* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Ch. 20-Drugs Used to Treat Dysrhythmias
Survey
Document related concepts
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
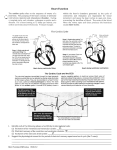
Chapter 20 Drugs Used to Treat Dysrhythmias •the heart pumps blood to itself through coronary arteries and to the rest of the body’s tissues •there are 2 phases of heart action: •diastole: resting phase, heart chambers fill with blood, heart is relaxed in this phase •systole: working phase, heart contracts, blood is pumped through the vessels when the heart contracts •systole and diastole make up the cardiac cycle •the conduction system (electrical system) controls the cardiac cycle •heart muscle must relax and fill with blood and contract to pump blood, in a coordinated fashion. Otherwise cells do not get enough blood and oxygen •to coordinate the cardiac cycle the heart’s muscle fibers are linked together •an electrical impulse starts in wall of right atrium, it’s conducted to muscles fibers in right and left atria, causing the atria to contract. Then the impulse moves to the ventricles, and causes them to contract •for every heartbeat an electrical impulse is conducted through the heart 4 structures in the heart wall make up the conduction system (see fig. 20-1 pg. 256): •sino-atrial node (SA node) •atrio-ventricular node (AV node) •atrio-ventricular bundle (AV bundle aka bundle of His) •purkinje fibers •SA node: starts the impulse in the right atrium, its also called the pace-maker. It sets the beat of the heart •the electrical impulse travels from the SA node to the right and left atria •the right and left atria contract as the impulse travels through them. Blood pumps to ventricles •electrical impulse reaches AV node, it is at the bottom of the right atrium near the right ventricle •the impulse travels through the AV node to the AV bundle, aka bundle of His, in the wall separating the right and left ventricles •AV bundle has right and left branches, they extend to all parts of the ventricular wall •the right bundle branch conducts the impulse to the right ventricle •left bundle branch conducts the impulse to the left ventricle •Purkinje fibers branch into the myocardium from the right and left bundle branches •when impulse reaches the ventricular muscle, the ventricles contract •after contracting the ventricles relax •arrhythmia: without rhythm •dysrhythmia: an abnormal rhythm •there is a disturbance in the normal electrical conduction causing: •an abnormal heart muscle contraction •an abnormal heart rate •areas outside the SA node can act as a pacemaker, this causes an irregular heart beat •some rhythms are life-threatening •blocks can occur in the conduction system, block prevents impulse from traveling in a normal manner, can be lifethreatening •electrocardiograms (ECGs): record the electrical activity of the conduction system •this is recorded in waves •waves give the cardiac cycle a distinct appearance •each wave represents electrical activity in a certain part of the heart •the P wave, QRS complex, and T wave are the major parts of cardiac cycle •if a problem occurs in a part of the conduction system, the wave for that part appears abnormal •by studying ECG doctor determines the site of problem in the conduction system or the area of heart muscle damage •see fig. 20-2 pg. 257 Types of Dysrhythmias: •normal sinus rhythm impulses start in SA node •the heart rate is between 60-100 beats per minute •various heart disease cause changes in conduction system •dysrhythmias are classified by origins within the heart tissues Supraventricular dysthythmias: these develop above the bundle of His: •Sinus tachycardia: heart rate is rapid, Impulses start in SA node (fig 20-4 p. 258) •Sinus bradycardia: heart rate is slow, impulses start in SA node (fig 20-5) •Premature atrial contraction (PAC): SA node sends out impulse early (fig 20-6) •Paroxysmal atrial tachycardia (PAT): normal rhythm that suddenly turns into tachycardia. Bursts(paroxysms) of tachycardia occur. The tachycardia stops suddenly. (fig 20-7) supraventricular dysrhythmias cont… •atrial flutter: impulses start in the atria at a rapid rate -ventricles do NOT respond to every impulse (fig 20-8), -more P waves than QRS complexes -QRS complexes occur at regular impulses -persons pulse is regular •atrial fibrillation: impulses start in atria at multiple sites -no P waves -Impulses are conducted to the ventricles at irregular intervals (fig 20-9) -pulse is irregular. -Atria quiver, not contract -Blood not pumped from atria to ventricles in normal amounts, thus inadequate blood pumped to rest of body •junctional rhythms: impulses start in the AV node, there are no P waves (fig 20-10), these can occur at normal or slow rates blocks in conduction pathways: -described by degree of the block: •first-degree heart block: -impulse takes longer to travel from SA node to AV note -PR interval is longer than normal (fig 20-11) -rhythm is regular •second-degree heart block: -some impulses from SA node do not reach ventricles -Impulses from SA node take longer and longer to travel through the AV node until a beat is skipped -QRS complex does NOT follow a P wave (fig 20-12) -rhythm is irregular •third-degree heart block: -impulse is blocked between the atria and ventricles (fig 20-13) -Impulse cannot reach the ventricles -ventricles must create their own impulses -P waves appear but are not related to QRS complexes -QRS complexes are wider than normal -Heart rate is very slow -LIFE THREATENING DYSRHYTHMIA!!! Ventricular dysrhythmias: these develop below the bundle of His: •Premature ventricular contraction (PVC): -impulse created in ventricles -occurs earlier than the next regular beat -QRS complex is wide and bizarre (fig 20-14) -unifocal PVCs come from one site, all look the same -multifocal PVCs created in many sites (fig. 20-15) -bigeminy: every second complex is a PVC (fig 20-16) -trigeminy: every third complex is a PVC -two PVCs can occur in a row (fig 20-17) -they can be unifocal or multifocal, called coupled PVCs -a run of ventricular tachycardia is several PVCs in a row (fig 20-18) rhythm returns to normal -PVCs can mean heart muscle is irritable -LIFE THREATENING!!! Ventricular dysrhythmias cont…. Ventricular tachycardia (VT): -impulses start in ventricles -heart rate can change from 40-250 beats per minute -QRS complexes are wide and bizarre -rhythm looks like a series of PVCs (fig 20-19) -LIFE THREATENING!!! -if not corrected it progresses to ventricular fibrillation Ventricular fibrillation (VF or V fib): -impulses start from multiple sites in ventricles -P waves and QRS complexes are not present (fig 20-20) -ventricles quiver, not contract -DEADLY!!! person is in cardiac arrest Asystole: -means no contraction -no electrical action occurs in heart (fig 20-21) -DEADLY!!! person in cardiac arrest •conduction system tissues are affected by calcium and sodium •ion is atom with electrical charge •atom is smallest part of an element •element is a simple substance that cannot be broken down into another substance •calcium and sodium are elements: -calcium: SA and AV nodes depend on calcium ions for electrical conduction -sodium: atrial muscle, His-Purkinje system, and ventricular muscle depend on sodium for contraction Drug Therapy for Dysrhythmias: •Anti-dysrhythmic agents are drugs used to prevent or correct abnormal heart rhythms •depending on drug, anti-dysrhythmic agents affect the heart’s conduction system by: -inhibiting sodium ion movement, this depresses the heart muscle -prolonging or shortening the duration of electrical stimulation on the cells -increasing or decreasing the time between electrical impulses -slowing the conduction rate between the atria and ventricles Delegation Guidelines Drug Therapy for Dysrhythmias: Some drugs used to treat dysrhythmias are given parenterally- by intramuscular or intravenous injection. Because you do NOT give parenteral dose forms, they are not included in this chapter. Should a nurse delegate the administration of such to you, you must: - remember that parenteral dosages are often very different from dosages other routes -Refuse the delegation. Make sure to explain why. Do NOT just ignore the request. Make sure the nurse knows that you cannot give drug and why Drug therapy for Dysrhythmias amiodarone hydrochloride (Cordarone): -slows the rate of electrical conduction, increases the time between contractions -drug is given to convert the following dysrhythmias to normal sinus rhythm: - supraventricular tachycardias – rapid arrhythmias that occur above the bundle of His - atrial fibrillation - atrial flutter - bradycardia-tachycardia syndromes - ventricular tachycardia - ventricular fibrillation Drug therapy for Dysrhythmias cont… Assisting With the Nursing Process amiodarone hydrochloride (Cordarone): ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (for 1 min), and respirations PLANNING: oral dose forms are: 100, 200, 400mg tablets IMPLEMENTATION: initial adult dose is 800-1600mg daily in divided doses for 1-3 weeks. Then a dosage of 600-800mg is given for about 1 month, lowest effective dose should be used (usually 400mg) EVALUATION: report and record: -fatigue, tremors, involuntary muscle movements, sleep problems, numbness and tingling, coordination problems, dizziness, confusion. Many of these resolve when dose is reduced or drug is discontinued, provide for safety -dyspnea on exertion, non-productive cough, chest pain with breathing: symptoms resolve when drug is discontinued -blurred vision, narrowed peripheral vision, halos: provide for safety, resolve when drug is discontinued - nausea, vomiting, constipation, abdominal pain, anorexia: common with high dosages, resolve with lower dosages or divided doses -dysrhythmias: drug may cause dysrhythmias or cause existing ones to worsen -skin reactions: rash, burning, tingling, redness, blistering: from exposure to sun (photosensitivity). person should wear sunscreen, long sleeved shirts, avoid exposure to sun -anorexia, nausea, vomiting, jaundice: may signal liver toxicity Drug therapy for Dysrhythmias cont… -Beta blockers are widely used as anti-dysrhythmic agents (ch.14) -by blocking beta receptors, they block the heart’s response to sympathetic nerve stimulation -heart rate, BP and cardiac output are reduced -see table 14-2 for beta blockers used to treat dysrhythmias -they are effective in converting the following dysrhythmias to normal sinus rhythm: •various ventricular dysrhythmias •sinus tachycardia •paroxysmal supraventricular tachycardia •premature ventricular contractions •atrial flutter when tachycardia is present •atrial fibrillation when tachycardia is present Drug therapy for Dysrhythmias cont… Assisting With the Nursing Process for beta blockers: See chapter 14 Drug Therapy for Dysrhythmias cont… Disopyramide (Norpace): -Prolongs the simulation on the cells and increases the time between electrical impulses -Effective in converting the following dysrhythmias to normal sinus rhythm: -atrial fibrillation -paroxysmal supraventricular tachycardia -runs of ventricular tachycardia -ventricular tachycardia Drug therapy for Dysrhythmias Assisting With the Nursing Process disopyramide (Norpace): ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (1 min) and respirations, ask about bowel elimination and urination PLANNING: oral dose form: 100, 150mg tablets 100, 150mg extended release capsules IMPLEMENTATION: dosage depends on person needs, usually 400800mg/day, usually 150mg every 6 hours EVALUATION: report and record: - dry mouth, nose and throat: provide oral hygiene, give, hard candy or ice chips if care plan allows -bradycardia, signs of heart failure(ch. 21): signs of myocardial toxicity -difficulty starting a urine stream: run tap water or immerse hand in water, measure input/output -constipation, abdominal distention, flatus: ask about bowel elimination and expelling gas Drug therapy for Dysrhythmias cont… flecainide acetate (Tambocor): -slows conduction rate through atria and ventricles -effective in converting the following dysrhythmias to normal sinus rhythm: -ventricular tachycardia -paroxysmal supraventricular tachycardia -premature ventricular contractions Drug therapy for Dysrhythmias Assisting With the Nursing Process flecainide acetate (tambocor): ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (1 min) and respirations, observe for signs and symptoms of heart failure (ch.21) PLANNING: oral dose forms: 50, 100, 150 mg tablets IMPLEMENTATION: initial dose is 100mg every 12 hours, increased by 50mg twice a day every 4 days. Usual dose is 150mg 2x/day, max daily dose is 400mg EVALUATION: report and record: -dizziness, headache, constipation, nausea: mild, tend -vision to resolve disturbances: provide for safety -signs and symptoms of heart failure (ch 21), may cause heart failure or existing heart failure to worsen -dysrhythmias: may cause or worsen dysrhytmias Drug therapy for Dysrhythmias cont… mexiletine (Mexitil): •shortens the duration of electrical stimulation on the cells •increases the time between electrical impulses •effective in converting the following dysrhythmias to normal sinus rhythm: •ventricular tachycardia •premature ventricular contractions Drug therapy for Dysrhythmias cont… Assisting With the Nursing Process mexiletine (Mexitil): ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (1 min) and respirations, ask about GI symptoms, observe orientation to person, time and place. Observe for agitation PLANNING: oral dose forms: 150, 200, 250mg tablets IMPLEMENTATION: usual dose is 200-400mg every 8 hours, give drug with food or antacids, if ordered EVALUATION: report and record: -nausea, vomiting, indigestion: occur -dysrhythmias: may -fine usually with higher doses cause them or worsen existing ones hand tremors, coordination problems, light-headedness, blurred vision, double vision, involuntary eye movement, difficult speech, confusion, numbness and tingling, drowsiness, seizures: signal toxic effect on CNS -confusion: observe for confusion and persons orientation to person, time and place, provide for safety Drug therapy for Dysrhythmias cont… moricizine (Ethmozine): •slows the conduction rate between atria and ventricles •effective in converting ventricular dysrhythmias to normal sinus rhythm •it can cause other dysrhythmias, it is used when benefits are greater than the risk Drug therapy for Dysrhythmias cont… Assisting With the Nursing Process moricizine (Ethmozine): ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (1 min) and respirations, ask about GI symptoms, observe orientation to person, time and place. Observe for agitation and confusion PLANNING: oral dose forms: 200, 250, 300mg tablets IMPLEMENTATION: initial dose is 200mg every 8 hours, may be increased by 150mg every 3 days. usual dosage is between 600900mg/day, given in divided doses around the clock, give drug with food and milk EVALUATION: report and record: -hypotension, dizziness: may occur with starting drug, usually subside, provide for safety -nausea: give drug with food or milk -dysrhythmias: may cause them or worsen existing -euphoria, confusion: observe orientation to person time and place, provide for safety Drug therapy for Dysrhythmias cont… procainamide hydrochloride (Procanbid): prolongs the duration of electrical stimulation on the cells increases the time between electrical impulses effective in converting the following dysrhythmias to normal sinus rhythm: ◦ ◦ ◦ ◦ ventricular dysrhythmias supraventricular dysrhythmias atrial flutter atrial fibrillation Drug therapy for Dysrhythmias cont… Assisting With the Nursing Process procainamide hydrochloride (Procanbid): ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (1 min) and respirations PLANNING: oral dose forms: 250, 375, 500mg capsules/tablet and 250, 500, 750, 1000mg sustained-release tablets IMPLEMENTATION: initial dose is 1-1.25g, followed with 750mg one hour later if arrhythmia is still present, dosage is maintained at 0.5-1g every 4-6 hours (some every 3-4), given in divided doses around the clock, give with food or milk EVALUATION: report and record: -drowsiness, sedation, dizziness, hypotension: provide for safety - fever, chills, joint and muscle pain, skin eruptions: may signal changes in white blood cells Drug therapy for Dysrhythmias cont… propafenone (Rythmol): slows the conduction rate between the atria and ventricles effective in converting atrial fibrillation and ventricular dysrhythmias to normal sinus rhythm it can cause other dysrhythmias so it is used when benefits are greater than risks Drug therapy for Dysrhythmias cont… Assisting With the Nursing Process propafenone (Rhythmol): ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (1 min) and respirations, ask about GI symptoms PLANNING: oral dose forms: 150, 225, 300mg tablets and 225, 325 and 425 extended-release tablets IMPLEMENTATION: initial dose is 150mg every 8 hours, every 3-4 days dosage may be increased to 225mg every 8 hours, then 300mg every 8 hours (900mg daily), drug is given around the clock, ask nurse what to do if a dose is missed EVALUATION: report and record: - dizziness: provide for safety - nausea, vomiting, constipation: give drug with food or milk - dysrhythmias: drug may cause them or worsen existing Drug therapy for Dysrhythmias cont… quinidine: shortens the duration of electrical stimulation on the cells increases the time between electrical impulses slows the heart rate and changes a rapid, irregular pulse to a slow, regular pulse it is effective in converting the following dysrhythmias to normal sinus rhythm: ◦ ◦ ◦ ◦ atrial flutter atrial fibrillation paroxysmal supraventricular tachycardia premature ventricular contractions Drug therapy for Dysrhythmias cont… Assisting With the Nursing Process quinidine: ASSESSMENT: observe for dyspnea, chest pain, fatigue, edema, fainting, palpitations (person says “heart skips beats” or “my heart is racing”), measure BP, apical pulse (1 min) and respirations, ask about bowel elimination PLANNING: oral dose forms for quinidine sulfate: 200, 300mg tablets and 300mg sustained-release tablets quinidine gluconate: 324mg sustained-release tablets IMPLEMENTATION: quinidine sulfate: 200-400mg orally 3-5x/day, max single dose is 600-800mg, give with food/milk quinidine gluconate: 324-972mg every 8-12 hours EVALUATION: report and record: - diarrhea: common with start of drug, usually subsides - dizziness, faintness: usually subside, provide for safety - hearing loss, headache, tinnitus, increasing mental confusion, rash, chills, fever: result from excess quinidine - hypotension: may occur if person is also on diuretics or anti-hypertensive meds, provide for safety