Ventricular Assist Devices - cardiac anesthesia basics
... • Allows flows exceeding 10 liters • Need CPB for placement • BSA requirement…greater than 1.7 • Patients are able to go home • Minimal anti-coagulation • High cost ...
... • Allows flows exceeding 10 liters • Need CPB for placement • BSA requirement…greater than 1.7 • Patients are able to go home • Minimal anti-coagulation • High cost ...
Physiology, Health & Exercise
... Strengthened cardiac muscle- capable of more forceful contraction- higher SV- even at rest Athlete’s heart actually gets bigger- cardiac hypertrophy Increase in protein synthesis in cardiac muscle fibres increase in contractile elements within each fibre increase in size ...
... Strengthened cardiac muscle- capable of more forceful contraction- higher SV- even at rest Athlete’s heart actually gets bigger- cardiac hypertrophy Increase in protein synthesis in cardiac muscle fibres increase in contractile elements within each fibre increase in size ...
Background: Mitral regurgitation is the most prevalent heart valve
... was correlated with younger age (p=0.04) but not gender (p=0.7). There was no significant association between PTSD and objective measurements of MR severity (effective regurgitant orifice, MR volume, all p>0.6) or MR consequences. PTSD was strongly associated with subjective manifestations of MR: pr ...
... was correlated with younger age (p=0.04) but not gender (p=0.7). There was no significant association between PTSD and objective measurements of MR severity (effective regurgitant orifice, MR volume, all p>0.6) or MR consequences. PTSD was strongly associated with subjective manifestations of MR: pr ...
Managing Chronic Heart Failure
... Class III: Marked limitations of physical activity, but asymptomatic at rest. Less-than-ordinary physical activity causes fatigue, palpitations, dyspnea, or anginal pain. Class IV: Patient unable to perform physical activity without discomfort, may have symptoms at rest. This patient will be conside ...
... Class III: Marked limitations of physical activity, but asymptomatic at rest. Less-than-ordinary physical activity causes fatigue, palpitations, dyspnea, or anginal pain. Class IV: Patient unable to perform physical activity without discomfort, may have symptoms at rest. This patient will be conside ...
– H F R
... decision-making, educate team members and patients when necessary, and explain the plan of care to each patient on the service. The attending and fellow will ultimately choose one of two approaches: The fellow sees all the patients on the service with the attending and HF team. The fellow sees h ...
... decision-making, educate team members and patients when necessary, and explain the plan of care to each patient on the service. The attending and fellow will ultimately choose one of two approaches: The fellow sees all the patients on the service with the attending and HF team. The fellow sees h ...
Facts About Sudden Cardiac Arrest
... return the heart to normal rhythm. Dangerous patterns may indicate ventricular fibrillation, ventricular tachycardia or less problematic supraventricular tachycardias that arise in the upper chambers of the heart. ICDs now also collect information for the physician to use in diagnosis and programmin ...
... return the heart to normal rhythm. Dangerous patterns may indicate ventricular fibrillation, ventricular tachycardia or less problematic supraventricular tachycardias that arise in the upper chambers of the heart. ICDs now also collect information for the physician to use in diagnosis and programmin ...
Clinical Review of Cardiac Resynchronization Therapy for Heart
... Clinical Review of Cardiac Resynchronization Therapy for Heart Failure Chun hwang, MD Utah Valley Regional Medical Center, Provo, UT ...
... Clinical Review of Cardiac Resynchronization Therapy for Heart Failure Chun hwang, MD Utah Valley Regional Medical Center, Provo, UT ...
BiVentricular Pacing
... control station known as the atrioventricular or AV node. After a split-second delay, the signal spreads to the ventricles by way of specialized routes called the left and right bundle branches. The bundle branches fan out in the ventricles, thereby enabling the electrical signal to stimulate both v ...
... control station known as the atrioventricular or AV node. After a split-second delay, the signal spreads to the ventricles by way of specialized routes called the left and right bundle branches. The bundle branches fan out in the ventricles, thereby enabling the electrical signal to stimulate both v ...
Open Access Echo Request Wansbeck
... Does this breathlessness COAD patient also have heart failure? Patient has had MI How impaired is the left ventricle? Is there a left ventricular aneurysm? ...
... Does this breathlessness COAD patient also have heart failure? Patient has had MI How impaired is the left ventricle? Is there a left ventricular aneurysm? ...
Ashley Powerpoint Presentation NURS457
... Wireless Transmitter Device Wirelessly transmits data from ICD Information sent to healthcare provider via secure server ...
... Wireless Transmitter Device Wirelessly transmits data from ICD Information sent to healthcare provider via secure server ...
Document
... “The concordance of the SonR signal with measurements of LVdP/dtmax suggests that this new, operatorindependent system is a reliable means of tailored optimization of CRT devices,” commented Philippe Ritter, M.D. at University Hospital, in Bordeaux, France. “Providing weekly optimization both at re ...
... “The concordance of the SonR signal with measurements of LVdP/dtmax suggests that this new, operatorindependent system is a reliable means of tailored optimization of CRT devices,” commented Philippe Ritter, M.D. at University Hospital, in Bordeaux, France. “Providing weekly optimization both at re ...
Acute Coronary Syndromes Algorithm
... Goals of Therapy in ACS Reduce the amount of myocardial necrosis that occurs in patients with MI, preserving left ventricular function and preventing heart failure Prevent major adverse cardiac events: death, nonfatal MI, and need for urgent revascularization Treat acute, life threatening compl ...
... Goals of Therapy in ACS Reduce the amount of myocardial necrosis that occurs in patients with MI, preserving left ventricular function and preventing heart failure Prevent major adverse cardiac events: death, nonfatal MI, and need for urgent revascularization Treat acute, life threatening compl ...
Cardiac Resynchronization Therapy
... Diagnosis Code(s) (if known): Please check all that apply to the individual: Request is for FDA-approved biventricular pacemaker for cardiac resynchronization therapy (CRT) Request is for a FDA-approved ICD, in combination with cardiac resynchronization therapy (CRT/ICD) (*** If checked, you must co ...
... Diagnosis Code(s) (if known): Please check all that apply to the individual: Request is for FDA-approved biventricular pacemaker for cardiac resynchronization therapy (CRT) Request is for a FDA-approved ICD, in combination with cardiac resynchronization therapy (CRT/ICD) (*** If checked, you must co ...
Cardiac Resynchronization Therapy
... Diagnosis Code(s) (if known): Please check all that apply to the individual: Request is for FDA-approved biventricular pacemaker for cardiac resynchronization therapy (CRT) Request is for a FDA-approved ICD, in combination with cardiac resynchronization therapy (CRT/ICD) (*** If checked, you must co ...
... Diagnosis Code(s) (if known): Please check all that apply to the individual: Request is for FDA-approved biventricular pacemaker for cardiac resynchronization therapy (CRT) Request is for a FDA-approved ICD, in combination with cardiac resynchronization therapy (CRT/ICD) (*** If checked, you must co ...
Percutaneous ventricular restoration in a chronic
... associated remodelling and wall stress produce an inefficient and often failing left ventricle. Fifty seven percent of patients with an anterior infarction develop heart failure one year after thrombolytic therapy for an acute MI4. Heart failure after myocardial infarction (MI) is a progressive dise ...
... associated remodelling and wall stress produce an inefficient and often failing left ventricle. Fifty seven percent of patients with an anterior infarction develop heart failure one year after thrombolytic therapy for an acute MI4. Heart failure after myocardial infarction (MI) is a progressive dise ...
Arrhythmogenic Right Ventricular Cardiomyopathy Arrhythmogenic
... Cardiomyopathy, is a disease of the lower chamber of the heart called the ventricle. The right ventricle is primarily affected in most cases, but it can sometimes affect both ventricles. In ARVC, the normal heart muscle tissue is replaced by fibrous or fatty tissue. This disturbs the electrical cond ...
... Cardiomyopathy, is a disease of the lower chamber of the heart called the ventricle. The right ventricle is primarily affected in most cases, but it can sometimes affect both ventricles. In ARVC, the normal heart muscle tissue is replaced by fibrous or fatty tissue. This disturbs the electrical cond ...
Cardiac Conducting System
... This ensures that the heart beats in a coordinated manner. This sequence of events is brought about by the Pacemaker (SAN) and the conducting system. ...
... This ensures that the heart beats in a coordinated manner. This sequence of events is brought about by the Pacemaker (SAN) and the conducting system. ...
Heart Failure Handout
... Compensatory Mechanisms Normal heart: If CO low, venous return will increase increasing (preload) allowing increased end diastolic volume, returning CO back to normal Mild myocardial depression: CO maintained but increased venous pressure and sinus tachycardia, this however reduces ejection fraction ...
... Compensatory Mechanisms Normal heart: If CO low, venous return will increase increasing (preload) allowing increased end diastolic volume, returning CO back to normal Mild myocardial depression: CO maintained but increased venous pressure and sinus tachycardia, this however reduces ejection fraction ...
HeartMate 3 Left Ventricular Assist System
... patient’s native heart and designed to supplement the pumping ability of the weakened heart’s left ventricle, which is responsible for pumping oxygen-rich blood from the lungs throughout the body. The device is implanted above the diaphragm, immediately next to the native heart, and is attached to t ...
... patient’s native heart and designed to supplement the pumping ability of the weakened heart’s left ventricle, which is responsible for pumping oxygen-rich blood from the lungs throughout the body. The device is implanted above the diaphragm, immediately next to the native heart, and is attached to t ...
CARDIMAX
... flow and reducing blood pressure. A long history of use has recently been confirmed in positive human clinical trials which showed safety and efficacy. ...
... flow and reducing blood pressure. A long history of use has recently been confirmed in positive human clinical trials which showed safety and efficacy. ...
PBL- Case 1: Cardiac Arrhythmias Pre
... High prevalence of CAD, CHF and valvular disease and calcification (common in older patients) puts them at higher risk of atrial fibrillation. Cardiac valvular stenosis or regurgitation caused by either rheumatic or age related degenerative changes increases left atrial pressure and results in the e ...
... High prevalence of CAD, CHF and valvular disease and calcification (common in older patients) puts them at higher risk of atrial fibrillation. Cardiac valvular stenosis or regurgitation caused by either rheumatic or age related degenerative changes increases left atrial pressure and results in the e ...
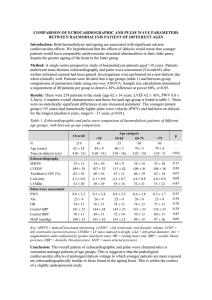
comparison of echocardiographic and pulse wave parameters
... Introduction: Both haemodialysis and ageing are associated with significant adverse cardiovascular effects. We hypothesised that the effects of dialysis would mean that younger patients would have comparable cardiovascular structural abnormalities to their older peers, despite the greater ageing of ...
... Introduction: Both haemodialysis and ageing are associated with significant adverse cardiovascular effects. We hypothesised that the effects of dialysis would mean that younger patients would have comparable cardiovascular structural abnormalities to their older peers, despite the greater ageing of ...
Cardiac contractility modulation
.jpg?width=300)
Cardiac contractility modulation (CCM) is a treatment for patients with moderate to severe left ventricular systolic heart failure (NYHA class II–IV). The short- and long-term use of this therapy enhances both the strength of ventricular contraction and the heart’s pumping capacity. The CCM mechanism is based on stimulation of the cardiac muscle by non-excitatory electrical signals (NES). CCM treatment is delivered by a pacemaker-like device that applies the NES, adjusted to and synchronized with the electrical action in the cardiac cycle.In CCM therapy, electrical stimulation is applied to the cardiac muscle during the absolute refractory period. In this phase of the cardiac cycle, electrical signals cannot trigger new cardiac muscle contractions, hence this type of stimulation is known as a non-excitatory stimulation. However, the electrical CCM signals increase the influx of calcium ions into the cardiac muscle cells (cardiomyocytes). In contrast to other electrical stimulation treatments for heart failure, such as pacemaker therapy or implantable cardioverter defibrillators (ICD), CCM does not affect the cardiac rhythm directly. Rather, the aim is to enhance the heart’s natural contraction (the native cardiac contractility) sustainably over long periods of time. Furthermore, unlike most interventions that increase cardiac contractility, CCM is not associated with an unfavorable increase in oxygen demand by the heart (measured in terms of Myocardial Oxygen Consumption or MVO2). This may be explained by the beneficial effect CCM has in improving cardiac efficiency. A meta-analysis in 2014 and an overview of device-based treatment options in heart failure in 2013 concluded that CCM treatment is safe, that it is generally beneficial to patients and that CCM treatment increases the exercise tolerance (ET) and quality of life (QoL) of patients. Furthermore, preliminary long-term survival data shows that CCM is associated with lower long-term mortality in heart failure patients when compared with expected rates among similar patients not treated with CCM.