* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Digestive Ch23-part 2
Wilson's disease wikipedia , lookup
Glycogen storage disease type I wikipedia , lookup
Intestine transplantation wikipedia , lookup
Surgical management of fecal incontinence wikipedia , lookup
Liver transplantation wikipedia , lookup
Liver cancer wikipedia , lookup
Hepatic encephalopathy wikipedia , lookup
Cholangiocarcinoma wikipedia , lookup
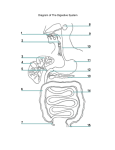
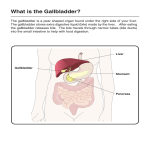
ppt Part 2 VI. Small Intestine & Associated Organs … B. Liver = largest gland in the body 1. Gross Anatomy a. 4 lobes: • Right– anterior surface • Left on Anterior surface Sternum Nipple Liver Bare area Falciform ligament Left lobe of liver Right lobe of liver Gallbladder (a) Round ligament (ligamentum teres) B. Liver … a. Lobes … • Caudate small, seen mainly posterosuperiorly; nest to V. Cava • Quadrate small and mainly seen posteroinferiorly below Left Lobe and next to gallbladder(“q” like “g”) b. Ligaments • Falciform Ligament: separates Right & Left lobes anteriorly and suspends liver from diaphragm • Round ligament (ligamentum teres) – remnant of umbilical vein Sternum Bare area Liver Right lobe of liver Gallbladder (a) Copyright © 2010 Pearson Education, Inc. Falciform ligament Left lobe of liver Round ligament (ligamentum teres) c. Ducts • Bile Duct (Common Bile Duct) • Common Hepatic Ducts • Cystic Duct • R&L Hepatic Right and left hepatic ducts of liver Cystic duct Common hepatic duct Bile duct Gallbladder (bile storage) Copyright © 2010 Pearson Education, Inc. Pancreas Jejunum d. Blood Vessels • Hepatic Artery • Hepatic Portal Vein • Hepatic Vein Lesser omentum (in fissure) Left lobe of liver Porta hepatis containing hepatic artery (left) and hepatic portal vein (right) Quadrate lobe of liver Ligamentum teres (b) Copyright © 2010 Pearson Education, Inc. Bare area Caudate lobe of liver Sulcus for inferior vena cava Hepatic vein (cut) Bile duct (cut) Right lobe of liver Gallbladder 2. Microscopic Anatomy of Liver a. Liver lobules = hexagonal structural and functional units • Hepatocytes • Many rough & smooth ER, Golgi, peroxisomes • Functions: produce bile (900 ml per day) • Process nutrients from blood (glucose glycogen, …) • Store fat soluble vitamins • Detoxification (nitrogen from amino acids/ammonia urea, …) • Central vein drains filtered blood to Portal Triad Hepatic Veins Plates of Hepatocytes LOBULE Central 2. Microscopic Anatomy of Liver … b. Portal triad = bile duct, arteriole (from hepatic artery), hepatic venule (from portal vein) – both blood vessels branch into sinusoids: Blood flows toward central vein, bile toward triad c. Liver sinusoids = leaky capillaries between hepatic plates • Carry oxygenated blood and nutrient rich/oxygen poor blood Portal Triad Plates of Hepatocytes Central 2. Microscopic Anatomy … d. Kupffer cells (hepatic macrophages) in sinusoid walls e. Bile canaliculi feed bile ducts f. High regeneration capacity: from high blood flow, 80% removed regenerates Bile canaliculi Plates of Hepatocytes Sinusoids g. Bile • Function: Fat emulsifier • Particularly Bile Salts • Bile Composition: • Bile Salts (acids derived from cholesterol) • Pigments: bilirubin– break down product of RBCs • Cholesterol • Phospholipids • Bile Salts Recycled: reabsorbed in ileum then Enterohepatic Circulation— Hepatic Portal Vein Liver new bile g. Bile … • Health: Excess cholesterol can crystallize = gallstones • Control bile production • Secretin: released from intestinal cells exposed to fats stimulate Liver. • Recycled bile salts: as increase and recycle back to liver = major stimuli to liver for increased bile production Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. C. The Gallbladder • Muscular sac with Cystic Duct to Bile Duct • Function: Stores/concentrates (10-20 times) & releases bile • Control: • Cholecytokinin (CCK) major stimulus: released from duodenum when acidic fatty chyme enters duodenum Gallbladder • Causes contraction • Vagus nerve– minor stimulus • No digestion if: Hepatopancreatic Sphincter closed—bile backs up into gallbladder & is stored D. Pancreas • Parts: Head, tail, Main Duct • Location: • deep to greater curvature of stomach • Head encircled by duodenum; tail abuts spleen • Exocrine function: Pancreatic Juice • Acini = round cluster of secretory cells that secrete enzymes; enzymes need alkalinity Pancreas • Duct cells secrete bicarbonate: neutralizes stomach acid to pH of 8; cuboidal Small duct Acinar cells Tail Head of Pancreas Pancreas Islets Acinar cells Copyright © 2010 Pearson Education, Inc. Pancreas Acinar cells Pancreatic Duct, branch Copyright © 2010 Pearson Education, Inc. Pancreatic Juice … Exocrine Function … • Enzymes: Pancreas secretes enzymes for all 4 major Biochemical groups (food molecules) • Amylase, Lipases, Nucleases • secreted active; optimal activity with bile & ions • Proteases = secreted inactive (activated in duodenum) • Control: Secretin target Duct cells AND Cholecystokinin targets acinar cells Epithelial cells 1 of many brush border enzymes Membrane-bound enteropeptidase Trypsinogen Trypsin (inactive) Chymotrypsin Chymotrypsinogen (inactive) Carboxypeptidase Procarboxypeptidase (inactive) • Pancreas Endocrine Function: hormones insulin & glucagon from cells in the Islets of Langerhans Acinar cells Copyright © 2010 Pearson Education, Inc. E. Regulation of Bile & Pancreatic Secretion and Entry into the Sm. Intest. Stimulatory events Cephalic phase Gastric phase 1 Sight and thought of food Cerebral cortex Conditioned reflex 2 Stimulation of taste and smell receptors Hypothalamus and medulla oblongata 1 Stomach distension activates stretch receptors Vagovagal reflexes Intestinal Phase 1 Presence of low pH, partially digested foods, fats, or hypertonic solution in duodenum when stomach begins to empty Stimulate Inhibit Copyright © 2010 Pearson Education, Inc. Medulla Vagus nerve Vagus nerve Local reflexes 2 Food chemicals (especially peptides and caffeine) and rising pH activate chemoreceptors Intestinal phase Inhibitory events G cells Intestinal (enteric) gastrin release to blood Gastrin release to blood Lack of stimulatory impulses to parasympathetic center Cerebral cortex Gastrin secretion declines G cells Overrides parasympathetic controls Sympathetic nervous system activation 1 1 2 Stomach secretory activity Enterogastric reflex Brief effect Processing in Small IntestineFigure 23.17 Local reflexes Vagal nuclei in medulla Pyloric sphincter Release of intestinal hormones (secretin, cholecystokinin, vasoactive intestinal peptide) 1 Distension of duodenum; presence of fatty, acidic, hypertonic chyme, and/or irritants in the duodenum 2 Distension; presence of fatty, acidic, partially digested food in the duodenum E. Regulation of Bile & Pancreatic Secretion and Entry into the Small Intestine Continuation after intestinal phase of Stomach: 1. Cholecystokinin & Secretin released • Stimulus = Chyme entering Duodenum • CCK & Secretin potentiate (syngergistic)one another 2. Hormones Blood 3. Hepatopancreatic Sphincter relaxes (CCK) 4. Pancreatic Juice secreted (CCK & Secretin) 5. Liver produces more bile (Secretin, Bile Salts) 6. Gallbladder contracts (CCK) 7. Secretions enter Duodenum Copyright © 2010 Pearson Education, Inc. 8. Absorption across ample surface area (circular folds, villi, microvilli) • Breakdown products of carbohydrate protein, fat, & nucleic acid digestion 9. Peristalsis: occurs after most nutrients have been absorbed; 10. Ileocecal Sphincter relaxes • Next Meal, increased stomach activity increased segmentation in Ileum • Gastrin from stomach relaxes ileocecal sphincter remaining substances move into Lg. Intestine • Sm. Intestine is emptied START ALL OVER AGAIN WITH CYCLE VII. Large Intestine A. Gross Anatomy 1. Parts = Colon, Cecum, appendix, Rectum, & Anal Canal 2. Gross Anatomy • Teniae coli – Reduction of the 3 bands of longitudinal smooth muscle in muscularis to a thin band Transverse colon Haustrum Ascending colon IIeum IIeocecal valve Cecum Rectum Vermiform appendix Anal canal Epiploic appendages Descending colon Teniae coli Sigmoid colon VII. Large Intestine … 2. Gross Anatomy • Haustra - pocketlike sacs caused by tone of teniae coli • Epiploic appendages - fat-filled pouches of visceral peritoneum a) Veriform Appendix Transverse colon Haustrum Ascending colon IIeum IIeocecal valve Cecum Rectum Vermiform appendix Anal canal Epiploic appendages Descending colon Teniae coli Sigmoid colon b. Cecum c. Colon • Ascending Colon • Right Colic (Hepatic) Flexure • Transverse Colon • Left Colic (Splenic) Flexure • Descending Colon • Sigmoid Colon d. Rectum & Anal Canal • 3 rectal valves stop feces from being passed with gas Copyright © 2010 Pearson Education, Inc. d. Rectum and Anus … • Rectum … • Well-developed muscularis Rectum Rectal valve Hemorrhoidal veins • Anal Canal • Internal anal sphincter— smooth muscle • External anal sphincter— skeletal muscle Anal canal B. Bacterial Flora • Enter from small intestine or anus • Ferment indigestible carbs • Release irritating acids and gases • Synthesize B complex vitamins and vitamin K C. Microscopic Anatomy 1. Mucosa • Simple Columnar ET w/ many Goblet Cells • Stratified Squamous in Anal Canal Copyright © 2010 Pearson Education, Inc. Colon Copyright © 2010 Pearson Education, Inc. D. Functions of the Large Intestine • Vitamins, water, and electrolytes reclaimed • Major function = propel feces to anus • Slow segmentation by haustra gradually move contents distally • Gastrocolic reflex = food in stomach causes 3-4 mass peristaltic waves thru colon per day PART 3 Physiology of Digestion and Absorption I. Carbohydrates: Polysaccharides disaccharides & Monosaccharides II. PROTEINS: III. Lipids IV. Nucleic Acids Copyright © 2010 Pearson Education, Inc. END Copyright © 2010 Pearson Education, Inc. Review Questions The digestive function of the liver is to produce _______ bile which functions in the chemical lipids digestion of _________. Liver _________ lobules are the functional units of the liver which contain a central vein and peripheral portal __________ with what 3 components? triads arteriole, hepatic venule, and bile duct Review Questions CCK stimulates the release of pancreatic enzymes ________ contraction of the gall bladder while ________ secretin and __________ stimulates the release of bicarbonate __________ - rich pancreatic chyme from the secretion to neutralize acidic _________ stomach. proteins Enzymes that break down __________ must be activated in the duodenum. Copyright © 2010 Pearson Education, Inc. Review Questions Motilin is released during the ‘fasting state’ by _________ the __________ duodenum and initiates the ___________ migrating motility complex that gradually moves residues to large intestine the _________ ____________. Conscious control of defecation is via relaxation of external anal sphincter. the ___________ Review Questions Amylase, lactase, and sucrase (among others) are enzymes that help break down carbohydrates ___________. active Amino acids are absorbed from the lumen via __________ transport. emulsified by bile salts, then travel as Fats are first _________ micelles between microvilli, and are finally converted to ________ chylomicrons in the absorptive cells before being _____________ lacteals as part of the lymph. carried away in the ________ 1 Chyme in duodenum = release of cholecystokinin (CCK) + secretin from duodenal enteroendocrine cells. Bile and Pancreatic Juice Regulation Figure 23.28, step 1 1 Chyme entering duodenum causes release of cholecystokinin (CCK) and secretin from duodenal enteroendocrine cells. 2 CCK (red dots) and secretin (yellow dots) enter the bloodstream. CCK = secretion of enzyme-rich pancreatic juice. Secretin = secretion of HCO3–-rich pancreatic juice. CCK and secretin potentiate one another 3 Figure 23.28, step 3 1 Chyme entering duodenum causes release of cholecystokinin (CCK) and secretin from duodenal enteroendocrine cells. 4 Bile salts returning from ileum + secretin = liver produces bile more rapidly. 2 CCK (red dots) and secretin (yellow dots) enter the bloodstream. 3 CCK induces secretion of enzyme-rich pancreatic juice. Secretin causes secretion of HCO3–-rich pancreatic juice. Figure 23.28, step 4 1 Chyme entering duodenum causes release of cholecystokinin (CCK) and secretin from duodenal enteroendocrine cells. 2 CCK (red dots) and secretin (yellow dots) enter the bloodstream. 3 CCK induces secretion of enzyme-rich pancreatic juice. Secretin causes secretion of HCO3–-rich pancreatic juice. 4 Bile salts and, to a lesser extent, secretin transported via bloodstream stimulate liver to produce bile more rapidly. 5 CCK also = gallbladder contracts + hepatopancreatic sphincter relaxes; bile enters duodenum. Figure 23.28, step 5 1 Chyme entering duodenum causes release of cholecystokinin (CCK) and secretin from duodenal enteroendocrine cells. 2 CCK (red dots) and secretin (yellow dots) enter the bloodstream. 3 CCK induces secretion of enzyme-rich pancreatic juice. Secretin causes secretion of HCO3–-rich pancreatic juice. 4 Bile salts and, to a lesser extent, secretin transported via bloodstream stimulate liver to produce bile more rapidly. 5 CCK (via bloodstream) causes gallbladder to contract and hepatopancreatic sphincter to relax; bile enters duodenum. 6 Cephalic and gastric phases, vagal nerve causes weak contractions of gallbladder. Figure 23.28, step 6 Carbohydrate digestion Foodstuff Enzyme(s) and source Site of action Starch and disaccharides Oligosaccharides and disaccharides Lactose Maltose Sucrose Galactose Glucose Fructose Salivary amylase Pancreatic amylase Brush border enzymes in small intestine (dextrinase, glucoamylase, lactase, maltase, and sucrase) Mouth Small intestine Path of absorption • Glucose/galactose absorbed via cotransport w/ Na+. • Fructose passes via facilitated diffusion. • All Small intestine monosaccharides leave epithelia via facilitated diffusion, enter capillary blood in villi, and transported to liver via hepatic portal vein. Lumen of intestine Amino acids of protein fragments Brush border enzymes Apical membrane (microvilli) Pancreatic proteases 1 Proteins digested to amino acids by pancreatic proteases (trypsin, chymotrypsin, carboxypeptidase) + brush border enzymes (carboxypeptidase, aminopeptidase, dipeptidase). Na+ Na+ Absorptive epithelial cell 2 amino acids absorbed by active transport into absorptive cells. Amino acid carrier Active transport Passive transport 3 Capillary Amino acids leave villus by facilitated diffusion, enter capillary via intercellular clefts. Figure 23.33 Protein digestion Foodstuff Protein Large polypeptides Small polypeptides, small peptides Amino acids (some dipeptides and tripeptides) Enzyme(s) and source Pepsin (stomach glands) in presence of HCl Pancreatic enzymes (trypsin, chymotrypsin, carboxypeptidase) Brush border enzymes (aminopeptidase, carboxypeptidase, and dipeptidase) Site of action Path of absorption • Amino acids are absorbed by cotransport with Stomach sodium ions. • Some dipeptides and tripeptides are absorbed via cotransport with H++ Small and hydrolyzed to amino intestine acids within the cells. • Amino acids leave the epithelial cells by Small facilitated diffusion, enter intestine the capillary blood in the villi, and are transported to the liver via the hepatic portal vein. Figure 23.32 (2 of 4) Fat digestion Foodstuff Enzyme(s) and source Unemulsified fats Emulsification by the detergent action of bile salts ducted in from the liver Pancreatic lipases Monoglycerides Glycerol and fatty acids and fatty acids Site of action Path of absorption • Fatty acids and monoglycerides enter the intestinal cells via diffusion. Small intestine • Fatty acids and monoglycerides are recombined to form triglycerides and then combined with other lipids and proteins within the cells, and the resulting chylomicrons are Small extruded by exocytosis. intestine • The chylomicrons enter the lacteals of the villi and are transported to the systemic circulation via the lymph in the thoracic duct. • Some short-chain fatty acids are absorbed, move into the capillary blood in the villi by diffusion, and are transported to the liver via the hepatic portal vein. Figure 23.32 (3 of 4) Nucleic acid digestion Foodstuff Enzyme(s) and source Site of action Nucleic acids Pentose sugars, N-containing bases, phosphate ions Path of absorption • Enter Pancreatic ribonuclease and deoxyribonuclease Brush border enzymes (nucleosidases and phosphatases) Small intestine intestinal cells by active transport via membrane carriers. Small • Absorbed intestine capillaries, into villi transported to liver via hepatic portal vein. Figure 23.32 (4 of 4) E. Regulation of Bile & Pancreatic Secretion and Entry into the Sm. Intest. Regulation of Gastric Secretion-- REVIEW Stimulatory events Cephalic phase Gastric phase 1 Sight and thought of food Cerebral cortex Conditioned reflex 2 Stimulation of taste and smell receptors Hypothalamus and medulla oblongata 1 Stomach distension activates stretch receptors Vagovagal reflexes 1 Presence of low pH, partially digested foods, fats, or hypertonic solution in duodenum when stomach begins to empty Stimulate Inhibit Copyright © 2010 Pearson Education, Inc. Medulla Vagus nerve Vagus nerve Local reflexes 2 Food chemicals (especially peptides and caffeine) and rising pH activate chemoreceptors Intestinal phase Inhibitory events G cells Intestinal (enteric) gastrin release to blood Gastrin release to blood Lack of stimulatory impulses to parasympathetic center Cerebral cortex Gastrin secretion declines G cells Overrides parasympathetic controls Sympathetic nervous system activation 1 Loss of appetite, depression 1 Excessive acidity (pH <2) in stomach 2 Emotional upset Stomach secretory activity Enterogastric reflex Brief effect Processing in Small IntestineFigure 23.17 Local reflexes Vagal nuclei in medulla Pyloric sphincter Release of intestinal hormones (secretin, cholecystokinin, vasoactive intestinal peptide) 1 Distension of duodenum; presence of fatty, acidic, hypertonic chyme, and/or irritants in the duodenum 2 Distension; presence of fatty, acidic, partially digested food in the duodenum F. Digestion in the Small Intestine 1. Overall Function: finish digestion/absorb nutrients & water 2. Hypertonic Chyme moved slowly into Duodenum from stomach via slow peristalsis (3ml) • Chyme = acidic and hypertonic w/ partially digested carbohydrates/proteins & undigested fats • Pancreatic juices neutralize chime & make it isotonic 3. Segmentation Mixes chime w/ bile & pancreatic secretions and moves chime slowly towards Ileum