* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PDF
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Dr Pravina Koteshwar, ICRI
Introduction to Cardiovascular System
Introduction
The heart and circulatory system (also called the cardiovascular system) make up the network that
delivers blood to the body's tissues. With each heartbeat, blood is sent throughout our bodies,
carrying oxygen and nutrients to all of the cells in the body.
Basic Components:
•
Structure and organization of blood vessels
•
Structure of the heart ; cardiac cycle and physiology
•
Circulatory system.
•
Blood and components
•
Cardiac diseases and their management
Structure and organization of blood vessels
Every day, the approximately 10 pints (5 liters) of blood in adult human body travel many times
through about 60,000 miles (96,560 kilometers) of blood vessels that branch and cross, linking the
cells of our organs and body parts. From the hard-working heart, to our thickest arteries, to capillaries
so thin that they can only be seen through a microscope, the cardiovascular system is our body's
lifeline.
heart→
→arteries →arterioles
↑
↓
veins←
←venules ←capillaries
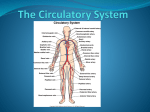
The circulatory system is composed of the heart and blood vessels, including arteries, veins, and
capillaries. Our bodies actually have two circulatory systems: The pulmonary circulation is a short
loop from the heart to the lungs and back again, and the systemic circulation (the system we
usually think of as our circulatory system) sends blood from the heart to all the other parts of our
bodies and back again.
The circulatory system is composed of the heart and blood vessels, including arteries, veins, and
capillaries. Our bodies actually have two circulatory systems: The pulmonary circulation is a short
loop from the heart to the lungs and back again, and the systemic circulation (the system we
CVS Introduction
Page 1
Dr Pravina Koteshwar, ICRI
usually think of as our circulatory system) sends blood from the heart to all the other parts of our
bodies and back again.
Functions of CVS:
1. Transportation (nutrients, gases, hormones, wastes, etc.)
2. Acid-base regulation
3. Thermoregulation
4. Immunity Vs pathogens and toxins
5. Hemostasis (restriction of fluid losses at the site of injury
The Role of Blood Vessels
Blood vessels carrying blood away from the heart are called arteries. They are the thickest blood
vessels, with muscular walls that contract to keep the blood moving away from the heart and through
the body. In the systemic circulation, oxygen-rich blood is pumped from the heart into the aorta. This
greater artery curves up and back from the left ventricle, then heads down in front of the spinal
column into the abdomen. Two coronary arteries branch off at the beginning of the aorta and divide
into a network of smaller arteries that provide oxygen and nourishment to the muscles of the heart.
Unlike the aorta, the body's other main artery, the pulmonary artery, carries oxygen-poor blood.
From the right ventricle, the pulmonary artery divides into right and left branches, on the way to the
lungs where blood picks up oxygen.
CVS Introduction
Page 2
Dr Pravina Koteshwar, ICRI
Arterial walls have three layers:
•
The endothelium is on the inside and provides a smooth lining for blood to flow over as it
moves through the artery. Endothelium- prevents platelet aggregation secretes substances
that control diameter of blood vessel
•
The media is the middle part of the artery, made up of a layer of muscle and elastic tissue.
The middle layer of an artery wall consists of smooth muscle that can constrict to regulate
blood flow and blood pressure
•
The adventitia is the tough covering that protects the outside of the artery.
As they get farther from the heart, the arteries branch out into arterioles which are smaller and less
flexible. Arterioles can constrict or dilate, changing blood pressure.
Blood vessels that carry blood back to the heart are called veins. They are not as muscular as
arteries, but they contain valves that prevent blood from flowing backward. Veins have the same three
layers that arteries do, but they are thinner and less flexible. The two largest veins are the superior
and inferior vena cavae.
Venules are continuous with capillaries; take in some returned fluid (rest is retained by tissues
or returned to blood via lymphatic
system)
Veins have thinner walls; less muscle; but can hold much more blood
Many veins in limbs have valves to prevent backflow (Varicose veins arise when pressure on
valves is prolonged)
CVS Introduction
Page 3
Dr Pravina Koteshwar, ICRI
A network of tiny capillaries connects the arteries and veins. Even though they're tiny, the capillaries
are one of the most important parts of the circulatory system because it is through them that
nutrients and oxygen are delivered to the cells. In addition, waste products such as carbon dioxide are
also removed by the capillaries. In capillaries, oxygen and nutrients move out by diffusion; CO2 in (via
lipid membrane, channels, etc.)
The Heart
The heart is the key organ in the circulatory system. As a hollow, muscular pump, its main function is
to propel blood throughout the body. It usually beats from 60 to 100 times per minute, but can go
much faster when it needs to. It beats about 100,000 times a day. The approximate size of heart is:
11cm long, 7cm wide, weighting leass than 500 g.
3 Layers f heart:
–
Epicardium: thin, lubricated outermost layer
–
Myocardium: thickest layer containing cardiac muscle tissue: contracts to eject blood
from ventricles of heart
–
Endocardium: innermost layer that lines the entire circulatory system; protective
inner lining of chambers and valves
•
The pericardium is the outer membranous sac with lubricating fluid.
The heart has four chambers that are enclosed by thick, muscular walls. It lies between the lungs and
just to the left of the middle of the chest cavity. The bottom part of the heart is divided into two
CVS Introduction
Page 4
Dr Pravina Koteshwar, ICRI
chambers called the right and left ventricles, which pump blood out of the heart. A wall called the
interventricular septum divides the ventricles.
The upper part of the heart is made up of the other two chambers of the heart, called the right and
left atria. The right and left atria receive the blood entering the heart. A wall called the interatrial
septum divides the atria, and they're separated from the ventricles by the atrioventricular valves.
The tricuspid valve separates the right atrium from the right ventricle, and the mitral valve
separates the left atrium and the left ventricle.
Semilunar heart valves separate the ventricles and the large blood vessels that carry blood leaving the
heart. These valves are called the pulmonic valve, which separates the right ventricle from the
pulmonary artery leading to the lungs, and the aortic valve, which separates the left ventricle from
the aorta.
Cardiac Cycle
A healthy heart makes a "lub-dub" sound with each beat. One complete heartbeat makes up a
cardiac cycle, which consists of two phases. In the first phase, the ventricles contract (this is called
systole, sending blood into the pulmonary and systemic circulation. To prevent the flow of blood
backwards into the atria during systole, the atrioventricular valves close, creating the first ("lub")
sound.
When the ventricles finish contracting, the aortic and pulmonic semilunar valves close to prevent blood
from flowing back into the ventricles. This is what creates the second sound (the "dub"). Then the
ventricles relax. This is called diastole and fills with blood from the atria, which makes up the second
phase of the cardiac cycle.
CVS Introduction
Page 5
Dr Pravina Koteshwar, ICRI
Passage of blood through the heart
Blood follows this sequence through the heart: superior and inferior vena cava → right atrium →
tricuspid valve → right ventricle → pulmonary semilunar valve → pulmonary trunk and arteries to the
lungs → pulmonary veins leaving the lungs → left atrium → bicuspid valve → left ventricle → aortic
semilunar valve → aorta → to the body.
Blood from the head and arms returns to the heart through the superior vena cava, and blood from
the lower parts of the body returns through the inferior vena cava. Both vena cavae deliver this
oxygen-depleted blood into the right atrium. From here the blood exits to fill the right ventricle, ready
to be pumped into the pulmonary circulation for more oxygen.
In the pulmonary circulation, blood low in oxygen but high in carbon dioxide is pumped out the right
ventricle into the pulmonary artery, which branches off in two directions. The right branch goes to the
right lung, and vice versa. In the lungs, the branches divide further into capillaries. Blood flows more
slowly through these tiny vessels, allowing time for gases to be exchanged between the capillary walls
and the millions of alveoli, the tiny air sacs in the lung.
During the process called oxygenation, oxygen is taken up by the bloodstream. Oxygen locks onto a
molecule called hemoglobin in the red blood cells. The newly oxygenated blood leaves the lungs
through the pulmonary veins and heads back to the heart. It enters the heart in the left atrium, then
fills the left ventricle so it can be pumped into the systemic circulation
Blood supply to the heart
Right and left coronary arteries stem from aorta; branch into smaller vessels. Cardiac veins deliver
blood to coronary sinus and back to the right atrium.
CVS Introduction
Page 6
Dr Pravina Koteshwar, ICRI
Conduction system of the Heart:
Intrinsic control mechanisms
A unique electrical system in the heart causes it to beat in its regular rhythm.
The sinoatrial node (SA node), a small area of tissue in the wall of the right atrium, sends
out an electrical signal to start the contracting of the heart muscle. These electrical impulses
cause the depolarization of atria and lead to their contraction first (the right atrium contracts
slightly before the left atrium);
At that time AV valves open and ventricles fill with blood.
The cardiac impulse then travel down to the atrioventricular or AV node, which acts as a
kind of relay station. It helps in complete filling up of ventricles.
From here the electrical signal travels through the right and left ventricles via Bundle of His
of interventricular septum, and then via Purkinje system causing the ventricles to contract
and force blood out into the major arteries.
Ventricles contract and ventricular pressure exceeds atrial pressure: the AV valves close- atria
relaxes and refills with blood
When ventricular pressure exceeds pressure in pulmonary artery and aorta, the pulmonic and
aortic valves open, and blood is pumped into the pulmonary and systemic circulations,
respectively.
As the ventricles begin to relax after systole, the pulmonic and aortic valves close and diastole
begins.
Nerve supply to the heart: Extrinsic Control of Heart
•
A cardiac control center in the medulla oblongata speeds up or slows down the heart rate by
way of the autonomic nervous system branches: parasympathetic system slows heart rate &
CVS Introduction
Page 7
Dr Pravina Koteshwar, ICRI
sympathetic system increases heart rate.
•
Hormones epinephrine and norepinephrine from the adrenal medulla also stimulate heart rate.
•
Sympathetic nervous system through celiac plexus to heart secretes norepinephrine increases
force of contractions
•
Normally both sympathetic and parasympathetic function at a steady background level
•
Cardiac control center in medulla oblongata maintains balance between the two
•
Baroreceptors detect changes in blood pressure. Rising pressure stretches receptors
•
Increase in temperature increases heart rate
•
Ions and heart rate: HR is decreased by excess potassium ; excess calcium increases HR
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a recording of the electrical changes that occur in the myocardium
during a cardiac cycle.
Atrial depolarization creates the P wave, ventricle depolarization creates the QRS wave, and
repolarization of the ventricles produces the T wave.
Blood Pressure
•
The beating of the heart is necessary to homeostasis because it creates pressure that propels
blood in arteries and the arterioles.
•
Arterioles lead to the capillaries where nutrient and gas exchange with tissue fluid takes place.
•
The pumping of the heart sends out blood under pressure to the arteries.
•
Blood pressure is greatest in the aorta; the wall of the left ventricle is thicker than that of the
right ventricle and pumps blood to the entire body. Blood pressure then decreases as the
cross-sectional area of arteries and then arterioles increases.
•
Blood pressure due to the pumping of the heart accounts for the flow of blood in the arteries.
•
Systolic pressure is high when the heart expels the blood.
•
Diastolic pressure occurs when the heart ventricles are relaxing.
CVS Introduction
Page 8
Dr Pravina Koteshwar, ICRI
•
Both pressures decrease with distance from the left ventricle because blood enters more and
more arterioles and arteries.
The measurement blood pressure without further specification usually refers to the systemic
arterial pressure measured at a person's upper arm. It is measured on the inside of an elbow at
the brachial artery, which is the upper arm's major blood vessel that carries blood away from the
heart. A person's BP is usually expressed in terms of the systolic pressure over diastolic pressure
for example 120/80 mmHg.
Cardiodynamics and Cardiac Output
Cardiodynamics: study of movements and forces generated during cardiac contractions
Important Terms:
–End-diastolic volume (EDV): blood amount in each ventricle at end of ventricular diastole
–End-systolic volume (ESV): blood amount in each ventricle at end of ventricular systole
–Stroke Volume (SV): blood amount pumped from each ventricle during a single beat:
SV= EDV- ESV
–Ejection fraction (EF): % EDV represented by SV: EF= SV/ EDV
Preload: degree of stretching by ventricular muscle cells during ventricular diastole
•
Directly proportional to EDV
•
Affects heart rate
Afterload: amount of tension contracting ventricle must produce to eject blood
Directly proportional to ESV
Inversely proportional to stroke volume
Cardiac Output (CO):
CO determines the amount of blood pumped by each ventricle in one minute, measured as ml/ min
•
Blood Pressure (BP): cardiac output × peripheral vascular resistance (PVR):
BP = CO × PVR
*****
CVS Introduction
Page 9