* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diseases of Nervous system
Management of multiple sclerosis wikipedia , lookup
Transcranial Doppler wikipedia , lookup
Brain damage wikipedia , lookup
Cortical stimulation mapping wikipedia , lookup
Epilepsy-intellectual disability in females wikipedia , lookup
Hemiparesis wikipedia , lookup
History of neuroimaging wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
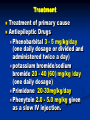
Diseases of Nervous system Definition A condition characterized by recurrent seizures (two or more) result from an abnormal and excessive neuronal discharge. epileptic seizures are a sign of cerebral dysfunction Characteristics Three main characteristics of epileptic seizures are: the loss of control (in various degrees), the episodic nature of the attacks (they start suddenly and they terminate suddenly), and the repetitive clinical pattern (attacks are identical from episode to episode). Types Localized: caused by localized area of brain dysfunction (the epileptic focus in cerebral cortex and do not spread) and symptoms are related to area involved. Generalized: The abnormal impulses originate from the cerebral cortex and spread Origin of localized epilepsy The abnormal impulses originate from a specific area of the cerebral cortex and do not spread. Origin of generalized epilepsy The abnormal impulses originate from the cerebral cortex and spread Etiology 1. 2. 3. 4. 5. 6. 7. 8. Genetics in some breeds (autosomal recessive trait ) as German shepherd and Collie Infection: distemper, toxoplasma, Head trauma and neoplasia inflammatory condition Idiopathic (unknown cause) Hypocalcemia, hypoglycemia, thiamine deficiency Renal and hepatic dysfunction Lead intoxication Clinical signs Localized motor activity e.g., tonic seizures of one leg or facial twitching autonomic signs such as pupil dilatation, salivation or vomiting Tonic seizure in limbs Dilated eye pupil - epilepsy Diagnosis 1. 2. 3. 4. Detail case history Clinical signs if appeared Lab diagnosis: 1. Urinalysis 2. Serum: hypocalcemia or hypoglycemia Radiographic: fracture, trauma or neoplasia. Treatment Treatment of primary cause Antiepileptic Drugs Phenobarbital 3 - 5 mg/kg/day (one daily dosage or divided and administered twice a day) potassium bromide/sodium bromide 20 - 40 (60) mg/kg /day (one daily dosage) Primidone 20-30mg/kg/day Phenytoin 2.0 - 5.0 mg/kg given as a slow IV injection. Definition Narcolepsy is a neurological disorder associated with abnormalities of rapid eye movement sleep with excessive daytime sleepiness Occurs sporadically in dogs and rarely, in cats cataplexy is often the dominant clinical sign, which is characterized by sudden paroxysmal attacks of flaccid paralysis (muscle atony) with conservation of consciousness, that may last from a few seconds to more than 20 minutes Etiology Imbalance between cholinergic (e.g., hyperactive) and catecholaminergic (e.g., hypoactive) neurotransmitter systems within the CNS due to diffuse encephalitis Canine distemper Genetic predisposition (recessive trait) Clinical signs 1. 2. 3. 4. 5. Rapid eye movement (REM) during sleep Excessive daytime sleeping muscular twitching, variable vocalization, facial grimacing and chewing movements. Flaccid paralysis (cataplexy) Attacks can be induced in most affected animals by exercise or eating Sudden bouts of deep sleep Diagnosis History Clinical sign Stimulation test: Give an affected dog a bone and within seconds it’s on the floor Treatment intravenous imipramine at a dose of 0.5 mg/kg. imipramine is an antidepressant act to change the balance of naturally occurring chemicals in the brain (neurotransmitters) that regulate the transmission of nerve impulses between cells Atropine sulfate: 0.1 mg/kg, IV Definition Inflammation of meninges of brain (pia, dura and arachnoid) that may involve brain (meningioencephalitis) or brain and spinal cord (meningioencephalomyelitis), characterized clinically by hyperesthesia and rigidity of the neck most affected dogs are adult, with a mean age around 5 years Etiology and pathogenesis 1. 2. 3. 4. Bacterial infections of the CNS most often occur via: hematogenous spread from distant foci within the body (e.g., lung or splenic abscess, vegetative endocarditis, pleuritis, and urinary tract infections), by direct extension from sinuses, ears and eyes, as a result of trauma, meningeal spread with entry along nerve roots, or from contaminated surgical instruments (e.g., spinal needle) Bacteria causing meningitis 1. 2. Pasteurella sp (e.g., P. multocida), Staphylococcus 1. 2. 3. 3. 4. 5. 6. aureus, Staphylococcus epidermidis, Staphylococcus albus, Actinomyces sp, Nocardia sp, Escherichia coli, Streptococcus sp (e.g., S. pneumoniae) Klebsiella sp Other causes 1. Viral: 1. 2. 2. canine distemper, feline infectious peritonitis Mycotic infection: 1. 2. 3. histoplasmosis, cryptococcosis and blastomycosis. Clinical signs 1. 2. 3. 4. 5. hyperesthesia, fever, cervical pain, and frequently, cervical rigidity. In addition, vomiting, bradycardia, anorexia, occasional cranial nerve deficits, and seizures may be observed. 1. Seizures may be caused by high fever, brain edema, or inflammation, 2. while vomiting may result from increased intracranial pressure or from direct effects on the vomiting center Stiff gait and walking with caution (as walking on eggs) Congested MM (fever in meningitis Rigidity in the neck Diagnosis Case history Clinical signs CSF examination for color, protein and Gram stain Cells (neutrophilia if bacteria is the cause) Treatment 1. 2. 3. 4. Antibacterial: can pass blood-brain barrier 1. Chloramphenicol (50 mg/kg, IV, IM, or SC, bid), 2. metronidazole (10 - 15 mg/kg, PO, tid), 3. trimethoprim-sulfonamide (30 - 60 mg/kg, PO, daily 4. Ampicillin, 5 - 10 mg/kg, IV, every 6 hours Anticonvulsant (antiseizure): Diazepam Anti-inflammatory: prednisone 2mg/kg Osmotic diuretics may be useful for treating increased intracranial pressure secondary to brain edema. ENCEPHALITIS Definition Encephalitis is inflammation of brain tissue that may extend to spinal cord (encephalomyelitis) causing seizures, circling and blindness in dogs Etiology A-Viral 1. Canine distemper, 2. Rabies (rhabdovirus) 3. Herpes virus (puppies) B- Granulomatous encephalitis (mycotic, e.g. Cryptococcus and Histoplasma). C-Parasitic: 4. Dirofilaria immitis or 5. Canine Angiostrongylus vasorum infestation 6. Toxoplasmosis (toxoplasma gondi) D- Genetic condition Clinical Signs 1. 2. 3. 4. 5. 6. 7. 8. 9. Seizures, Depression, Abnormal gait and incoordination Blindness, Walking in circle Staring off into space, Pressing their heads against the wall or furniture, Ataxia (a staggering walk), and Intermittent screaming. Diagnosis 1. 2. 3. 4. 5. 6. The disease is hard to diagnose since its symptoms often relate to other CNS diseases. Seizures may be caused by many other underlying conditions such as hypoglycemia, canine distemper, rabies, Analyzing the white blood cells in the spinal fluid Most often the disease is diagnosed after the dog die Positive diagnosis may be made through use of immunofluorescent or immunocytochemical techniques to detect canine distemper viral antigen in brain sections and other tissues (e.g., mononuclear cells in blood smears, conjunctival or tracheal washes Magnetic Resonance Imaging (MRI) is a diagnostic test that allows visualization of the structures of the brain) Treatment 1. 2. 3. 4. Anticonvulsants, such as phenobarbital, may help control seizures Anti-inflammatory: oral prednisone, 1 to 2 mg/kg/day initially for several days, then reducing the dosage to 2.5 - 5 mg on alternate days Amphotericin B: 0.1 to 0.5 mg/kg body weight, IV, three times weekly (for mycotic encephalitis) Ivermectin: 0.2 mg/kg S/C 5- FELINE SPONGIFORM ENCEPHALOPATHY (FSE) Definition Specific brain disease affecting cats related to bovine spongiform encephalopathy (BSE) and scrapie in sheep. Etiology and pathogenesis Oral exposure from consumption of foodstuffs derived from cattle contaminated with the BSE agent which in turn was spread to cattle through animal protein concentrates (e.g., meat and bone-meal) processed from scrapieinfected sheep carcasses. The infectious agent in these spongiform encephalopathies is a protease resistant prion protein (PrP), a product of nerve cells, and considered to be an abnormal posttranslational modification of a host-encoded membrane-bound cellular glycoprotein produced by infection that accumulates in the affected brain Clinical signs 1. 2. 3. 4. 5. 6. 7. 8. 9. Muscle tremors Ataxia (especially of the pelvic limbs) Dilated pupils, Jaw champing,Salivation Behavioral abnormalities such as uncharacteristic aggression, biting Hyperesthesia Creeping about the house and hiding Vacant staring Excessive grooming, and being easily startled (fear) by noise Kangaroo-like movements in advanced cases Diagnosis 1. 2. 3. History Clinical signs Microscopic exam: diffuse vacuolation (single or multiple vacuoles) of gray matter and neurons throughout the brain, particularly in cerebral cortex Treatment There is no treatment. Prognosis is poor, since all spongiform encephalopathy cases are fatal. Questions