231-256. Hodgins, S., and Janson, C-G. Criminality and Violence Moran, P.; Walsh, E.; Tyrer, P.; Burns, T; Creed, F.; and Fahy, T. The impact of co-morbid personality disorder on violence in psychosis—data from the UK700 trial. British Journal of Psychiatry, 182:129-134, 2003. Mueser, K.T.; Drake, R.E.; Ackerson, T.H.; Alterman, A.I.; Miles, K.M.; and Noordsy, D.L. Antisocial personality disorder, conduct disorder, and substance abuse in Among the Mentally Disordered: The Stockholm Metropolitan Project. Cambridge, U.K.: Cambridge University Press, 2002. schizophrenia. Journal of Abnormal Psychology, Hodgins, S., and Miiller-Isberner, R., eds. Violence, Crime and Mentally Disordered Offenders: Concepts and Methods for Effective Treatment and Prevention. 106:473-477, 1997. Mueser, K.T.; Rosenberg, S.D.; Drake, R.E.; Miles, K.M.; Wolford, G.; Vidaver, R.; and Carrieri, K. Conduct disorder, antisocial personality disorder and substance use disorders in schizophrenia and major affective disorders. Journal of Studies on Alcohol, 60:278-284, 1999. Chichester, U.K.: John Wiley and Sons, 2000. Hodgins, S.; Tengstrom, A.; Ostermann, R.; Eaves, D.; Hart, S.; Konstrand, R.; Levander, S.; Miiller-Isberner, R.; Tiihonen, J.; Webster, C D . ; Eronen, M.; Freese, R.; Jockel, D.; Kreuzer, A.; Levin, A.; Maas, S.; Repo, E.; Ross, D.; Tuninger, E.; Kotilainen, I.; Vaananen, K.; Vartianen, H.; and Vokkolainen, A. An international comparison of community treatment programs for mentally ill persons who have committed criminal offences. Criminal Justice and Behavior, in press. Parnas, J. Assortative mating in schizophrenia: Results from the Copenhagen High-Risk Study. Psychiatry, 51:58-64,1988. Rhee, S.H., and Waldman, I.D. Genetic and environmental influences on antisocial behavior: A meta-analysis of twin and adoption studies. Psychological Bulletin, 128:490-529,2002. Hodgins, S.; Toupin, J.; and Cote, G. Schizophrenia and antisocial personality disorder: A criminal combination. In: Schlesinger, L.B., ed. Explorations in Criminal Psychopathology: Clinical Syndromes with Forensic Implications. Springfield, IL: Charles C. Thomas, 1996. pp. 217-237. Robins, L.N. Childhood conduct problems, adult psychopathology, and crime. In: Hodgins, S., ed. Mental Disorder and Crime. Newbury Park, CA: Sage Publications, 1993. pp. 173-207. Robins, L.N., and McEvoy, L. Conduct problems as predictors of substance abuse. In: Robins, L.N., and Rutter, M., eds. Straight and Deviant Pathways From Childhood to Adulthood. Cambridge, U.K.: Cambridge University Press, 1990. pp. 182-204. Hunt, G.E.; Bergen, J.; and Bashir, M. Medication compliance and comorbid substance abuse in schizophrenia: Impact on community survival 4 years after a relapse. Schizophrenia Research, 54(Suppl 3):253-264, 2002. Kay, S.R. Significance of the positive-negative distinction in schizophrenia. Schizophrenia Bulletin, 16(4):635-652, 1990. Kay, S.R.; Fiszbein, A.; and Opler, L.A. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13(2):261-276, 1987. Robins, L.N., and Price, R.K. Adult disorders predicted by childhood conduct problems: Results from the NIMH Epidemiologic Catchment Area project. Psychiatry, 54:116-132, 1991. Robins, L.N.; Tipp, J.; and Przybeck, T. Antisocial personality. In: Robins, L.N., and Regier, D., eds. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: Mac mi 11 an/Free Press, 1991. pp. 258-290. Kim-Cohen, J.; Caspi, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; and Poulton, R. Prior juvenile diagnoses in adults with mental disorder. Archives of General Psychiatry, 60:709-714, 2003. 800 Comorbid Antisocial Personality Disorder Schizophrenia Bulletin, Vol. 30, No. 4, 2004 Sheilagh Hodgins, Ph.D., Institute of Psychiatry, King's College, London; Derek Eaves, M.D., Vancouver, Canada; Markku Eronen, M.D., Ph.D., Vanha Vaasa Hospital, Vaasa, and Niuvanniemi Hospital, Kuopio, Finland; Stephen Hart, Ph.D., Simon Fraser University, Burnaby, Canada; Robert Kronstrand, Ph.D., Rattsmedicinalverket and Linkoping University, Linkoping, Sweden; Sten Levander, M.D., Ph.D., University Hospital, MAS, Malmo, Sweden; Riidiger Miiller-Isberner, Dr.med., Klinik filr forensische Psychiatrie Haina, Haina (Kloster), Germany; Jari Tiihonen, M.D., Ph.D., University of Kuopio, Finland; Christopher Webster, Ph.D., Simon Fraser University, Burnaby, Canada, and McMaster University, Hamilton, Canada; Roland Freese, M.D., Klinik fiir forensische Psychiatrie Haina, Haina (Kloster), Germany; Andrea Grabovac, M.D., Riverview Hospital, Vancouver, Canada; Dieter Jockel, D.med., Klinik fiir forensische Psychiatrie Haina, Haina (Kloster), Germany; Artur Kreuzer, Dr.jur., Justus Liebig University, Giessen, Germany; Alexander Levin, M.D., Vancouver General Hospital, Vancouver, Canada; Stephanie Maas, Klinik fiir forensische Psychiatrie Haina, Haina (Kloster), Germany; Eila Repo-Tiihonen, M.D., Ph.D., Niuvanniemi Hospital, Kuopio, Finland; Deborah Ross, M . S c , Riverview Hospital, Coquitlam, Canada; Eva Tuninger, M.D., University Hospital, MAS, Malmo, Sweden; Irma Kotilainen, M.D., University of Kuopio, Kuopio, Finland; Kirsi Vaananen, Niuvanniemi Hospital, Kuopio, Finland; Paivi Toivonen, M.D., Vanha Vaasa Hospital, Vaasa, Finland; Heikki Vartiainen, M.D., Ph.D., Helsinki Central University Hospital, Helsinki, Finland; Aila Vokkolainen, Vanha Vaasa Hospital, Vaasa, Finland; Jean-Francois Allaire, M.Sc, Institut Philippe Pinel de Montreal, Montreal, Canada; and Anders Tengstrom, Ph.D., MariaUngdom Research Centre, Karolinska Institute, Stockholm, Sweden. Grants to support this study have been awarded by the following sources: 1. The European Union's BIO-MED-II program. Scott, S.; Spender, Q.; Doolan, M.; Jacobs, B.; Aspland, H.; and Webster-Stratton, C. Multicentre controlled trial of parenting groups for childhood antisocial behaviour in clinical practice. British Medical Journal, 323:194-198, 2001. Silver, E. Race, neighbourhood, disadvantage, and violence among persons with mental disorders: The importance of contextual measurement. Law and Human Behavior, 24(Suppl 4):449^56, 2000. Silverton, L. Crime and the Schizophrenia Spectrum: A Study of Two Danish Cohorts. Unpublished doctoral dissertation, University of Southern California, 1985. Spitzer, R.L.; Williams, J.B.W.; Gibbon, M.; and First, M.B. The Structured Clinical Interview for DSM-III-R (SCID) I: History, rationale, and description. Archives of General Psychiatry, 49:624-629, 1992. Stata Corporation. Stata Statistical Software. Release 7.0. College Station, TX: Stata Corporation, 2001. Tengstrom, A., and Hodgins, S. Assessing psychopathic traits among persons with schizophrenia: A way to improve violence risk assessment. In: Blaauw, E., and Sheridan, L., eds. Psychopaths: Current International Perspective. The Hague, The Netherlands: Elsevier, 2002. pp. 81-111. Tengstrom, A.; Hodgins, S.; and Kullgren, G. Men with schizophrenia who behave violently: The usefulness of an early- versus late-start offender typology. Schizophrenia Bulletin, 27(2):205-218, 2001. Torgalsb0en, A-K. Co-morbidity in schizophrenia: A prognostic study of personality disorders in recovered and non-recovered schizophrenia patients. Scandinavian Journal of Psychology, 40:147-152, 1999. Tyrer, P., and Simmonds, S. Treatment models for those with severe mental illness and comorbid personality disorder. British Journal of Psychiatry, 182(Suppl): 15—18, 2003. Welsh, B.C.; Farrington, D.P.; Sherman, L.W.; and MacKenzie, D.L. What do we know about crime prevention. International Annals of Criminology, 40(1/2): 11-31, 2002. Zammit, S.; Allebeck, P.; Andreasson, S.; Lundberg, I.; and Lewis, G. Self-reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: Historical cohort study. British Medical Journal, 325:1199-1201,2002. 2. Funding in Canada came from the Forensic Psychiatric Services Commission of British Columbia; the Mental Health, Law, and Policy Institute, Simon Fraser University; Riverview Hospital. 3. Funding in Finland came from Niuvanniemi and Vanha Vaasa State Mental Hospitals. 4. Funding in Germany came from Deutsche Forschungsgemeinschaft, Institut fiir forensische Psychiatrie Haina. 5. Funding in Sweden came from Medicinska Forskningradet, Vardalstiftelsen; National Board of Acknowledgments The Comparative Study of the Prevention of Crime and Violence by Mentally 111 Persons is being conducted by 801 Schizophrenia Bulletin, Vol. 30, No. 4, 2004 P. Moran and S. Hodgins Forensic Medicine; Forensic Science Centre, Linkoping University; and Linkoping University. The Authors Paul Moran is funded by a postdoctoral fellowship awarded by the National Health Service National Programme on Forensic Mental Health. The views expressed in this article are those of the authors and not necessarily those of the Programme or the U.K. Department of Health. 802 Paul Moran, M.D., MRCPsych, is Postdoctoral Research Fellow and Honorary Consultant Psychiatrist, Health Services Research Department, Institute of Psychiatry, London, U.K. Sheilagh Hodgins, M.Sc, Ph.D., is Head, Department of Forensic Mental Health Science, Institute of Psychiatry, London, U.K.