* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
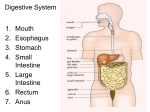
Abdominal viscera Introduction Stomach Small intestines Large intestines Liver pancreas Spleen 26/06/2016 BAAB @2016 Abdominal viscera are organs of the abdominal cavity. They are divided into intraperitoneal which are covered (surrounded) by the peritoneum and extraperitoneal organs which are outside the peritoneum. Some organs share the two sides, they are both intra and extra peritoneal. All extra peritoneal organs are found in the posterior abdominal wall unlike the anterior abdominal wall which is formed of the rectus sheeth. Location and structure: This is a dilated organ of the alimentary canal situated between the esophagus and the small intestines. It occupies the left upper quadrant, epigastric and the umbilical region much of it undercover of the lower ribs. Its long axis passes downwards anf forward to right and then backward and slightly backward. It is roughly J-shaped with two openings cardiac and pyloric orifices. It has two curvetures, greater (extending from left of the cardiac orifice over the dome of the fundus through the left border to the pylorus) and lesser curveture (right border). It has two surfaces, anterior and posterior surfaces. The surfaces are covered by the omentum which forms the lesser omentum or gastrosplenic ligament to attach to the spleen and the greater omentum which extend to the transverse colon. The stomach is divided into the following parts: ◦ Fundus: dome – shaped projecting upwardly and to the left of the cardiac, usually full of gas. ◦ body: extending from the level of the cardiac orifice to the level of the insura angularis ◦ Pyloric antrum: this extend from the insura angularis to the pylorus. ◦ Pylorus: a tubular part with thick muscular form called pyloric sphincter. The cavity of the pylorus is the pyloric canal. Stomach – Blood supply Blood supply: Arteries. Main arterial source is the celiac trunk of abdominal aorta. The right gastric artery arise from the hepatic artery of celiac trunk to supply the lesser curvature of the stomach. The left gastric artery arise from the celiac trunk and supply superior part of the stomach. The short gastric artery arises from the splenic artery and supply the fundus of the stomach. The right gastroepiploic (gastro-omental) artery arise from the gastroduodenal branch of hepatic artery and supply the lower part of the greater curveture. The left gastroepiploic (gastro-omental) artery arise from the spleenic artery and supply the upper part of the greater curveture Veins: The veins drain into the portal circulation ◦ The left and right gastric veins drain directly into the portal vein. ◦ The short gastric vein and the left gastroepiploic vein join the splenic vein. ◦ The right gastroepiploic vein join the superior mesenteric vein. Lymphatic drainage: ◦ The lymph vessels follow the artery into the right and left gastric nodes, the left and right gastroepiploic nodes and the short gastric nodes. ◦ All lymph from the stomach passes to the celiac nodes located around the root of celiac trunk on the posterior abd. Wall. Nerve supply: The sympathetic fibres from the celiac plexus and parasympathetic fibres from the right and left vagus nerves. ◦ The anterior vagal trunk mainly from the left vagus nerve supply the anterior surface of the stomach and the pyrolus. It also carries nerve fibres for pain transmission. ◦ The posterior vagal trunk mainly from the right vagus nerve supply the posterior surface of the stomach. It also carries secretomotor nerve fibres to gastric glands and gastric wall muscles. Functions of the stomach: 1. Digestion-. The stomach releases proteases (proteindigesting enzymes such as pepsin) and hydrochloric acid, which kills or inhibits bacteria and provides the acidic pH of two for the proteases to work. Food is churned by the stomach through peristalsis –the boluses are converted into chyme (partially digested food). Chyme which enters the duodenum to begin extraction of nutrients. Depending on the quantity and contents of the meal, the stomach will digest the food into chyme anywhere between forty minutes and a few hours. The average human stomach can comfortably hold about a litre of food. Gastric juice in the stomach also contains inactive pepsinogen which is activated by Hydrochloric acid to the active form pepsin, that breaks down proteins into polypeptides. 2.Absorption Although the absorption is mainly a function of the small intestine, some small are absorbed through stomach lining. This includes: Water, if the body is dehydrated Medication, like aspirin Amino acids 10–20% of ingested ethanol (e.g. from alcoholic beverages) ◦ Caffeine ◦ Water-soluble vitamins ◦ The parietal cells of the stomach are responsible for producing intrinsic factor, which is necessary for the absorption of vitamin B12. B12 is used in cellular metabolism and is necessary for the production of red blood cells, and the functioning of the nervous system. ◦ ◦ ◦ ◦ 3. Control of secretion and motility The movement and the flow of chemicals into the stomach are controlled by both the autonomic nervous system and by the various digestive system hormones: The hormone gastrin for secretion of HCl from the parietal cells, and pepsinogen from chief cells in the stomach. Gastrin released by G cells in the stomach also causes increased motility and distension of the antrum. 4. Temporaly storage The stomach pushes food into the small intestine only when the intestine is not busy. While the intestine is full and still digesting food, the stomach acts as storage for food. 5. Stomach as nutrition sensor The stomach can "taste" sodium glutamate using glutamate receptors and this information is passed to the lateral hypothalamus and limbic system in the brain as a palatability signal through the vagus nerve. The stomach can also sense, independently to tongue and oral taste receptors, glucose, carbohydrates, proteins, and fats. This allows the brain to link nutritional value of foods to their tastes. The small intestine or small bowel is the longest part of the GIT extending between the pylorus the stomach and the ileocaecal junction, and is where most of the digestion and absorption of food takes place. Structure: The small intestine has three distinct regions – the duodenum, jejunum, and ileum. The average length of the small intestine in an adult human male is 6.9 m (22 ft 8 in), and 7.2 m (23 ft 6 in) in an adult female. [It can vary greatly, from as short as 4.6 m (15 ft) to as long as 9.8 m (32 ft).Recent studies indicate that small intestine may be shorter, around 3.5 m (11 ft 6 in), and that the length is less affected by age after childhood than expected] It is approximately 2.5–3 cm in diameter. The surface area of the human small intestinal mucosa averages 30 square meters Fig: The duodenum is a short structure (about 20– 25 cm (8 – 10 in) long continuous with the stomach It is shaped like a "C". It surrounds the head of the pancreas and fixed to the posterior abdominal wall. The duodenum contains Brunner's glands, which produce a mucus-rich alkaline secretion containing bicarbonate. These secretions, in combination with bicarbonate from the pancreas, neutralizes the stomach acids contained in gastric chyme. The duodenum consists of four parts ◦ 1st part is 5cm(2in) long, runs upwards and backwards from the pylorus to the right side of the 1st lumbar vert. Fig: The section of small intestine - Duodenum 2nd part is 8cm(3in) long, runs vertically downwards anteriorto the hilum of the right kidney and the 2nd – 3rd lumbar vert. The main pancreatic duct opens into it this part. 3rd part is 8cm(3in) long, runs holizontally to the left on the subcostal plane following the lower margin of the pancreas. 4th part is 5cm(2in) long, runs upwards and to the left to the duodenojejunal flexure. The flexure is held in its position by the ligament of treitz which is attached to the right crus of the diaphragm. Blood supply: The upper half by the superior pancreaticoduodenal branch from the gastroduodenal artery. The lower half by inferior pancreaticoduodenal branch of superior mesenteric artery. Veins: superior pancreaticoduodenal to the portal vein and the inferior pancreaticoduodenal to the superior mesenteric vein. Lymph drainage: lymph vessel follow the arteries and drain upwards via pancreaticoduodenal nodes to gastroduodenal nodes to the celiac trunk. Nerve supply: sympathetic and parasympathetic (vagal) from celiac and superior mesenteric plexus. Jejunum and Ileum: These measures 6m (20ft), jejunum 2.4m (7.9ft), ileum 3.6m (12.1ft). Jejunum is the upper 2/5 of the total freely mobile length extending from the duodenojejunal frecture to the ileocecal junction. The two parts are in living distinguished by 1. The jejunum lie coiled in the upper part of pertoneal cavity below the left side of the transverse mesocolon while the ileum occupy the lower part of the cavity and in the pelvis. 2. The jejunum is wider bored, thicker walled and redder than the ileum 3. The jejunal mesentery is attached on the posterior abdominal wall above and to the left of abd. Aorta, while the ileal attaches below and right side of the aorta. 4. the jejunal mesenteric vessels form one or two arcades with long and infrequent branching passing to the intestinal wall. Ileum receives numerous short terminal vessels arising from series of three or four or more arcades. 5. Jejunal fat deposits at the root of mesentery and scant near the intestial wall, ileal fats deposit throughout that it extend from the root to the intestinal wall. 6. In the living, payer’s patch seen in the lower part of the wall of the ileum. Fig: An arcade of small intestine Blood supply: from the superior mesenteric artery and the ileocecal artery of the lower part of the ileum. Veins correspond to the artery and drain into the superior mesenteric vein. Lymphatic drainage to the superior mesenteric nodes situated around the origin of the superior mesenteric artery. Nerve supply: sympathetic and parasympathetic (vagal) from superior mesenteric plexus Functions 1. Digestion The small intestine is where most chemical digestion takes place. ◦ Many of the digestive enzymes that act in the small intestine are secreted by the pancreas and liver and enter the small intestine via the pancreatic duct. ◦ Pancreatic enzymes and bile from the gallbladder enter the small intestine in response to the hormone cholecystokinin, which is produced in the small intestine in response to the presence of nutrients. ◦ Secretin, another hormone produced in the small intestine, causes additional effects on the pancreas, where it promotes the release of bicarbonate into the duodenum in order to neutralize the potentially harmful acid coming from the stomach. ◦ The three major classes of nutrients that undergo digestion are proteins, lipids (fats) and carbohydrates: 2. Absorption Digested food is now able to pass into the blood vessels in the wall of the intestine through either diffusion or active transport. The small intestine is the site where most of the nutrients from ingested food are absorbed. The functions of the plicae circulares, the villi, and the microvilli are to increase the amount of surface area available for the absorption of nutrients, and to limit the loss of said nutrients to intestinal fauna. Each villus has a network of capillaries and fine lymphatic vessels called lacteals close to its surface. The epithelial cells of the villi transport nutrients from the lumen of the intestine into these capillaries (amino acids and carbohydrates) and lacteals (lipids). The material that remains undigested and unabsorbed passes into the large intestine. Absorption of the majority of nutrients takes place in the jejunum, with the following notable exceptions: ◦ Iron is absorbed in the duodenum. ◦ Vitamin B12 and bile salts are absorbed in the terminal ileum. ◦ Water and lipids are absorbed by passive diffusion throughout the small intestine. ◦ Sodium bicarbonate is absorbed by active transport and glucose and amino acid co-transport. ◦ Fructose is absorbed by facilitated diffusion 3. Immunological The small intestine supports the body's immune system. ◦ The presence of probiotic gut flora appear to contribute positively to the host's immune system. ◦ Peyer's patches, located within the ileum of the small intestine are an important part of the digestive tract's local immune system. The large intestine, also called the colon or the large bowel, is the last part of the digestive system in vertebrates. Water is absorbed here and the remaining waste material is stored as feces before being removed by defecation. It is the combination of the cecum, colon proper, rectum and anal canal. In humans, it begins in the right iliac region of the pelvis, just at or below the waist, where it is joined to the end of the small intestine It then continues up the abdomen, across the width of the abdominal cavity, and then down to its endpoint at the anus. Overall, in humans, the large intestine is about 1.55 metres (4.9 ft) long, which is about one-fifth of the whole length of the gastrointestinal tract. The length of the adult human colon is, on average, for women 155 cm (61in) range of 80 to 214 cm (31.5 – 84) and for men 166 cm (65in) range of 80 to 313 cm (31.5 – 123in). The colon is the last part of the digestive system in most vertebrates. ◦ It extracts water and salt from solid wastes before they are eliminated from the body ◦ is the site in which flora-aided (largely bacterial) fermentation of unabsorbed material occurs. ◦ About 1.5 litres or 45 ounces of water arrives in the colon each day. The parts of the large intestine are either intraperitoneal or behind it – retroperitoneum which have no a complete covering of peritoneum, so they are fixed in location. Sections of the large intestine are: The cecum and the appendix ◦ The cecum is the first section of the colon and involved in the digestion ◦ the appendix which develops embryologically from it, is a vestigial organ and has a high concentration of lymphatic cells. Is not involved in digestion but is part of the gut-associated lymphoid tissue. Also the appendix has a role in housing a sample of the colon's microflora, and is able to help to repopulate the colon with bacteria if the microflora Fig: Large intestine. The ascending colon: ◦ The ascending colon is one part of four sections of the large intestine. It runs through the abdominal cavity, upwards toward the transverse colon for approximately eight inches (20 cm). ◦ Its main functions of the colon is to remove the water and other key nutrients from waste material and recycle it back into the body The transverse colon: ◦ is the part of the colon from the hepatic colic flexure to the splenic flexure. ◦ It hangs off the stomach, attached to it by a large fold of peritoneum called the greater omentum ◦ It is connected to the posterior abdominal wall by a mesentery known as the transverse mesocolon It functions as to concentrate materials in large intestine as the contents become more solid (water is removed) in order to form feces. Blood supply is from middle colic artery [a branch of the superior mesenteric artery (SMA)] to its proximal two-thirds while the latter third is supplied by branches of the inferior mesenteric artery (IMA). The "watershed" area between these two blood supplies, which represents the embryologic division between the midgut and hindgut, is an area sensitive to ischemia. The descending colon: The descending colon is the part of the colon from the splenic flexure to the beginning of the sigmoid colon. It is retroperitoneal in two-thirds of humans with a (usually short) mesentery. One function of the descending colon in the digestive system is to store faeces that will be emptied into the rectum. Blood supply: The arterial supply comes via the left colic and sigmoid branches of the inferior mesenteric artery. Veins follow artery and drain into the inferior mesenteriv vein Nerve supply: sympathetic and parasympathetic pelvic splachnic nerve through the inferior mesenteric plexus. The sigmoid colon – the v-shaped region of the large intestine. Is the part of the large intestine after the descending colon and before the rectum. The walls of the sigmoid colon are muscular, and contract to increase the pressure inside the colon, causing the stool to move into the rectum. Blood supply: supplied with blood from several branches (usually between 2 and 6) of the sigmoid arteries, a branch of the IMA. The IMA terminates as the superior rectal artery. Rectum is the last section of the colon. ( ref to perineum) Additional appearances: ◦ Taeniae coli – three bands of smooth muscle, run the length of the large intestine ◦ Haustra – bulges caused by contraction of taeniae coli, Because the taenia coli are shorter than the large bowel itself, the colon becomes sacculated, forming the haustra of the colon which are the shelf-like intraluminal projections. ◦ Epiploic appendages – small fat accumulations or tabs on the viscera.