* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Presentation
Survey
Document related concepts
Transcript
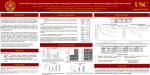
Personalized Health Care and Cancer Therapeutics (Biomarkers and Treatment) April 17,, 2011 Dr Howard L. McLeod Eshelman Distinguished Professor and Director Institute for Pharmacogenomics and Individualized Therapy (IPIT) University of North Carolina – Chapel Hill, NC “A surgeon who uses the wrong side of the scalpel cuts her own fingers and not the patient; if the same applied to drugs they would have been investigated very carefully a long time ago” Rudolph Bucheim Beitrage zur Arzneimittellehre, 1849 Personalized medicine, schmersonalized medicine! Medicine has always been personalized Medicine is moving toward greater 'customer accountability' Medicine will never be personalized it is a change in expectation as well as some practical, process changes Drivers of Personalized Medicine Technology – Significant new opportunities over the past 5 years Patient financial burden – When you are paying more, you want more say Less personal care – Who will be my 'doctor' today? Cost of care – Even the USA can't afford treating 100% to benefit 20% Preemptive action is a clinical major weapon Drug interactions Renal dysfunction Age Vaccination Antimalarial TB Mammography colonoscopy The clinical problem •Multiple active regimens for the treatment of most diseases •Variation in response to therapy •Unpredictable toxicity $$$$$$$$$$$$$ With choice comes decision Pharmacogenomic examples-2011 • • • • • • • • • • • bcr/abl or 9:22 translocation—imatinib mesylate* HER2-neu—trastuzumab** C-kit mutations—imatinib mesylate** Epidermal growth factor receptor mutations—gefitinib Thiopurine S-methyltransferase—mercaptopurine and azathioprine* UGT1A1-irinotecan** CYP2D9/VKORC1-warfarin* HLA-B*5701-abacavir * HLA-B*1502-carbamazepine * CYP2C19-clopidogrel Cytochrome P-450 (CYP) 2D6—5-HT3 receptor antagonists, antidepressants, ADHD drugs, and codeine derivatives, tamoxifen* What needs to be done to determine hope vs hype? •Find the 'right' biomarkers •Validate in robust datasets •Apply them! We do not know very much about drugs Irinotecan cell membrane ABCB1 ???? ???? Irinotecan CES1 Irinotecan CES2 CES1 CYP3A4 APC CYP3A5 NPC ???? CES2 ???? SN-38 SN-38 ???? ???? ???? ???? SN-38 ???? SN-38G ???? ???? TOP1 ???? ???? ???? ADPRT ???? TDP1 XRCC1 ???? ???? ???? NFKB1 CDC45L ???? Cell Death 4 Grade 3 2 1 DB A/ 2 CB J A/ J PL AK /J NO R/J D BA /LtJ LB / SW 2J R/ C5 J 7L R /J NZ IIIS B/ /J B1 NJ A/ J 0 HapMap Linkage Model systems Expression array Discovery Strategies cases controls Association What needs to be done to determine hope vs hype? •Find the 'right' biomarkers •Validate in robust datasets •Apply them! Correlative science: business as usual Phase I Phase II Phase III In vivo Mechanism Biomarker assessment Biomarker validation 2011 Estimated US Cancer Cases* C90401; n=1020 Prostate 33% Lung and bronchus C30502; n=270 13% Colon and rectum Men 710,040 Women 662,870 10% 7% Melanoma of skin 5% Non-Hodgkin 4% 3% Leukemia C10105; MDS 3% Oral Cavity 3% Pancreas 2% C80303; n=528 All Other Sites Lung and bronchus C30502; n=270 11% Colon and rectum Uterine corpus C80203/80405; n=2200 4% Non-Hodgkin lymphoma 4% Melanoma of skin C50303; n=430 3% C50303; n=430 lymphoma Kidney 12% 6% C80203/80405; n=2200 Urinary bladder C40101; n=4646 Breast 32% Ovary 3% Thyroid 2% Urinary bladder 2% Pancreas 21% All Other Sites C80303; n=528 17% C80101 gastric; n=800 *Excludes basal and squamous cell skin cancers and in situ carcinomas except urinary bladder. Source: American Cancer Society, 2005. GWAS x 2 GWAS 2010 Estimated US Cancer Cases* NextGEN C90401; n=1020 Prostate 33% GWAS Lung and bronchus C30502; n=270 13% Colon and rectum Men 710,040 Women 662,870 10% 7% Melanoma of skin 5% Non-Hodgkin 4% 3% Leukemia C10105; MDS 3% Oral Cavity 3% Pancreas 2% GWAS C80303; n=528 All Other Sites Lung and bronchus C30502; n=270 11% Colon and rectum Uterine corpus C80203/80405; n=2200 4% Non-Hodgkin lymphoma 4% Melanoma of skin C50303; n=430 3% C50303; n=430 lymphoma Kidney 12% 6% C80203/80405; n=2200 Urinary bladder C40101; n=4646 Breast 32% Ovary 3% Thyroid 2% Urinary bladder 2% Pancreas 21% All Other Sites C80303; n=528 17% C80101 gastric; n=800 *Excludes basal and squamous cell skin cancers and in situ carcinomas except urinary bladder. Source: American Cancer Society, 2005. What needs to be done to determine hope vs hype? •Find the 'right' biomarkers •Validate in robust datasets •Apply them! Fundamental questions When is surgery enough? Should we use chemotherapy? difficult to reverse practice Which treatment should we use? toxicity-many 'equal' therapies efficacy dosage When should we use chemotherapy? Tumor tissue DNA Chip Analysis “Gene signature” Single value on “Gene signature” Relapse Hazard Score Assay result: • low- or high- risk group • probability of distant relapse 1.0 Prediction of disease recurrence after surgery in Stage II colon cancer 0.6 Good prognosis 0.4 N = 16 0.2 Poor prognosis P-value = 0.0001 0.0 Distant Relapse-free Survival 0.8 N = 20 0 20 40 Time (months) 60 80 patients with stage II disease Treat with therapy Watch and wait Not Predisposed to relapse Development and Validation of a Multi-Gene RT-PCR Colon Cancer Assay Colon Cancer Technical Feasibility • NSABP and CCF Collaborations 761 genes studied in 1,851 patients to select genes which predict recurrence and/or differential 5FU/LV benefit • Clinical Validation of final assay in a large, prospectively-designed independent study Development Studies Surgery Alone Development Studies Surgery + 5FU/LV NSABP C-01/C-02 (n=270) NSABP C-04 (n=308) CCF (n = 765) NSABP C-06 (n=508) Selection of Final Gene List & Algorithm Validation of Analytical Methods Clinical Validation Study – Stage II Colon Cancer QUASAR (n=1,436) Test Prognosis and Treatment Benefit QUASAR RESULTS: Colon Cancer Recurrence Score Predicts Recurrence Following Surgery Prospectively-Defined Primary Analysis in Stage II Colon Cancer (n=711) RECURRENCE SCORE STROMAL FAP INHBA BGN CELL CYCLE Ki-67 c-MYC MYBL2 GADD45B REFERENCE ATP5E GPX1 PGK1 UBB VDAC2 Risk of recurrence at 3 years Calculated from Tumor Gene Expression 35% Group Risk (by Kaplan-Meier) 22% 12% 18% 30% 25% 20% 15% 10% p=0.004 5% 0% 0 10 20 30 40 50 Recurrence Score 60 70 Fundamental questions When is surgery enough? Should we use chemotherapy? difficult to reverse practice Which treatment should we use? toxicity-many 'equal' therapies efficacy dosage The Epidermal Growth Factor Receptor Pathway Shc Grb2 PI3-K Sos-1 Ras AKT MEKK-1 Raf MEK mTOR MKK-7 ERK JNK Apoptosis Resistance Proliferation Angiogenesis Metastasis Retrospective studies supporting K-ras and lack of anti-EGFR response Single agent panitumumab: N=208 K-Ras Mutation Wild-Type K-Ras Panitumumab registration trial Amado RG, et al. J Clin Oncol. 2008;26:1626-1634. Mutations aplenty! Your patient with stage III sigmoid mucin neg adenocarcinoma has mutations in KRAS, BRAF, FGFR3, and CDK4 WHAT DO YOU DO? Patient biology Lymph node status Tumor biology Cancer Outcome Distant metastasis Surgical technique Access to care Comprehensive optimization of patient care Disease Genotypes Infection Defense Genotypes Toxicity-risk Genotypes Supportive Care Genotypes