* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Somatic sensation and pain
Survey
Document related concepts
Transcript
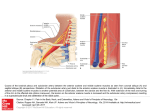
SOMATIC SENSATION AND PAIN Zoltán Pfund, MD, PhD University of Pécs Department of Neurology CONTENTS • • • • • • Anatomy and physiology of somatic sensation Interruption of sensory pathways Pain and nociception Anatomy and physiology of pain Pain disorders Therapy of pain University of Pé Pécs, cs, Department of Neurology SENSORY AFFERENTS CUTAN MECHANORECEPTORS University of Pé Pécs, cs, Department of Neurology SENSORY AFFERENTS CUTAN MECHANORECEPTORS • Fast Adapting Touch-Pressure Receptors Hair follicle receptor Meissner endings – hairless skin – Aβ Respond to flutter, flutter, motion Pacinian corpuscle – dermis – Aβ Responds to vibration vibration University of Pé Pécs, cs, Department of Neurology SENSORY AFFERENTS CUTAN MECHANORECEPTORS • Slowly Adapting Touch-Pressure Receptors Free nerve endings - hairy & hairless skin - C fibers Tickle & light or superficial touch Merkels discs - in both hairy and hairless skin – Aβ Pressure, form, texture Ruffini endings - hairy and some in hairless skin - Aβ Respond to lateral stretch of the skin and steady pressure University of Pé Pécs, cs, Department of Neurology SENSORY AFFERENTS JOINT & MUSCLE RECEPTORS • Proprioceptive Receptors Receptors in muscles, tendons and joints Joint afferents – diverse receptors – Aα Protective function Muscle spindle is a major stretch receptor - Aβ Respond to muscle length Golgi organs in tendons - Aα Respond to muscle tension University of Pé Pécs, cs, Department of Neurology SENSORY AFFERENTS TEMPERATURE RECEPTORS • Temperature Receptors Separate warm and cold receptors Free nerve endings Warm receptors - C fibers Respond to increasing temperature Cold receptors - Aδ fibers Respond to decreasing temperature University of Pé Pécs, cs, Department of Neurology SENSORY AFFERENTS NOCICEPTORS • Nocioceptors Free nerve endings: mechano and thermoreceptors, thermoreceptors, polymodal nociceptors C fibers – dull/burning pain – slow pain Aδ fibers - sharp pricking & stinging pain – fast pain University of Pé Pécs, cs, Department of Neurology SENSORY AFFERENTS PRIMARY AFFERENT FIBERS Large Medium Small Unmyelinated I II III IV Aα 1212-20 µm 7272-120 m/sec Aβ 6-12 µm 3636-72 m/sec Aδ 1-6 µm 4-36 m/sec C 0.20.2-1.5 µm 0.40.4-2.0 m/sec University of Pé Pécs, cs, Department of Neurology SOMATOSENSORY PATHWAYS • Dorsal Column-Medial lemniscal system Discriminative touch Vibratory sense Limb and joint position information • Anterolateral system Pain Temperature Crude touch University of Pé Pécs, cs, Department of Neurology DORSAL COLUMN – MEDIAL LEMNISCAL SYSTEM • Primary afferents ascend to the medulla on the ipsilateral side of the cord in the posterior columns • Secondary afferents cross in the medulla and ascend as the medial lemniscus • In the thalamus they synapse in the VPL (ventroposterior lateral nucleus) and ascend to the cortex University of Pé Pécs, cs, Department of Neurology ANTEROLATERAL SYSTEM • Primary afferents enter the cord laterally and synapse in the dorsal horn • The secondary afferents cross to the opposite side of the spinal cord and ascend in the spinothalamic tract • The spinothalamic tract enters enters the VPL of the thalamus, thalamus, synapses and is finally carried to cortex by the thalamocortical neurons University of Pé Pécs, cs, Department of Neurology ANTEROLATERAL SYSTEM Lissauer`s tract Pain afferents travel one or two segments up or down the cord before synapsing. synapsing. Lissauer's tract is the tract carrying these migrating axons, axons, but they are only in the tract for a short time. time. Within one or two levels, levels, they enter the dorsal horn and synapse. synapse. University of Pé Pécs, cs, Department of Neurology ANTEROLATERAL SYSTEM The dorsal horn is a multimulti-layered structure. structure. The thin outermost layer is called the posterior marginalis layer. layer. The wide pale second layer is called the substantia gelatinosa, and the layer deep to that is called the the nucleus proprius. roprius. University of Pé Pécs, cs, Department of Neurology ANTEROLATERAL SYSTEM The two types of pain fibers enter different layers of the dorsal dorsal horn. Aδ fibers enter the posterior marginalis and the nucleus proprius, and synapse on a second set of neurons. The C fibers enter the substantia substantia gelatinosa and synapse, but they do not synapse on secondary afferents. afferents. Instead they synapse on interneurons - neurons which do not project out of the immediate area. The interneurons must carry the signal signal to the secondary afferents in either the posterior marginalis or the nucleus nucleus proprius. University of Pé Pécs, cs, Department of Neurology INTERRUPTION OF SENSORY PATHWAYS Hemispheric lesion: Contralateral side of the body University of Pé Pécs, cs, Department of Neurology INTERRUPTION OF SENSORY PATHWAYS Brainstem: Alternate syndromes University of Pé Pécs, cs, Department of Neurology INTERRUPTION OF SENSORY PATHWAYS Spinal cord: Segmental University of Pé Pécs, cs, Department of Neurology INTERRUPTION OF SENSORY PATHWAYS Peripheral: Root, Root, plexus plexus or peripheral nerve University of Pé Pécs, cs, Department of Neurology PAIN AND NOCICEPTION • Pain is a subjective experience that accompanies nociception, but can also arise without any stimuli. It includes the emotional response. • Nociception is a neurophysiologic term and denotes the activity in the nerve pathways. These pathways transmit the unpleasant signals that are not always painful. • Pain is a critical component of the body's defense system • Cognitive and emotional factors might dramatically influence painful sensations • According to WHO one human being out of five suffers from chronic pain University of Pé Pécs, cs, Department of Neurology PAIN AND NOCICEPTION • Pain is a subjective experience that accompanies nociception, but can also arise without any stimuli. It includes the emotional response. • Nociception is a neurophysiologic term and denotes the activity in the nerve pathways. These pathways transmit the unpleasant signals that are not always painful. • Pain is a critical component of the body's defense system • Cognitive and emotional factors might dramatically influence painful sensations • According to WHO one human being out of five suffers from chronic pain University of Pé Pécs, cs, Department of Neurology NOCICEPTION • Nociceptors are the free nerve endings of neurons that have their cell bodies outside the spinal column in the dorsal root ganglion • When the nociceptors are stimulated, they transmit signals through sensory neurons in the spinal cord • Signals release glutamate, an exicitory neurotransmitter that relays signals from one neuron to another and ultimately to the thalamus, in which pain perception occurs • From the thalamus, the signal travels to the cerebrum, at which point the individual becomes fully aware of the pain University of Pé Pécs, cs, Department of Neurology ANATOMY AND PHYSIOLOGY OF PAIN – Neurotransmission by C neurons involves substance P – A-δ transmitters at terminals: glutamate, aspartate, adenosin triphosphate – Opiates (receptors in lamina II) decreases substance P and lamina II neurons release enkephalins, endorphins and dynorphins University of Pé Pécs, cs, Department of Neurology ANATOMY AND PHYSIOLOGY OF PAIN Spinal afferent tracts – Lateral spinothalamic tract (fast conducting pathway) via anterior comissure, termination in brainstem and thalamic structures – Medial spinothalamic tract; paleospinothalamic pathway (slow-conducting multineuron system), mediates poorly localized pain from deep somatic and visceral structures. Connections to medulla, parabrachial region, midbrain reticular formation and hypothalamus University of Pé Pécs, cs, Department of Neurology ANATOMY AND PHYSIOLOGY OF PAIN Thalamic terminus and thalamocortical projections – Lateral division terminates in the ventrobasal and posterior groups of nuclei; projections to the primary sensory cortex and Sylvian fissure – Medial divisions terminates in the intralaminar complex; projections to hypothalamus, amygdaloid nuclei and limbic cortex (arousal and autonomic responses) – Paleospinothalamic fibers project onto the medial intralaminar nuclei; cortical projection is not well known University of Pé Pécs, cs, Department of Neurology DESCENDING PAIN-MODULATING SYSTEMS – – – – Projections from the frontal cortex and hypothalamus to the periaqueductal region of the midbrain and medulla From the medulla it descends to the lateral funiculus and posterior horn Modulate activity of nociceptive pathways Other descending pathways (serotoninergic, noradrenergic) project to locus ceruleus, dorsal raphe nucleus University of Pé Pécs, cs, Department of Neurology DESCENDING PAIN-MODULATING SYSTEMS Opiate interneurons in the spinal cord can be activated by descending descending projections from the brainstem (especially the raphe nuclei and periaqueductal grey), and can block pain transmission at two sites. 1., 1., They can prevent the primary afferent from passing on its signal by blocking neurotransmitter neurotransmitter release, and 2., 2., they can inhibit the secondary afferent so it does not send the signal up the spinothalamic tract. University of Pé Pécs, cs, Department of Neurology PAIN THRESHOLD • The threshold for perception of pain is approximately the same in all person • It is lowered by inflammation (sensitization) • It is raised by local anesthetics, certain lesions of the nervous system and centrally acting analgesic drugs University of Pé Pécs, cs, Department of Neurology DIFFERENT TYPES OF PAIN • Acute pain is defined as short-term pain or pain with an easily identifiable cause • Chronic pain is medically defined as pain that has lasted 6 months or longer • Cutaneous pain is caused by injury to the skin or superficial tissues • Somatic pain originates from ligaments, tendons, bones, blood vessels, and even nerves themselves • Visceral pain originates from body organs • Phantom limb pain is the sensation of pain from a limb that one no longer has • Neuropathic pain can occur as a result of injury or disease to the nerve tissue itself University of Pé Pécs, cs, Department of Neurology DIFFERENT PAIN TYPES • Skin pain: fast pain is transmitted by A-δ fibers, slow and longer-lasting pain is transmitted by C fibers • Deep pain: visceral and skeletomuscular structures; sharp, penetrating and burning type (e.g. heartburn and angina pectoris) • Referred pain: deep pain projects fix site University of Pé Pécs, cs, Department of Neurology PAIN INTENSITY fast pain longerlonger-lasting pain Intensity Time University of Pé Pécs, cs, Department of Neurology REFERRED PAIN Diaphragm C4 Heart T3T3-4 Esophagus T4T4-5 Stomach T6T6-9 Liver, gallbladder T8T8-11 Small intestines T10T10-L1 Large intestines T11T11-L1 Kidney, testicles T10T10-L1 Urinary bladder T11T11-L1 University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Peripheral nerve pain (neuropathic, neurogenic) – Pain arises from direct stimulation of nervous tissue, pain is due to stimulation of sensitized C fibers – Mono and polyneuropathies – Plexus lesion – Trigeminal neuralgia – Root irritation – Herpes zoster – Deafferentation pain – Reflex sympathetic distrophy – Fibromyalgia University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Carpal tunnel syndrome (mononeuropathy) University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Carpal tunnel syndrome • Due to excessive use of hand • Dysesthesias and pain in the fingers • Paresthesias are worse during the night • Pain radiates into the forearm • Sensory loss, atrophy, motor weakness University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Polyneuropathy: similar symptoms, different etiology PAIN DISORDERS Brachial plexus neuritis (Parsonage-Turner syndrome) – The illness develops abruptly in healthy individuals – Shoulder and neck ache – Pain becomes rapidly more severe – After a period of 5 to 14 days there is a rapid development of muscular weakness, sensory and reflex impairment – Atrophy – CMV infection, AIDS, Coxsackie virus, vaccines University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Low-back pain - Local pain: periosteum, capsule of apophyseal joints, muscles, ligaments, annulus fibrosus - Referred pain: projected from the spine to viscera - Radicular or root pain: distal radiation to the territory of root - Pain secondary to muscle spasm University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Normal Abnormal Disc degeneration University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS L5 disc: axial view S1 root irritation University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Herpes zoster: • segmental distribution of rash • inflammatory reaction in cranial or spinal sensory ganglia (root) • radicular pain • varicella zoster virus University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Central pain – Spinal cord lesion: intolerable pain below the level of lesion; deafferentation of secondary neurons in the posterior horns or of sensory ganglion cells; deafferented cells become continuously active – Thalamic pain syndrome (Déjerine-Roussy) and parietal lobe infarction (Schmahmann and Leifer), lateral medullary and pons lesion: intractable pain; loss of descending inhibitory systems and/or altered sensitivity and hyperactivity of central neurons University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Primary headaches – Migraine: trigeminovascular headache – Cluster: trigemino-autonomic headache – Tension headache: contraction of craniocervical muscles University of Pé Pécs, cs, Department of Neurology PAIN DISORDERS Secondary headache - Headaches related to medical diseases - Pain-sensitive cranial structures: 1. Skin, subcutaneus tissue, muscles, extracranial arteries, periosteum of the skull 2. Delicate structures of eye, ear, nasal cavities, sinuses 3. Intracranial venous sinuses 4. Parts of dura and intracranial arteries 5. Optic, oculomotor, oculomotor, trigeminal, trigeminal, glossopharyngeal, glossopharyngeal, vagus, vagus, first three cervical nerves University of Pé Pécs, cs, Department of Neurology ANEURYSM RUPTURE University of Pé Pécs, cs, Department of Neurology SINUS THROMBOSIS University of Pé Pécs, cs, Department of Neurology BRAIN TUMOR University of Pé Pécs, cs, Department of Neurology THERAPY OF PAIN • (specific treatment) • Nonopioid analgesics: e.g. Acetylsalicylic acid, Indomethacin, Naproxen • Narcotic analgesics: e.g. Codeine, Morphine, Fentanyl • Anticonvulsants: e.g. Carbamazepine, Gabapentin, Pregabalin • Tricyclic and SSRI antidepressants: e.g. Amitriptylin, Sertaline • Anesthetics: e.g. Lidocaine, Mexiletine • Root blocks, epidural injection, ganglion infiltration • Ablative surgery: rhizotomy, spinothalamic tractotomy, bilateral cordotomy, stereotactic surgery on the thalamus • Spinal cord stimulation, deep brain stimulation • Other treatments: biofeedback, acupuncture, transcutaneous electrical stimulation University of Pé Pécs, cs, Department of Neurology