* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download IN THIS ISSUE Precursor loss triggers AIDS A MyD88 meddles with
Immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
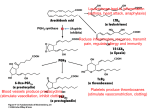
Published August 20, 2007 IN THIS ISSUE Precursor loss triggers AIDS A MyD88 meddles with survival In the MyD88 family of cytosolic adaptor proteins, the newest member is the group’s black sheep, according to Kim et al. (page 2063). Whereas most MyD88 proteins turn on antipathogen responses within myeloid cells, the rebel, MyD88-5, instigates cell death within neurons. MyD88-1–4 all respond to Toll-like receptor (TLR) activation in leukocytes and stimulate innate immune responses. MyD88-5, however, does not transmit TLR signals or induce innate response genes. Two extra domains in MyD88-5 that may allow it to interact with cytoskeletal proteins hint at an entirely different function. Kim et al. now find that the protein is not even expressed in most leukocytes and instead is found mainly in neurons. There, MyD88-5 bound to microtubules and studded the outer 2010 membranes of mitochondria. Mitochondria formed clusters when MyD88-5 expression levels were high but were unable to group when the two protein interaction domains of MyD88-5 were removed. By linking them to the microtubules, MyD88-5 probably enables the mitochondria to get around efficiently within the neuron, where these energy stores must travel long distances. But how MyD88-5 levels are controlled within the neuron remains to be determined. MyD88-5 also recruited JNK3, a kinase whose association with mitochondria activates apoptosis in stressed cells. The stress of UV light increased the association of JNK3 with MyD88-5, and neurons from mice lacking MyD88-5 were less vulnerable to stress-induced apoptosis. The authors are now using mouse models of brain injury to investi- Proapoptotic JNK3 (yellow) clusters near mitochondria (red) only when MyD88-5 (green) is present. gate whether the absence of MyD88-5 saves damaged neurons during, for example, a stroke. T cells also expressed some MyD88-5. Because these cells lack JNK3, the adaptor probably has additional binding partners. JEM Vol. 204, No. 9, 2007 Downloaded from on June 12, 2017 HIV and its simian counterpart, SIV, replicate rapidly after infection but often take many years to subdue the immune system and cause AIDS. Okoye et al. (page 2171) now find that these slow burner viruses only cause disease after they deplete the precursor cells that give rise to pathogen-fighting effector cells. The effector memory T (TEM) cells that battle these viruses at infection sites develop from a pool of CD4+ central memory (TCM) cells that are stored in secondary lymphoid organs. Although the virus infects both types of cells simultaneously, TEM cells are the first casualties. This early depletion of TEM cells is not completely devastating; the TCM population quickly cranks out more TEM cells. But this defensive strategy is obviously not foolproof: infected individuals eventually develop AIDS. Okoye et al. now identify the glitch in the strategy by tracking disease progression in SIV-infected rhesus macaques. Newly generated TEM cells were short lived, they found, as persistent activation by the virus induced their death. And unlike in earlier stages of infection, TCM cells no longer came to the rescue, Loss of TCM cells during chronic SIV infection (bottom) as they were also crippled by viral infection. The virus thus tamed the immune depletes pathogen-fighting TEM cells and triggers AIDS. system by stimulating one population to death and destroying its back-up. Based on these results, stabilizing the TCM pool may be a more effective way to prevent the onset of AIDS than controlling viral load—the goal of current vaccination strategies. Rising viral loads might not be the trigger for AIDS, as viral loads remained constant while CD4+ T cell levels declined during the later stages of disease. Recent studies from other groups show that survival of patients with AIDS correlates with more circulating TCM cells, supporting the idea that protecting the TCM niche might keep AIDS at bay. The team is now trying to identify the factors that bolster TCM cell levels and how HIV/SIV dismantles them. Published August 20, 2007 Text by Hema Bashyam [email protected] T-bet terminates self-renewal The transcription factor T-bet is expressed mainly in TEM cells. A T cell transcription factor favors short-term benefits over long-term stability, according to a new study by Intlekofer et al. (page 2015). Long-term protection against pathogens by CD8+ T cells is due to a self-renewing population of central memory (TCM) cells that circulate in the lymph nodes. When they see their target antigen, these cells first rapidly proliferate, become cytotoxic, and then head out to the periphery to fight the invaders. A faster attack mode is provided by effector memory T (TEM) cells, which are already in the periphery, but these cells quickly die out. Memory T cell development requires a transcription factor called T-bet. Intlekofer et al. now find that mice lacking T-bet have plenty of TCM cells but lack the TEM pool. In normal mice, only the TEM cells expressed T-bet, suggesting that T-bet skews the balance between the two populations by driving the differentiation of activated CD8+ T cells into TEM cells. CD8+ memory T cell development also requires signals from CD4+ T cells. The team found that these signals favored the growth of CD8+ TCM cells. Mice that lacked CD4+ T cells therefore had higher numbers of TEM cells than TCM cells. This expanded TEM population had high levels of T-bet protein. Deletion of T-bet corrected this defect by restoring the numbers of self-renewing cells. T cell education dictates function On page 2053, Ghosh et al. reveal how antiinflammatory COX-2 inhibitors cause dangerous cardiac side effects. COX-2, they find, is needed to shut off an important clotting protein. COX-2 is produced during infection and injury by the endothelial cells that line blood vessels. The enzyme converts a cellular lipid known as arachidonic acid into lipids that instigate fever, pain, and other uncomfortable hallmarks of inflammation. COX-2 inhibitors such as Vioxx were popular antiinflammatory drugs until some users began to suffer serious side effects such as heart attack and stroke. Ghosh et al. now find that the normally cardioprotective effect of COX-2 stems from its metabolic conversion not of arachidonic acid, but of other substrates: the endocannabinoids. Byproducts of these lipids, they found, activated a nuclear receptor and transcription factor, PPARδ, that suppressed the gene for tissue factor (TF)— a protein that activates blood clotting. Mice that were given COX-2 inhibitors had high levels of TF that could then be decreased by activating PPARδ. The side effects triggered by the COX-2 inhibitors in humans may thus be due to the overproduction of TF. COX-2’s anticlotting role probably keeps injured vessels free of clots while the damage is being repaired. The team is now investigating whether patients who have adverse reactions to the drugs have defects in TF or other clotting genes. How a young T cell is educated may dictate its future function, according to a new report by Li et al. (page 2145). Young T cells receive survival signals through their T cell receptors during development. These signals are normally provided by epithelial cells in the thymus. But recent reports show that CD4+ thymocytes also signal to each other. When stimulated by antigen, epithelium-educated CD4+ thymocytes can become helper T cells of all varieties—T helper (Th)-1, Th2, or Th17 cells— depending largely on the surrounding cytokines. But self-educated thymocytes, Li et al. now find, fail to make this lineage choice. These cells rapidly generated both interferon (IFN)-γ and interleukin (IL)-4, even when stimulated under conditions that normally inhibit IL-4 production. A ready-to-fire IL-4 locus and preformed IL-4 mRNA in the developing cells explained their tendency to continue synthesizing IL-4. Mice whose thymocytes were forced to signal to each other to survive were less likely to develop allergic inflammation than were mice whose T cells developed normally. This protective effect might be due, the authors speculate, to the suppression of pro-allergic IL-4 by the IFNγ produced by these cells. Thus, people who have more self-educated T cells may be less allergy prone. But assessing the relative numbers of the two cell types in humans is difficult, as distinguishing surface markers have yet to be identified. The team is now investigating how T cells decide between a thymocyte- and an epithelial cell–based education and how thymocyte-to-thymocyte signals set the cells up for an IL-4–producing future. A COX-2 inhibitor (right) increases the expression of tissue factor (red) in heart vessels (arrows). IN THIS ISSUE | The Journal of Experimental Medicine 2011 Downloaded from on June 12, 2017 Following the trail from COX-2 to clotting