* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Transforming growth factor-β and myostatin signaling in skeletal
Survey
Document related concepts
Transcript
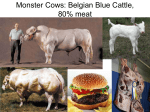
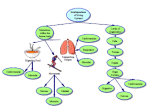
J Appl Physiol 104: 579–587, 2008; doi:10.1152/japplphysiol.01091.2007. Invited Review Transforming growth factor- and myostatin signaling in skeletal muscle Helen D. Kollias1 and John C. McDermott2 1 Department of Neurology, Johns Hopkins Hospital, Baltimore, Maryland; and 2Department of Biology, York University, Toronto, Ontario, Canada myogenesis; Smad; MyoD SKELETAL MUSCLE has a remarkable morphogenic ability to regenerate and adapt to environmental stimuli. Fundamentally, skeletal muscle regeneration is the recapitulation of skeletal muscle development in a postnatal context. Thus an understanding of the regulation of development and regeneration are mutually reinforcing. Both regeneration and development of skeletal muscle are profoundly sensitive to the extracellular milieu. In particular, signal transduction pathways initiated by growth factors such as insulin-like growth factor (IGF-1), fibroblast growth factor (FGF), and transforming growth factor- (TGF-) exert a potent level of control over muscle gene expression. The role of the TGF- superfamily of growth factors is of considerable interest since many facets of muscle ontogeny and physiology are regulated by some of the ligands belonging to this cytokine superfamily. In particular, myostatin is of growing interest since it has been shown to exert profound effects on muscularity in mice, cattle, and humans (see Fig. 1; Refs. 52, 54, 68), as well as other animals. TGF- superfamily signaling relies on a relatively parsimonious canonical pathway that interdigitates with particular aspects of the host cell machinery through cell-specific protein:protein interactions that allow precise cell context-dependent responses to the ligand. This review will focus on salient aspects of TGF- superfamily signaling that pertain specifically to skeletal muscle. Information from a variety of studies offering insights into the molecular events of TGF- signal transduction, the function of TGF- in cultured muscle cells, and the effects of TGF- in postnatal skeletal muscle physiology, will provide the foundation of this review. Address for reprint requests and other correspondence: J. McDermott, 327 Farquharson, 4700 Keele St., Toronto, Ontario, Canada M3J 1P3 (e-mail: [email protected]). http://www. jap.org AN OVERVIEW OF TGF- SIGNALING TGF-1 ligand is recognized as the prototype of a class of multifunctional growth factors that regulate key events of metazoan development, disease, and repair (44, 45). In 1981, TGF- effects were first reported by Roberts and colleagues (65), who found that TGF- induced rat kidney fibroblasts to proliferate. Since then, TGF- has been found to have a plethora of effects, such as regulation of cell growth, proliferation, differentiation, adhesion, migration, and apoptosis (reviewed in Refs. 44, 46, 48). These effects are highly complex and sometimes difficult to reconcile; however, one unifying feature of TGF- signaling is that its effects are profoundly dependent on the cell context. For example, TGF- causes increased proliferation in fibroblasts (65) but inhibits proliferation in epithelial cells, causes differentiation of neuronal cells, but blocks differentiation in mesenchymal cells (2, 18, 19, 66, 73). In skeletal muscle, TGF- superfamily members have been shown to have potent effects on both muscle development and postnatal skeletal muscle mass. The TGF- superfamily consists of over 50 structurally related ligands, many of which fall into three major subfamilies: TGF-, bone morphogenic protein (BMP), and activin (reviewed in Ref. 17). Exhaustive work on the molecular characterization of the TGF- signal transduction pathway has led to the delineation of a canonical signaling pathway for all TGF- superfamily members consisting of three main components (74): 1) the ligand; 2) the receptors (serine/threonine kinases); and 3) the intracellular mediators (Smads; see Fig. 2). For the TGF-, Activin, and BMP subfamilies signal transduction begins with the ligand binding to its type II receptor. The type II receptor associates with its corresponding type I receptor, forming an activated heterotetrameric receptor complex, which transphosphorylates the type I receptor activating the latent kinase activity of the receptor complex. The activated 8750-7587/08 $8.00 Copyright © 2008 the American Physiological Society 579 Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 Kollias HD, McDermott JC. Transforming growth factor- and myostatin signaling in skeletal muscle. J Appl Physiol 104: 579 –587, 2008; doi:10.1152/japplphysiol.01091.2007.—The superfamily of transforming growth factor- (TGF-) cytokines has been shown to have profound effects on cellular proliferation, differentiation, and growth. Recently, there have been major advances in our understanding of the signaling pathway(s) conveying TGF- signals to the nucleus to ultimately control gene expression. One tissue that is potently influenced by TGF- superfamily signaling is skeletal muscle. Skeletal muscle ontogeny and postnatal physiology have proven to be exquisitely sensitive to the TGF- superfamily cytokine milieu in various animal systems from mice to humans. Recently, major strides have been made in understanding the role of TGF- and its closely related family member, myostatin, in these processes. In this overview, we will review recent advances in our understanding of the TGF- and myostatin signaling pathways and, in particular, focus on the implications of this signaling pathway for skeletal muscle development, physiology, and pathology. Invited Review 580 TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE Fig. 1. Phenotype of mysotatin null vertebrates.A: upper forelimb muscles of wild-type mouse; B: upper forelimb of mouse that is myostatin null (52); C: bovine with myostatin mutation (54); D and E: human with myostatin mutation as a neonate (D) and at 7 mo of age (E; Ref. 68). Copyright permissions: copyright 1997 National Academy of Sciences USA (A and B); reprinted with permission from Macmillan Publishers (C): Nature; copyright 1997 (D) and 2004 (E) Massachusetts Medical Society. All rights reserved. SKELETAL MUSCLE DEVELOPMENT AND REGENERATION Briefly, skeletal muscle ontogeny is comprised of three developmental stages: 1) determination, 2) differentiation, and 3) maturation (Fig. 3). Determination begins with the aggre- gation of mesodermal precursors in the paraxial region of the embryo, which form somites. The somites are composed of pluripotent cells, of which some will become muscle progenitor cells (33). These myogenic progenitor cells give rise to proliferating cells that are committed to the myogenic lineage termed myoblasts and are derived from the myotome compartment of the somite (33). Proliferating myoblasts subsequently undergo differentiation, a process that includes withdrawal from the cell cycle, expression of muscle-specific genes, and fusion resulting in the formation of multinucleated myotubes. Myotubes eventually give rise to the vast array of muscle fibers that are used to construct the complex skeletal muscle architecture of the animal. There are two types of myoblasts, embryonic and fetal. Most embryonic myoblasts differentiate Fig. 2. Overview of the canonical transforming growth factor (TGF)- pathway. The TGF superfamily member (ligand) binds to the type II and type I receptors. The type II receptor then transphosphorylates and activates the type I receptor. The type I receptor phosphorylates receptorbound Smads (R-Smads), allowing them to interact with Smad4, and this complex translocates into the nucleus. The ternary Smad complex (RSmads and Smad4) then contributes to higher order complexes with transcription factors and cofactors that regulate target gene transcriptions. Adapted from Ref. 44. J Appl Physiol • VOL 104 • MARCH 2008 • www.jap.org Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 receptor complex then phosphorylates a receptor-regulated Smad protein that oligomerizes with a common Smad or co-Smad termed Smad4. The Smad oligomer translocates into the nucleus where it interacts with Smad binding partners to regulate transcription (27). These Smad binding partners regulate, in a cell type-specific manner, subsets of genes that are target genes of TGF- signaling. Another group of Smads, inhibitor Smads (Smad6 and Smad7) serve to abrogate TGF- signaling by establishing an autoinhibitory feedback loop. Invited Review TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE 581 Fig. 3. Schematic diagram depicting the states of skeletal muscle development in the mouse. Stages of skeletal muscle development: 1) determination; 2) differentiation (embryonic and fetal); and 3) maturation. Determination ends with the formation of the myotome from the dermomyotome. Embryonic myoblasts differentiate and fuse to form primary muscle fibers. Fetal myoblasts then undergo differentiation to form secondary fibers that surround the primary fibers (13, 33). Dpc, days postconception in the mouse. ROLE OF TGF- AND MYOSTATIN IN SKELETAL MUSCLE DEVELOPMENT Since it would be untenable to consider all TGF- ligands, we will focus on the protypical TGF-1 and myostatin ligands because of their potent role in skeletal muscle (35, 37, 38, 47). TGF-1 and myostatin signaling in skeletal muscle involve two strikingly similar pathways, which mediate some overlapping and also mutually exclusive effects. TGF-1 plays an important role in skeletal muscle development but also influences different tissues producing a plethora of outcomes. TGF-1 activity is very specific to the cellular context, that is, its signaling outcome is determined by the intracellular milieu of the cell. This duplicitous nature of TGF-1 proves to be necessary for its in vivo function since it regulates many tissues and processes. Conversely, myostatin plays a much more J Appl Physiol • VOL restricted role in skeletal muscle development, muscle mass regulation, and adipose tissue. The elucidation of the role of TGF-1 in skeletal muscle began in experiments using cultured muscle cells in vitro, while the understanding of the role of myostatin began in vivo through gene targeting experiments in mice. These two different starting points led to different insights into the role of these interrelated pathways. TGF-1 is the archetypal cytokine of this superfamily and much of the understanding of the components of the TGF- signaling pathway have been delineated by the study of TGF-1. Conversely, because of the pervasive hypermuscular phenotype of myostatin null mice, myostatin research has focused more on clinical applications in skeletal muscle and less on the detailed biochemical dissection of its cognate signaling pathway. In the late 1980s, several groups made three key observations that enabled the identification of an important in vivo role for TGF- in skeletal muscle development. First, TGF- is present in large amounts in the limb bud, is produced in the ectoderm, and affects the adjacent mesenchymal cells. Second, TGF- inhibits differentiation of fetal, but not embryonic, myoblasts (80). Last, the treatment of limb bud organ cultures with TGF- neutralizing antibodies results in the premature appearance of large myotubes (secondary; Ref. 14). These observations suggest that TGF- prevents premature differentiation in migrating myoblasts, allowing for proper muscle formation in the developing embryonic limb. Myostatin was discovered during a screen for novel mammalian members of the TGF- superfamily (54). Expression of myostatin mRNA is first seen at embryonic day 9.5 post conception in the myotome of developing somites and continues throughout muscle development. The myostatin gene is expressed in adult skeletal muscle, heart, and adipose tissue (69). In addition to its restricted pattern of expression, mice homozygous null for the myostatin gene are two to three times larger in mass than the wild type due to an enhanced mass of the musculature (Fig. 1, A and B). The increase in skeletal muscle mass is attributed to both hyperplasia (increase in muscle fiber number) and hypertrophy (increase in muscle fiber size). Myostatin homozygous null mice also have reduced stores of adipose tissue (53, 54). Furthermore, heterozygous (⫹/⫺) myostatin mice have a 25% increase in body weight, which is a lesser effect than that seen in the homozygous (⫺/⫺) mice, suggesting a dose-dependent effect of myostatin protein levels on skeletal muscle mass. Naturally occurring 104 • MARCH 2008 • www.jap.org Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 and fuse to form primary muscle fibers, but some continue to proliferate and become fetal myoblasts. These fetal myoblasts form secondary fibers, smaller than the primary fibers, which surround the primary fibers (13). Fetal myogenesis is more similar to postnatal muscle regeneration than embryonic myogenesis. Postnatally, myotubes mature into muscle fibers. In the adult, skeletal muscle regeneration begins with quiescent satellite cells, located between the basal lamina and the sarcolemma of the muscle fiber, that become activated by trauma, be it mechanical or biological (e.g., disease). Recent work has classified satellite cells as a heterogeneous population of cells comprised of stem cells and committed progenitors based on the combined Pax7 and Myf5 status of the cells (32). Once activated, satellite cells proliferate, undergo differentiation, and then fuse to an existing muscle fiber or alternately create fibers de novo (see review, Refs. 9, 26). Two families of transcriptional regulatory proteins are critical in regulating developmental myogenesis: the muscle regulatory factors (MRFs) and the myocyte enhancer factor 2 (MEF2) proteins. MRF members are considered the prototypic master regulatory genes in skeletal muscle based on their capacity to convert some nonmyogenic fibroblast cells into a myogenic cell phenotype (61). MEF2 family members function as necessary coactivators for the MRFs in an evolutionarily conserved ancient code to specify skeletal muscle ontogeny (7). Both MRFs and MEF2 members have functional ciselements within many skeletal muscle-specific promoters and enhancers (7). Invited Review 582 TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE TGF- SIGNALING IN SKELETAL MUSCLE TGF- represses skeletal muscle specific gene expression and has also been reported to modulate proliferation in satellite cells (3, 12, 19, 24, 47, 59). Taken together, these studies indicate that TGF- reprograms gene expression in muscle cells resulting in an alteration of proliferative control and a potent inhibition of the program of gene expression underlying myogenic differentiation. As key orchestrators of muscle gene expression, the MRFs were shown to be targeted by TGF- signaling. Therefore, logical targets of TGF-1 are the myogenic transcription factors, the MRFs and the MEF2s, as the quintessential regulators of myogenesis. The MRFs are comprised of MyoD, Myf5, myogenin, and MRF4, whereas the MEF2s include MEF2A-D. To that end, Brennan and colJ Appl Physiol • VOL leagues (8) showed that TGF- inhibited the transcriptional activity of myogenin without affecting its DNA binding affinity. Furthermore, it has been shown that TGF-1 targets the basic helix-loop-helix (bHLH) region of all MRFs, decreasing their DNA transcriptional activity without affecting their binding properties (43). Not only does TGF-1 inhibit the transcriptional activity of the MyoD protein it also inhibits the transcription of the MyoD gene, thus reducing both levels and activity (76). How does TGF-1 inhibit myogenesis? What role do Smad2 and Smad3 have in myogenesis? In recent years several studies have begun to elucidate the role of Smad2 and Smad3 during TGF-1-mediated myogenic inhibition and in “normal” differentiation (39, 62). It has been shown that Smad3 is the key mediator of TGF- inhibition of myogenesis. Liu and colleagues (39) showed that Smad3 alone, and not Smad2, via MyoD inhibition is critical in TGF- signaling in myoblasts. Smad3 was found to physically interact with MyoD, inhibiting the transactivation properties of MyoD. Furthermore, Smad3 was also shown to physically interact with MEF2C and decrease its transcriptional activity (40). However, the relevance of this biochemical interaction in vivo is controversial because the MEF2C gene is not expressed in myoblasts endogenously (50), although MEF2C does play a role in the late stages of differentiation and conditional deletion in skeletal muscle affects sarcomere integrity (60). The role of Smad2 in TGF- inhibition of myogenesis is less clear. Using myoblasts De Angelis et al. (15) reported that MEF2, normally found in the nucleus, translocates to the cytoplasm upon TGF- treatment. Forced expression of MEF2C rescued TGF- inhibition by maintaining a pool of MEF2C in the nucleus. Furthermore, endogenous Smad2 and MEF2 are complexed together in the nuclei of differentiating myotubes, but not in myoblasts, where Smad2 is cytoplasmic and where MEF2A and 2C are not highly expressed (62). Thus the link between MEF2 and Smad2 protein is complex and may depend on the differentiation status of the cells. Together, these data suggest that Smad2 is an important component of TGF--mediated repression of differentiation in myoblasts, although the precise mechanism mediating this effect still requires further characterization (60). TGF- in skeletal muscle: a role in vivo. Recently, an in vivo role for TGF-1 in skeletal muscle regeneration was confirmed. Mice deficient in fibrillin-1 have increased TGF- signaling activity that causes a failure of skeletal muscle to regenerate (11). These mice are used as a model for the Marfan syndrome (MFS) in humans, which is caused by a mutation of the FBN1gene that encodes fibrillin-1 (an extracellular matrix protein). MFS symptoms include bone overgrowth, ocular lens dislocation, emphysema, cardiac complications, and an inability to increase skeletal muscle mass in response to exercise and other physiological signals (16). Antagonizing TGF- signaling with a TGF- neutralizing antibody or by losartan treatment rescues skeletal muscle regeneration in the fibrillin-1deficient mice. Increased TGF- signaling was also found in the skeletal muscle of dystrophin-deficient mice, a model of Duchenne muscular dystrophy, and antagonizing TGF- signaling restored the regeneration program in these mice (11). Furthermore, the fibrillin-1-deficient mice exhibited increased satellite cell numbers when TGF- was antagonized. Thus 104 • MARCH 2008 • www.jap.org Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 myostatin mutations in cattle (Belgian Blue, Piedmontese, and Marchigiana) and in humans have subsequently been shown also to lead to pronounced hypermuscularity (28, 42, 54, 68; Fig. 1, C-E). The consistency of the hypermuscular phenotype corresponding to myostatin null mutation across species is consistent with the evolutionary conservation of the myostatin gene and protein product between humans, mice, rats, pigs, cows, chickens, and turkeys. Since both TGF-1 and myostatin have been shown to regulate myogenesis and postnatal muscle physiology, a comparative analysis of the two may provide useful insights into the common and divergent aspects of the intracellular signaling of these pathways. TGF-1 signal transduction begins with the active ligand binding to the TGF- type II receptor (TRII) and either ALK-1 (activin like kinase-1) or TRI/ALK-5 (TGF- type I receptor) receptors. Myostatin signaling begins with the active myostatin ligand binding to either activin receptor type IIA (ActR-IIA) or ActR-IIB and either TRI/ ALK-5 or ALK-4, type I receptors (63). The myostatin ligand has a higher affinity for ActR-IIB in vitro (36, 63). Both pathways converge in the activation of Smad2 and Smad3 followed by oligomerization with Smad4. Next, the Smad complex translocates into the nucleus, where it regulates transcription of genes such as MyoD (39, 64). Additional nonSmad-dependent signaling has also been implicated in TGF-1 effects, although this is so far less well characterized (51). To counteract TGF-1/myostatin signaling, repression of the signal can be achieved by the I-Smads, Smad6 and Smad7, or a ubiquitin-mediated proteasomal degradation pathway mediated by the Smad-ubiquitin regulatory factors (SMURFS; Ref. 5). Smad7 has been previously shown to inhibit both TGF-1 and myostatin signaling (31, 82). Furthermore, Smad7 may have additional pro-myogenic functions. A recent study from our group (31) has shown a dramatic enhancement of skeletal muscle differentiation and growth by the myostatin signaling inhibitor Smad7, which interacts with and potentiates MyoD transcriptional activity. However, although Smad7 is able to inhibit TGF-1 signaling, as assessed by a TGF- responsive promoter (3TP-lux), it was not able to rescue TGF--mediated inhibition of myogenesis. Therefore, consideration of how the TGF-1/myostatin downstream effectors integrate with skeletal muscle-specific transcriptional regulators to control gene expression will be paramount in understanding how these growth factors modulate the muscle phenotype during development and regeneration. Invited Review TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE MYOSTATIN SIGNALING IN SKELETAL MUSCLE While the relevance of TGF-1 in vivo has just begun to be understood, the in vivo importance of myostatin was obvious from the early phase of its discovery. However, characterization of the intracellular signaling pathway for myostatin is still in its infancy. Much of what is known has been inferred by knowledge of the TGF- signaling pathway but there may still be some surprises to unfold since studies are now identifying differences in TGF-1 and myostatin signaling (31). Myostatin: a role in vivo. Myostatin null mice (Mstn⫺/⫺) have proved to be an excellent model for understanding the genetic role of myostatin during both muscle development and postnatal muscle physiology (52). In addition to alterations in muscle mass, changes in fiber contractile properties, fiber type, and fiber recovery have now been reported in this genetic model (4, 55, 79). In addition to the increased muscle mass and decreased fat in the Mstn⫺/⫺ mice there are also corresponding increases in strength and changes in fiber type distribution with a shift toward the type IIb fibers. Furthermore, the contractile properties of Mstn⫺/⫺ mice differed from heterozygous (Mstn⫹/⫺) and wild-type mice (55). In physiological studies of skeletal muscle derived from the mice, the extensor digitorum longus (EDL) muscle and the soleus muscle are often used as indicators of fast twitch and slow twitch muscle fibers, respectively. In vitro contractile analysis of EDL and soleus muscles from wild-type, Mstn⫹/⫺, and Mstn⫺/⫺ mice revealed that the maximum tetanic force (Po) in the EDL muscle and soleus muscle was greater in the Mstn⫺/⫺ than in the wild-type animals (55). Additionally, the specific maximum tetanic force (sPo; corrected for cross sectional area, N/mm2) was reduced in the Mstn⫺/⫺compared with the wild-type EDL muscle. However, in the soleus, no difference was found in the sPo of the Mstn⫺/⫺ compared with mice with the wild-type genotype. In the case of the EDL muscle, the phenomenon of decreased sPo with increased Po occurs because as the whole muscle cross sectional area increases the angle of pennation by muscle fibers J Appl Physiol • VOL increases, thus decreasing the transmission of force, a phenomenon previously described by Maxwell et al. (49). While the lack of any difference in the sPo of the soleus muscle is more difficult to explain, one possibility is that Po in the soleus muscle of the Mstn⫺/⫺ compared with the wild type was not large enough to affect the sPo. Interestingly, following two lengthening contractions, the EDL muscle from the Mstn⫺/⫺ mice had a greater force deficiency than the wild type. However, no difference in force production was found in the soleus muscle. Molecular analysis revealed that the levels of ActRIIB in the EDL muscle were twice as high as those in the soleus muscle suggesting that the higher levels of ActRIIB in the EDL muscle could prime it for greater sensitivity to the ligand compared with the soleus muscle. While Mendias et al. (55) have reported an increase in strength of the EDL of Mstn⫺/⫺ null mice, there is some conflict in this area since another study reported that Mstn⫺/⫺ null mice do not have increased Po generation in their EDL muscle compared with wild-type mice despite their larger muscle mass (4). However, consistent with other studies, the sPo in the myostatin-null state was reduced compared with that of their wild-type littermates. As well, the Po was slightly higher in the EDL muscle of the Mstn⫺/⫺ mice compared with the wild-type mice. Further comparison of the contractile properties of the EDL muscle from Mstn⫺/⫺ and wild-type mice exhibited differences in single twitch characteristics. EDL muscle from Mstn⫺/⫺ mice contracted and relaxed faster during a single twitch (4). A greater proportion of type IIb fibers in the Mstn⫺/⫺ mice can explain the shorter contraction and relaxation times reported. Assessed by myosin heavy chain (MHC) isoform expression, Mstn⫺/⫺ mice had less IIa and IIx fibers in EDL, but had more IIb fibers than the wild-type mice (4, 21). In the soleus muscle, Mstn⫺/⫺ mice had less IIa mRNA, but more IIx and IIb mRNA than the wild type, although this change at the mRNA level needs to be confirmed at the protein level. However, functional assessment using ATPase staining and succinate dehydrogenase (SDH) activity did confirm a shift toward more fast fibers and glycolytic fibers, respectively (21). The analysis of oxidative enzymes in the EDL muscle reported a decrease in mitochondrial enzymes, SDH, cytochrome oxidase (COX), and NADH reductase, in the Mstn⫺/⫺ mice consistent with the shift to fast glycolytic IIb fibers. Furthermore, the number of mitochondria per unit area was reduced. Taken together these data suggest that modification of myostatin levels does alter adult muscle contractile properties. Reduced myostatin levels have been shown to be potentially beneficial in aging muscle. Comparing older Mstn⫺/⫺ mice (24 mo) to older wild-type mice it was shown that Mstn⫺/⫺ mice had less IIb fibers and size losses compared with wild-type mice (70). Genetic removal of myostatin from conception exhibits profound effects on muscle mass and fiber type, but another extant question concerns whether postnatal myostatin repression can also have the same effects. Reducing myostatin in mice postweaning through the use of myostatin neutralizing antibodies, or by postnatal conditional genetic targeting, also leads to increased muscle mass (77–79). Depending on the length of treatment and the age of the mice there is a 10 –30% increase in muscle mass with neutralizing antibodies (77). Whittemore and colleagues (79) reported that mice treated with neutralizing antibodies had increased skeletal muscle mass and 104 • MARCH 2008 • www.jap.org Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 inhibition of TGF- signaling results in an improved skeletal muscle profile in several genetically invoked myopathies. In vivo studies have also documented the presence of TGF- during muscle injury. Muscle injury caused by eccentric contractions (6), cardiotoxin injection (22), and muscle strain injury (72) resulted in increased TGF- transcript and protein levels within 48 h of injury. However, increases in TGF-1 and TGF-2 precursors did not correspondingly lead to an increase in TGF- activity following muscle strain, suggesting a delay in TGF- activation after injury (72). Furthermore, TGF- type I receptor expression is regulated by myotube excitability. TRI was downregulated when primary rat myotubes were electrically stimulated and upregulated in adult rat muscle 72 h after denervation (75). Thus careful dissection of the role of TGF- signaling in these in vivo contexts is warranted to further understand the role played by the endogenous cytokine. Nearly three decades have passed since the potent effects of TGF- on myogenesis were first reported and only recently has an in vivo role for TGF- begun to be elucidated. Future studies using tissue-specific gene targeting and the discovery of new TGF- pathway mediators may further elucidate the role of TGF- in skeletal muscle. 583 Invited Review 584 TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE J Appl Physiol • VOL myostatin as a negative regulator of fiber size. However, the decrease in myostatin mRNA during running is more difficult to reconcile as one would expect myostatin levels to increase with this perturbation. A possible mechanism for exercise modulation of myostatin mRNA may be through calcium-dependent signaling via calcineurin. Calcineurin is a calcium-dependent phosphatase that has been shown to play a key role in the control of muscle gene expression by its regulation of the nuclear factor of activated transcription (NFAT) transcriptional regulator (10). Myostatin mRNA was reduced in mouse plantaris muscle that was overloaded. However, when calcineurin is inhibited through the use of cyclosporin A, myostatin mRNA was maintained at normal levels, suggesting that calcineurin may play a potentially important role in the regulation of myostatin levels during muscle remodeling (56, 57). Furthermore, expression of constitutively activated calcineurin in transgenic mice results in higher levels of myostatin mRNA levels (56). In addition, a number of experimental manipulations that result in reduced levels of calcineurin activity, such as calmodulin-binding protein (CaMBP)-overexpressing mice, parvalbumin-overexpressing mice, and NFATc2 null mice also exhibited reduced myostatin mRNA levels (56). Collectively, these data clearly indicate a connection between calcineurin activity and myostatin mRNA levels. The next and, probably, most important question to address is whether the alteration in myostatin levels is fundamental to the adaptation of the muscle in these contexts. The question as to whether myostatin levels are functionally linked to muscle performance is indeed intriguing. A recent study suggests that it may be, based on the observation that in a particular breed of racing dogs (whippets), performance characteristics were correlated with a mutation in the myostatin gene in that the dogs with the mutation are faster than those with the wild-type allele (58). This is the first report of myostatin gene mutation leading to enhanced athletic performance. Although increased muscle mass and strength in myostatin null animals is firmly established, there has been little evidence to date that it necessarily translates to increased athletic performance. With regard to this issue, whippets heterozygous for a mutant copy of myostatin (mh/⫹) are more muscular than normal whippets, ⬃20% more mass/height compared with normals, and are among the fastest, as determined by their racing grade. Interestingly, whippets homozygous for the mutant copy of myostatin (mh/mh) are considerably more muscular (60% more mass/height) compared with normal whippets, but were not as fast as the heterozygous dogs. Thus it is important to consider that the balance between muscle mass and muscular performance may be more optimal in the heterozygous rather than the homozygous null state. FUTURE PERSPECTIVES Repressing TGF- and myostatin signaling in muscle could have potential therapeutic applications since both TGF- and myostatin activity are elevated in a variety of clinical conditions associated with muscle loss. Increased TGF- signaling in mice deficient in fibrillin-1 have impaired skeletal muscle regeneration (11). A correlation between enhanced myostatin levels and muscle atrophy has also been observed in AIDS (23), bed rest (81), limb unloading, and exposure to micro- 104 • MARCH 2008 • www.jap.org Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 increased grip strength. Critically, this was the first study in postnatal animals to show that repressing myostatin signaling not only increases muscle mass but also enhances functional muscle strength. Recently, postnatal conditional genetic targeting of myostatin also showed increase muscle mass (78). Older mice that have ceased normal muscle growth also respond to myostatin repression with increased muscle mass but to a lesser degree. Additionally, short-term inhibition of myostatin in aged mice (14 –16 mo) enhanced muscle regeneration and activated satellite cell activation (71). Since older mice retain the capability to respond to myostatin repression with increased muscle mass it is tantalizing to consider the possibility of treating sarcopenia, age-related loss of muscle mass and strength, by inhibiting myostatin. These findings indicate that repression of myostatin could proffer a treatment for sarcopenia. Furthermore, inhibiting the myostatin pathway using the iSmads could be another potentially therapeutic strategy for maintaining muscle mass in ageing animals. In concert with the functional consequence of loss of myostatin signaling, when myostatin signaling is increased, mice undergo a predicted severe muscle loss. In experiments in which mice were systemically administered myostatin, pronounced skeletal muscle loss was observed (83). These mice exhibited symptoms similar to those of cachexia, which occurs in many disease states such as cancer, heart failure, AIDS, and sepsis. Thus it is now becoming clear that myostatin has the capacity to act as a specific and potent negative regulator of skeletal muscle mass during development, which is also paralleled in postnatal skeletal muscle. Recently, several studies have implicated modulation of myostatin mRNA levels in response to altered functional demand imposed by exercise training. It is clear that resistance training represses myostatin mRNA. Long-term resistance training reduces myostatin levels in rodents and humans (20, 67). An acute bout of resistance exercise also inhibits myostatin mRNA expression in rodents and humans (25, 29). Furthermore, resistance training mitigates atrophy and increases in myostatin caused by skeletal muscle unloading in rodents (1). Interestingly, hypertrophic capability of an individual had no impact on the level of myostatin reduction caused by resistance exercise (30). Thus both long-term and acute resistance training inhibit myostatin mRNA expression. However, individuals with greater hypertrophy in response to training did not concomitantly have the lowest levels of myostatin. The effect of submaximal intensity running exercise on myostatin mRNA levels has also been reported (41). Acute bouts of both resistance exercise (3 sets of 10 repetitions at 70% 1RM) and submaximal running (75% V̇O2 max for 30 min) reduced myostatin mRNA levels in young untrained participants. Postexercise time points comparing the two modes of acute exercise showed that resistance exercise has a more pronounced and longer suppression of myostatin. Resistance exercise reduced myostatin over sixfold for 23 h (1–24 h postexercise) while submaximal running decreased myostatin over threefold for 3 h (8 –12 h postexercise). Myostatin expression is suppressed by both resistance exercise and running, but with the former being a much more robust suppressor. Thus these data implicate an inverse correlation between exercise training and myostatin mRNA levels in a variety of exercise regimens. Decreases in myostatin mRNA levels in response to resistance exercise are consistent with the known role of Invited Review TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE 12. 13. 14. 15. 16. 17. 18. 19. GRANTS This work is supported by grants to J. C. McDermott from the Canadian Institutes of Health Research (CIHR) and the Natural Sciences and Engineering Research Council (NSERC) of Canada. 20. 21. REFERENCES 1. Adams GR, Haddad F, Bodell PW, Tran PD, Baldwin KM. Combined isometric, concentric, and eccentric resistance exercise prevents unloading induced muscle atrophy in rats. J Appl Physiol 103: 1644 –1654, 2007. 2. Alevizopoulos A, Mermod N. Transforming growth factor-beta: the breaking open of a black box. Bioessays 19: 581–591, 1997. 3. Allen RE, Boxhorn LK. Regulation of skeletal muscle satellite cell proliferation and differentiation by transforming growth factor-beta, insulin-like growth factor I, and fibroblast growth factor. J Cell Physiol 138: 311–315, 1989. 4. Amthor H, Macharia R, Navarrete R, Schuelke M, Brown SC, Otto A, Voit T, Muntoni F, Vrbova G, Partridge T, Zammit P, Bunger L, Patel K. Lack of myostatin results in excessive muscle growth but impaired force generation. Proc Natl Acad Sci USA 104: 1835–1840, 2007. 5. Attisano L, Silvestri C, Izzi L, Labbe E. The transcriptional role of Smads and FAST (FoxH1) in TGFbeta and activin signalling. Mol Cell Endocrinol 180: 3–11, 2001. 6. Barash IA, Mathew L, Lahey M, Greaser ML, Lieber RL. Muscle LIM protein plays both structural and functional roles in skeletal muscle. Am J Physiol Cell Physiol 289: C1312–C1320, 2005. 7. Black BL, Olson EN. Transcriptional control of muscle development by myocyte enhancer factor-2 (MEF2) proteins. Annu Rev Cell Dev Biol 14: 167–196, 1998. 8. Brennan TJ, Edmondson DG, Li L, Olson EN. Transforming growth factor beta represses the actions of myogenin through a mechanism independent of DNA binding. Proc Natl Acad Sci USA 88: 3822–3826, 1991. 9. Charge SB, Rudnicki MA. Cellular and molecular regulation of muscle regeneration. Physiol Rev 84: 209 –238, 2004. 10. Chin ER, Olson EN, Richardson JA, Yang Q, Humphries C, Shelton JM, Wu H, Zhu W, Bassel-Duby R, Williams RS. A calcineurindependent transcriptional pathway controls skeletal muscle fiber type. Genes Dev 12: 2499 –2509, 1998. 11. Cohn RD, van EC, Habashi JP, Soleimani AA, Klein EC, Lisi MT, Gamradt M, Ap Rhys CM, Holm TM, Loeys BL, Ramirez F, Judge DP, Ward CW, Dietz HC. Angiotensin II type 1 receptor blockade J Appl Physiol • VOL 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. attenuates TGF-beta-induced failure of muscle regeneration in multiple myopathic states. Nat Med 13: 204 –210, 2007. Cook DR, Doumit ME, Merkel RA. Transforming growth factor-beta, basic fibroblast growth factor, and platelet-derived growth factor-BB interact to affect proliferation of clonally derived porcine satellite cells. J Cell Physiol 157: 307–312, 1993. Cossu G, Biressi S. Satellite cells, myoblasts and other occasional myogenic progenitors: possible origin, phenotypic features and role in muscle regeneration. Semin Cell Dev Biol 16: 623– 631, 2005. Cusella-De Angelis MG, Molinari S, Le DA, Coletta M, Vivarelli E, Bouche M, Molinaro M, Ferrari S, Cossu G. Differential response of embryonic and fetal myoblasts to TGF beta: a possible regulatory mechanism of skeletal muscle histogenesis. Development 120: 925–933, 1994. De Angelis L, Borghi S, Melchionna R, Berghella L, Baccarani-Contri M, Parise F, Ferrari S, Cossu G. Inhibition of myogenesis by transforming growth factor beta is density-dependent and related to the translocation of transcription factor MEF2 to the cytoplasm. Proc Natl Acad Sci USA 95: 12358 –12363, 1998. Dietz HC, Cutting GR, Pyeritz RE, Maslen CL, Sakai LY, Corson GM, Puffenberger EG, Hamosh A, Nanthakumar EJ, Curristin SM. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352: 337–339, 1991. Feng XH, Derynck R. Specificity and versatility in TGF- signaling through Smads. Annu Rev Cell Dev Biol 21: 659 – 693, 2005. Flanders KC, Ludecke G, Engels S, Cissel DS, Roberts AB, Kondaiah P, Lafyatis R, Sporn MB, Unsicker K. Localization and actions of transforming growth factor-s in the embryonic nervous system. Development 113: 183–191, 1991. Florini JR, Roberts AB, Ewton DZ, Falen SL, Flanders KC, Sporn MB. Transforming growth factor-. A very potent inhibitor of myoblast differentiation, identical to the differentiation inhibitor secreted by Buffalo rat liver cells. J Biol Chem 261: 16509 –16513, 1986. Garma T, Kobayashi C, Haddad F, Adams GR, Bodell PW, Baldwin KM. Similar acute molecular responses to equivalent volumes of isometric, lengthening, or shortening mode resistance exercise. J Appl Physiol 102: 135–143, 2007. Girgenrath S, Song K, Whittemore LA. Loss of myostatin expression alters fiber-type distribution and expression of myosin heavy chain isoforms in slow- and fast-type skeletal muscle. Muscle Nerve 31: 34 – 40, 2005. Goetsch SC, Hawke TJ, Gallardo TD, Richardson JA, Garry DJ. Transcriptional profiling and regulation of the extracellular matrix during muscle regeneration. Physiol Genomics 14: 261–271, 2003. Gonzalez-Cadavid NF, Taylor WE, Yarasheski K, Sinha-Hikim I, Ma K, Ezzat S, Shen R, Lalani R, Asa S, Mamita M, Nair G, Arver S, Bhasin S. Organization of the human myostatin gene and expression in healthy men and HIV-infected men with muscle wasting. Proc Natl Acad Sci USA 95: 14938 –14943, 1998. Greene EA, Allen RE. Growth factor regulation of bovine satellite cell growth in vitro. J Anim Sci 69: 146 –152, 1991. Haddad F, Adams GR. Aging-sensitive cellular and molecular mechanisms associated with skeletal muscle hypertrophy. J Appl Physiol 100: 1188 –1203, 2006. Hawke TJ, Garry DJ. Myogenic satellite cells: physiology to molecular biology. J Appl Physiol 91: 534 –551, 2001. Jayaraman L, Massague J. Distinct oligomeric states of SMAD proteins in the transforming growth factor-beta pathway. J Biol Chem 275: 40710 – 40717, 2000. Kambadur R, Sharma M, Smith TP, Bass JJ. Mutations in myostatin (GDF8) in double-muscled Belgian Blue and Piedmontese cattle. Genome Res 7: 910 –916, 1997. Kim JS, Cross JM, Bamman MM. Impact of resistance loading on myostatin expression and cell cycle regulation in young and older men and women. Am J Physiol Endocrinol Metab 288: E1110 –E1119, 2005. Kim JS, Petrella JK, Cross JM, Bamman MM. Load-mediated downregulation of myostatin mRNA is not sufficient to promote myofiber hypertrophy in humans: a cluster analysis. J Appl Physiol 103: 1488 – 1495, 2007. Kollias HD, Perry RL, Miyake T, Aziz A, McDermott JC. Smad7 promotes and enhances skeletal muscle differentiation. Mol Cell Biol 26: 6248 – 6260, 2006. Kuang S, Kuroda K, Le GF, Rudnicki MA. Asymmetric self-renewal and commitment of satellite stem cells in muscle. Cell 129: 999 –1010, 2007. 104 • MARCH 2008 • www.jap.org Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 gravity (34). These observations position myostatin as a strong therapeutic target for manipulating phenotypic muscle mass in disease states and throughout the mammalian life span. Controversially, preliminary evidence in dogs indicates that myostatin inhibition may also potentially have ergogenic properties for athletic performance in events that require strength and power such as sprinting. On the molecular mechanistic level, much work still needs to be done to fully understand the intracellular mechanisms of the TGF- and myostatin signaling pathways in skeletal muscle. To date, very few TGF- or myostatin target genes have been annotated and this analysis needs to be carried out on a genome wide level. Clearly there are overlapping but also distinct features of the signaling initiated by these two cytokines that may result from common and divergent modulation of gene expression programs. Also, the role of the inhibitor Smads, such as Smad7, are intriguing because of their capacity to reverse the signaling and dramatically impinge on muscle cell differentiation and growth (31). Manipulation of TGF- and myostatin signaling thus holds considerable promise for the modulation of skeletal muscle mass and strength. This may have important implications for skeletal muscle regeneration in disease or injury states and also for skeletal muscle maintenance in the ageing population. 585 Invited Review 586 TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE J Appl Physiol • VOL 58. Mosher DS, Quignon P, Bustamante CD, Sutter NB, Mellersh CS, Parker HG, Ostrander EA. A mutation in the myostatin gene increases muscle mass and enhances racing performance in heterozygote dogs. PLoS Genet 3: e79, 2007. 59. Olson EN, Sternberg E, Hu JS, Spizz G, Wilcox C. Regulation of myogenic differentiation by type beta transforming growth factor. J Cell Biol 103: 1799 –1805, 1986. 60. Potthoff MJ, Arnold MA, McAnally J, Richardson JA, Bassel-Duby R, Olson EN. Regulation of skeletal muscle sarcomere integrity and postnatal muscle function by Mef2c. Mol Cell Biol 27: 8143– 8151, 2007. 61. Pownall ME, Gustafsson MK, Emerson CP Jr. Myogenic regulatory factors and the specification of muscle progenitors in vertebrate embryos. Annu Rev Cell Dev Biol 18: 747–783, 2002. 62. Quinn ZA, Yang CC, Wrana JL, McDermott JC. Smad proteins function as co-modulators for MEF2 transcriptional regulatory proteins. Nucleic Acids Res 29: 732–742, 2001. 63. Rebbapragada A, Benchabane H, Wrana JL, Celeste AJ, Attisano L. Myostatin signals through a transforming growth factor beta-like signaling pathway to block adipogenesis. Mol Cell Biol 23: 7230 –7242, 2003. 64. Rios R, Carneiro I, Arce VM, Devesa J. Myostatin is an inhibitor of myogenic differentiation. Am J Physiol Cell Physiol 282: C993–C999, 2002. 65. Roberts AB, Anzano MA, Lamb LC, Smith JM, Sporn MB. New class of transforming growth factors potentiated by epidermal growth factor: isolation from non-neoplastic tissues. Proc Natl Acad Sci USA 78: 5339 – 5343, 1981. 66. Roberts AB, Flanders KC, Heine UI, Jakowlew S, Kondaiah P, Kim SJ, Sporn MB. Transforming growth factor-beta: multifunctional regulator of differentiation and development. Philos Trans R Soc Lond B Biol Sci 327: 145–154, 1990. 67. Roth SM, Martel GF, Ferrell RE, Metter EJ, Hurley BF, Rogers MA. Myostatin gene expression is reduced in humans with heavy-resistance strength training: a brief communication. Exp Biol Med 228: 706 –709, 2003. 68. Schuelke M, Wagner KR, Stolz LE, Hubner C, Riebel T, Komen W, Braun T, Tobin JF, Lee SJ. Myostatin mutation associated with gross muscle hypertrophy in a child. N Engl J Med 350: 2682–2688, 2004. 69. Sharma M, Kambadur R, Matthews KG, Somers WG, Devlin GP, Conaglen JV, Fowke PJ, Bass JJ. Myostatin, a transforming growth factor-beta superfamily member, is expressed in heart muscle and is upregulated in cardiomyocytes after infarct. J Cell Physiol 180: 1–9, 1999. 70. Siriett V, Platt L, Salerno MS, Ling N, Kambadur R, Sharma M. Prolonged absence of myostatin reduces sarcopenia. J Cell Physiol 209: 866 – 873, 2006. 71. Siriett V, Salerno MS, Berry C, Nicholas G, Bower R, Kambadur R, Sharma M. Antagonism of myostatin enhances muscle regeneration during sarcopenia. Mol Ther 15: 1463–1470, 2007. 72. Smith CA, Stauber F, Waters C, Alway SE, Stauber WT. Transforming growth factor-beta following skeletal muscle strain injury in rats. J Appl Physiol 102: 755–761, 2007. 73. Sparks RL, Scott RE. Transforming growth factor type beta is a specific inhibitor of 3T3 T mesenchymal stem cell differentiation. Exp Cell Res 165: 345–352, 1986. 74. Ten Dijke P, Goumans MJ, Itoh F, Itoh S. Regulation of cell proliferation by Smad proteins. J Cell Physiol 191: 1–16, 2002. 75. Ugarte G, Brandan E. Transforming growth factor beta (TGF-beta) signaling is regulated by electrical activity in skeletal muscle cells. TGF-beta type I receptor is transcriptionally regulated by myotube excitability. J Biol Chem 281: 18473–18481, 2006. 76. Vaidya TB, Rhodes SJ, Taparowsky EJ, Konieczny SF. Fibroblast growth factor and transforming growth factor beta repress transcription of the myogenic regulatory gene MyoD1. Mol Cell Biol 9: 3576 –3579, 1989. 77. Walsh FS, Celeste AJ. Myostatin: a modulator of skeletal-muscle stem cells. Biochem Soc Trans 33: 1513–1517, 2005. 78. Welle S, Bhatt K, Pinkert CA, Tawil R, Thornton CA. Muscle growth after postdevelopmental myostatin gene knockout. Am J Physiol Endocrinol Metab 292: E985–E991, 2007. 79. Whittemore LA, Song K, Li X, Aghajanian J, Davies M, Girgenrath S, Hill JJ, Jalenak M, Kelley P, Knight A, Maylor R, O’Hara D, Pearson A, Quazi A, Ryerson S, Tan XY, Tomkinson KN, Veldman GM, Widom A, Wright JF, Wudyka S, Zhao L, Wolfman NM. Inhibition of myostatin in adult mice increases skeletal muscle mass and strength. Biochem Biophys Res Commun 300: 965–971, 2003. 104 • MARCH 2008 • www.jap.org Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 33. Kubota T, Zhang Q, Wrana JL, Ber R, Aubin JE, Butler WT, Sodek J. Multiple forms of SppI (secreted phosphoprotein, osteopontin) synthesized by normal and transformed rat bone cell populations: regulation by TGF-beta. Biochem Biophys Res Commun 162: 1453–1459, 1989. 34. Lalani R, Bhasin S, Byhower F, Tarnuzzer R, Grant M, Shen R, Asa S, Ezzat S, Gonzalez-Cadavid NF. Myostatin and insulin-like growth factor-I and -II expression in the muscle of rats exposed to the microgravity environment of the NeuroLab space shuttle flight. J Endocrinol 167: 417– 428, 2000. 35. Lee SJ. Regulation of muscle mass by myostatin. Annu Rev Cell Dev Biol 20: 61– 86, 2004. 36. Lee SJ, McPherron AC. Regulation of myostatin activity and muscle growth. Proc Natl Acad Sci USA 98: 9306 –9311, 2001. 37. Lee SJ, McPherron AC. Myostatin and the control of skeletal muscle mass. Curr Opin Genet Dev 9: 604 – 607, 1999. 38. Li Y, Foster W, Deasy BM, Chan Y, Prisk V, Tang Y, Cummins J, Huard J. Transforming growth factor-beta1 induces the differentiation of myogenic cells into fibrotic cells in injured skeletal muscle: a key event in muscle fibrogenesis. Am J Pathol 164: 1007–1019, 2004. 39. Liu D, Black BL, Derynck R. TGF-beta inhibits muscle differentiation through functional repression of myogenic transcription factors by Smad3. Genes Dev 15: 2950 –2966, 2001. 40. Liu D, Kang JS, Derynck R. TGF-beta-activated Smad3 represses MEF2-dependent transcription in myogenic differentiation. EMBO J 23: 1557–1566, 2004. 41. Louis ES, Raue U, Yang Y, Jemiolo B, Trappe SW. Time course of proteolytic, cytokine, and myostatin gene expression after acute exercise in human skeletal muscle. J Appl Physiol 103: 1744 –1751, 2007. 42. Marchitelli C, Savarese MC, Crisa A, Nardone A, Marsan PA, Valentini A. Double muscling in Marchigiana beef breed is caused by a stop codon in the third exon of myostatin gene. Mamm Genome 14: 392–395, 2003. 43. Martin JF, Li L, Olson EN. Repression of myogenin function by TGF-beta 1 is targeted at the basic helix-loop-helix motif and is independent of E2A products. J Biol Chem 267: 10956 –10960, 1992. 44. Massague J. TGF-beta signal transduction. Annu Rev Biochem 67: 753– 791, 1998. 45. Massague J. How cells read TGF-beta signals. Nat Rev Mol Cell Biol 1: 169 –178, 2000. 46. Massague J. The transforming growth factor-beta family. Annu Rev Cell Biol 6: 597– 641, 1990. 47. Massague J, Cheifetz S, Endo T, Nadal-Ginard B. Type beta transforming growth factor is an inhibitor of myogenic differentiation. Proc Natl Acad Sci USA 83: 8206 – 8210, 1986. 48. Massague J, Gomis RR. The logic of TGF signaling. FEBS Lett 580: 2811–2820, 2006. 49. Maxwell LC, Faulkner JA, Hyatt GJ. Estimation of number of fibers in guinea pig skeletal muscles. J Appl Physiol 37: 259 –264, 1974. 50. McDermott JC, Cardoso MC, Yu YT, Andres V, Leifer D, Krainc D, Lipton SA, Nadal-Ginard B. hMEF2C gene encodes skeletal muscleand brain-specific transcription factors. Mol Cell Biol 13: 2564 –2577, 1993. 51. McFarlane C, Plummer E, Thomas M, Hennebry A, Ashby M, Ling N, Smith H, Sharma M, Kambadur R. Myostatin induces cachexia by activating the ubiquitin proteolytic system through an NF-kappaB-independent, FoxO1-dependent mechanism. J Cell Physiol 209: 501–514, 2006. 52. McPherron AC, Lawler AM, Lee SJ. Regulation of skeletal muscle mass in mice by a new TGF-beta superfamily member. Nature 387: 83–90, 1997. 53. McPherron AC, Lee SJ. Suppression of body fat accumulation in myostatin-deficient mice. J Clin Invest 109: 595– 601, 2002. 54. McPherron AC, Lee SJ. Double muscling in cattle due to mutations in the myostatin gene. Proc Natl Acad Sci USA 94: 12457–12461, 1997. 55. Mendias CL, Marcin JE, Calerdon DR, Faulkner JA. Contractile properties of EDL and soleus muscles of myostatin-deficient mice. J Appl Physiol 101: 898 –905, 2006. 56. Michel RN, Chin ER, Chakkalakal JV, Eibl JK, Jasmin BJ. Ca2⫹/ calmodulin-based signalling in the regulation of the muscle fibre phenotype and its therapeutic potential via modulation of utrophin A and myostatin expression. Appl Physiol Nutr Metab 32: 921–929, 2007. 57. Michel RN, Dunn SE, Chin ER. Calcineurin and skeletal muscle growth. Proc Nutr Soc 63: 341–349, 2004. Invited Review TGF- AND MYOSTATIN SIGNALING IN SKELETAL MUSCLE 80. Yanagisawa M, Nakashima K, Takeda K, Ochiai W, Takizawa T, Ueno M, Takizawa M, Shibuya H, Taga T. Inhibition of BMP2-induced, TAK1 kinase-mediated neurite outgrowth by Smad6 and Smad7. Genes Cells 6: 1091–1099, 2001. 81. Zachwieja JJ, Smith SR, Sinha-Hikim I, Gonzalez-Cadavid N, Bhasin S. Plasma myostatin-immunoreactive protein is increased after prolonged bed rest with low-dose T3 administration. J Gravit Physiol 6: 11–15, 1999. 587 82. Zhu X, Topouzis S, Liang LF, Stotish RL. Myostatin signaling through Smad2, Smad3 and Smad4 is regulated by the inhibitory Smad7 by a negative feedback mechanism. Cytokine 26: 262–272, 2004. 83. Zimmers TA, Davies MV, Koniaris LG, Haynes P, Esquela AF, Tomkinson KN, McPherron AC, Wolfman NM, Lee SJ. Induction of cachexia in mice by systemically administered myostatin. Science 296: 1486 –1488, 2002. Downloaded from http://jap.physiology.org/ by 10.220.33.4 on June 12, 2017 J Appl Physiol • VOL 104 • MARCH 2008 • www.jap.org