* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Effects of Nitroprusside on Venous Return and Central
History of invasive and interventional cardiology wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
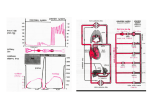
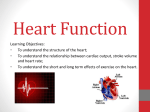
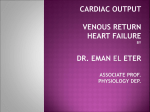
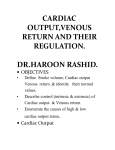
Effects of Nitroprusside on Venous Return and Central Blood Volume in the Absence and Presence of Acute Heart Failure HUBERT POULEUR, M.D., JAMES W. COVELL, M.D., AND JOHN Ross, JR., M.D. Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 SUMMARY The effects of nitroprusside (380-760 ug/min) on the systemic venous return, the central blood volume and the equilibrium point between the venous return and cardiac output curves were studied in eight dogs using a right-heart bypass preparation at constant total blood volume. Experiments were performed before and after the production of acute left ventricular failure. During control, nitroprusside infusion shifted the venous return curve, with a reduction in its plateau (3.1 to 2.4 l/min;p < 0.005), the central blood volume fell (-2.4 ± 0.4 ml/kg; p < 0.05) and the cardiac output at equilibrium was reduced (3.1 to 2.4 1/min; p < 0.005). Cardiac failure (produced by acute coronary artery ligation) increased the central blood volume (+6.3 ± 0.6 ml/kg; p < 0.01), leading to a decrease in both the systemic blood volume and the plateau of the venous return curve (3.2 to 2.6 1/min; p < 0.003). The cardiac output at equilibrium was also reduced (3.2 to 1.9 1/min; p < 0.001). In this setting, nitroprusside infusion decreased the central blood volume (-7.4 ml/kg; p < 0.01), but the venous return curve was not altered. The cardiac output curve was markedly shifted upward due to reduced afterload on the failing left ventricle; however, in the absence of a downward shift of the venous return curve, the cardiac output at equilibrium increased from 1.9 to 2.6 1/min (p < 0.05). We conclude that the differing effects of nitroprusside in acute cardiac failure are due primarily to an increased shift of blood from the central circulation in the failure state compared with the normal circulation. This shift counteracts the systemic venodilatation produced by nitroprusside and allows the markedly improved left ventricular function consequent to reduced afterload to be expressed as increased venous return and cardiac output. tion may occur;`4 however, this has not been critically or quantitatively examined, and in one study no change in the central blood volume was found during nitroprusside use in a patient with hypertension.15 Thus, although the effects of vasodilators on cardiac output and preload (left-heart filling pressures) have been amply documented,'-6 some investigators suggested that nitroprusside can cause peripheral venous pooling and thereby a reduction in the venous return to the right heart.'6 While a mechanism involving decreased venous return during nitroprusside infusion might be operative in the relatively normal circulation, in which a reduction in cardiac output usually accompanies nitroprusside use," 17 it is clearly incompatible with the increased cardiac output generally observed during such therapy in patients with congestive heart failure,1 2 because a steady-state augmentation in the cardiac output must be associated with a commensurate increase in venous return.'8 Therefore, we examined the responses to nitroprusside infusion in the presence and absence of left ventricular failure and tried to determine the mechanism by which this drug improves the output of the failing heart, despite an increase in the venous capacitance and a decrease in cardiac filling pressures.' We gave particular attention to the character of the venous return curves," the volume of blood in the central circulation,'9-21 and the shifts in this blood volume between the central and systemic circulations both in the normal and failure states. VASODILATOR THERAPY, or afterload reduction, has an important role in the treatment of congestive heart failure.1-6 Several clinical and experimental studies have shown that in congestive heart failure nitroprusside increases the cardiac output while decreasing the left ventricular end-diastolic pressure and relieving pulmonary congestion.' 6 There is evidence that these improvements are not the same when oral nitrates are used, because the cardiac output may not be significantly increased,7-9 and when hydralazine alone is used, increased cardiac output may occur without relief of pulmonary congestion." Attempts have been made to explain the superiority of nitroprusside by a balanced action of this agent on the resistance and capacitance vessels,' but how such an action might explain opposite responses of the cardiac output in the normal and heart failure states has not been investigated. Increased capacitance of the venous bed due to vasodilators has been shown in experimental animals,"," and vasodilators have been shown to decrease the forearm venous tone in patients with congestive heart failure." It has been suggested that a shift of blood from the central to peripheral circulaFrom the Division of Cardiology, Department of Medicine, University of California, San Diego, School of Medicine, La Jolla, California. Supported by NIH research grants HL-17682 and HL-12373, NHLBI, PHS/DHEW. Dr. Pouleur is a Fogarty International Fellow, No. 5 F05 TWO 2549-02. Address for correspondence: John Ross, Jr., M.D., Director, Division of Cardiology, Department of Medicine, M-013, University of California, San Diego, La Jolla, California 92093. Received October 13, 1978; revision accepted August 20, 1979. Circulation 61, No. 2, 1980. Methods Experimental data were obtained from eight mongrel dogs (mean weight 24 kg, range 19-33 kg) anesthetized with sodium pentobarbital (25 mg/kg 328 EFFECTS OF NITROPRUSSIDE ON VENOUS RETURN/Pouleur et al. Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 i.v.). Ventilation was maintained by a Harvard respirator with oxygen-enriched room air (20 ml/kg). After a median sternotomy, the heart was suspended in a pericardial cradle. Figure 1 shows a schematic diagram of the preparation. A 3-mm i.d. steel cannula was inserted into the left ventricle through a stab incision at the apex and connected to a Statham P23Db strain gauge manometer. The frequency response of this cannula coupled to the manometer was flat to 100 Hz and gain was linear to 200 mm Hg. A micromanometer (Millar 5F Model PC340A) was introduced through the right femoral artery and its tip was located just above the aortic valve for measurement of central aortic pressure. A silastic rubber catheter (1.1 mm i.d.) was also introduced in the right atrium via the left mammary vein and connected to a Statham P23Db transducer calibrated at high gain (20 mm Hg full scale). Zero reference levels were taken at the level of the mid-right atrium. Hydrostatic errors in right atrial pressure measurements were determined at the end of each experiment by exposing the catheter tip in situ to atmospheric pressure. Necessary corrections to the recorded right atrial pressure, if any, were then made. An electromagnetic flow probe (Biotronex) was implanted around the aortic root and connected to a Biotronex BL 610 flowmeter; probe diameter was selected to give a satisfactory signal during diastole at low aortic pressures and to avoid significant baseline shift during transient changes in aortic pressure; the mean pressure gradient across the probe was less than 5 mm Hg. The frequency response of this system was flat (-3 dB) from 0-100 Hz, with a transit time of 6 msec and a linear phase shift of 1.9°/Hz. The dogs were then placed on right-heart bypass. In brief, a wide-bore Bardic cannula (40F) with a multihole tip was introduced into the right atrium via the right atrial appendage and its tip advanced into the right ventricle. A 26F Bardic cannula was introduced 329 into the main pulmonary artery through the right ventricular outflow tract and secured with a tie around the pulmonary artery. The circuit (volume 350 ml) was primed with two-thirds dextran (MW 70,000 in 0.9% saline) and one-third Ringer's lactate. The entire venous return to the left heart was then assumed by a roller pump and measured by a Biotronex cannulaflow probe inserted in the external circuit. Dextran (50-70 ml) was infused to replace blood lost during surgery, and before collecting data the preparation was allowed to stabilize for 15 minutes at a right atrial pressure of 0-2 mm Hg. All signals together with a standard ECG lead II were simultaneously recorded on paper and on FM magnetic tape for later replay at a paper speed of 100 mm/sec. Control Measurements Venous Return Curves In eight dogs, the relation between the venous return to the right heart and the right atrial pressure was determined using a procedure modified after a method described by Guyton et al."1 In brief, starting from the control point (hemodynamic data obtained after stabilization at a right atrial pressure of 0-2 mm Hg and a mean left ventricular end-diastolic pressure of 9.4 ± 1.5 mm Hg), the speed of the roller pump was abruptly reduced or increased to a desired level and maintained there for 8-10 seconds. After the initial change in right atrial pressure, venous return to the right atrium responded reaching a new level and equilibrium between right atrial pressure and the venous return was rapidly achieved. At this transient equilibrium point, the output of the venous pump (measured with a flowmeter) equaled the venous return. During this brief period, significant vasomotor reflexes had not yet occurred," as evidenced by a con- E.M.F SG Heat Exchanger ,' SVC ,P FIGURE 1. Schematic diagram of the modified right-heart bypass preparation. IVC = inferior vena cava; SVC = superior vena cava; SG = strain gauge; EMF = electromagnetic flowmeter; PA = pulmonary artery; L V = left ventricle; R V = right ventricle. Millar A Micromanometer ClIRCULATION 330 VOL 61, No 2, FEBRUARY 1980 could displace the junction between the linear portion and the plateau of the venous return curve. This artifact, caused by the transmission of pulsatile waves from the pump backward to the right atrium, was minimized by interposing the heat exchanger between the roller pump and the right atrium. Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 stant heart rate. In addition, pump output changes during this period had little effect on release or trapping of blood in the lungs; the increases or decreases in central blood volume during the transient period were less than 1 ml/kg and of the same magnitude in all the maneuvers studied. Changes due to alterations in right-sided pump output should have been similar in our preparation to those in Guyton's transient method, which was shown to produce venous return curves similar to those in the isolated circulation."' Between each such measurement the pump speed was returned to the control level, and additional points were determined only when the right atrial and the left ventricular end-diastolic pressures had restabilized at their previous control levels (generally after 1.5-3 minutes). At least five points on the descending portion of the venous return curve and two points high on the venous return curve at right atrial pressures below 0 mm Hg were determined in each dog. It was found in obtaining the latter two points on the plateau of the venous return curve (fig. 2) that it was not possible to augment the pump output further even at more negative right atrial pressures, because the venous system cbllapses; i.e., the cardiac output is now limited by the amount of venous return." No attempt was made to directly determine the mean systemic pressure, which is a measure of the degree of filling of the systemic circulation at any given time.'2 22 Instead, the linear portion of the venous return-right atrial pressure relation was extrapolated to zero venous return to provide a reasonable approximation of this variable"' 23 (broken lines, fig. 2). No Starling resistor was inserted in the circuit; Guyton et al.1" have shown that the absence of a collapsible tube in the circuit does not quantitatively modify the results but Cardiac Output Curves of the Left Ventricle After recording the venous return curve, the cardiac output curve was determined by obtaining measuremdnts of flow and left ventricular end-diastolic pressure at three to five different levels of venous return, each point being obtained after 2 minutes in the steady state. Nitroprusside Infusion Before Heart Failure With the preparation stable at the control point, nitroprusside was infused in six dogs in a dose (380-760 gg/min) sufficient to produce a sustained decrease in mean aortic pressure, averaging -30 mm Hg. When a steady-state level of mean aortic and left ventricular end-diastolic pressures was obtained, the venous return curve and the cardiac output curve were repeated as described above. During the transient periods of decreases in mean aortic pressure, the venous return and the aortic blood flow were continuously recorded, and by subtracting the aortic flow from the venous return flow, the shift in the volume of blood contained between the pulmonary artery and aorta (central blood volume) was computed as previously described.24 25 Briefly, this approach is based on the assumption that, during a steady state, the amount of blood entering the lungs is equal to the 300T0 * CONVTROL o AIITROPRUSSIDE .E co (n=6) 2000k FIGURE 2. Curves relating venous return to the right heart to the mean right atrial pressure; such curves reflect primarily the characteristics of the peripheral circulation. 7 Average venous return curves ( SD) obtained under control conditions before and during nitroprusside infusion in six dogs are shown. The venous return data are normalized to an average body weight of 20 kg. CBV= central blood volume. a: F- Lii co_ a: C/) 1000 A CBV = -2.4 ± 0.4 m/Kg-' , -2 , , 0 2 4 jm* 6 RIGHT ATRIAL PRESSURE 8 mmHg EFFECTS OF NITROPRUSSIDE ON VENOUS RETURN/Pouleur et al. amount of blood leaving the left ventricle. Small amounts of flow (bronchial and coronary flows) are not detected by the flow probes, but the changes in these flows were probably small, and the effects of these two flows tend to cancel one amother.26 Because the validity of the computation is dependent upon the stability of the gain and of the zero flow levels of the two flow transducers, the reproducibility of the equilibrium between the two signals was checked at the different steady states in each dog and found to be within ± 0.2%; i.e., there was a maximum cumulative error of 4 ml/min at a cardiac output of 2000 ml/min. Heart Failure Produced by Coronary Occlusion Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 After recording control data and the responses to nitroprusside in five dogs, and in two additional dogs directly after recording the control data, the left anterior descending artery was abruptly occluded after premedication with lidocaine (2 mg/kg i.v.). During the ensuing period it was generally necessary to decrease the speed of the roller pump to avoid acute cardiac dilatation and to achieve a new steady state with left ventricular end-diastolic pressure averaging approximately 10 mm Hg higher than control. At this new steady state, the venous return and cardiac output curves were then determined. Similarly, changes in central blood volume during the transient period were computed by continuous subtraction of the two flow signals. In these seven dogs with coronary occlusion, nitroprusside (380-760 ,ug/min) was then infused and the venous return and cardiac output curves and the central blood volume were measured in the same way as during the control nitroprusside infusion. In all dogs, total peripheral resistance was calculated by the following formula: (mean aortic pressure - mean right atrial pressure)/mean aortic flow, and expressed in dyn-sec-cm-5. Statistical analysis of the data was performed by paired t test, and results having ap value less than 0.05 were considered significant. Results Relations Between Right Atrial Pressure and Venous Return Before and During Nitroprusside Control Conditions (Without Cardiac Failure) The averaged venous return curves obtained under control conditions before and during nitroprusside infusion for six dogs, normalized to an average weight of 20 kg, are illustrated in figure 2. Nitroprusside infusion caused a significant downward displacement of this relation (absolute average values [+ SEM] for the plateaus from 3100 + 300 to 2400 + 280 ml/min; p < 0.005), and the extrapolated mean systemic pressures fell (from 8.3 ± 0.9 to 7.2 ± 0.8 mm Hg; p < 0.05). There were no significant changes in the slopes of the linear portions of the curves (489 + 52 to 516 ± 59 ml/mm Hg; NS). 331 Cardiac Failure After the increase in left ventricular end-diastolic pressure due to coronary occlusion, and reduction of pump output, the position of the venous return curve was also below control, as shown in figure 3 (absolute values from 3200 + 365 to 2550 ± 321 ml/min; p < 0.003, n = 7), and the estimated mean systemic pressure also fell from 9.3 ± 0.8 to 7.6 ± 0.8 mm Hg (p < 0.005) without change in the slope of these relations (464 ± 50 and 521 ± 82 ml/mm Hg; NS). As shown in figure 3, when nitroprusside was infused in these seven dogs after coronary occlusion, there was no change in either the plateau of the curve (2550 ± 320 to 2580 ± 270 ml/min; NS) or the mean systemic pressure (7.6 ± 0.8 to 7.3 + 0.7 mm Hg; NS); the slopes also were not different (521 ± 82 to 535 ± 76 mm Hg-1; NS). Also, in the five dogs in which nitroprusside infusion was performed both before and after coronary occlusion, significant differences were not observed between the two venous return curves. Changes in Left Ventricular End-diastolic Pressure and the Central Blood Volume Control Conditions Nitroprusside infusion during control conditions decreased left ventricular end-diastolic pressure from 9.5 + 1.6 to 4.5 ± 1.5 mm Hg (p < 0.002), and the central blood volume fell; when the new steady state was reached, 2.4 ± 0.5 ml/kg of blood had been shifted from the central to systemic circulations (p < 0.05, compared with the theoretical maximal cumulated error during the same period, i.e., -1.0 ± 0.03 ml/kg). Cardiac Failure After coronary occlusion, left ventricular enddiastolic pressure increased from 9.5 ± 0.9 to 19.7 ± 2.0 mm Hg (p < 0.003), and 6.3 ml/kg (p < 0.01) of blood shifted from the systemic circulation into the central circulation between the control and failure states. Nitroprusside infusion after coronary occlusion decreased left ventricular end-diastolic pressure to 9.5 i 0.9 mm Hg (p < 0.0003), and the central blood volume fell by 7.4 i 1.3 ml/kg (p < 0.01). Left Ventricular Function Curves and Equilibrium Points Between the Cardiac Output and Venous Return Curves Figure 4 illustrates a representative experiment showing the curves relating cardiac output and left ventricular end-diastolic pressure before and after coronary occlusion, and the effects of nitroprusside. Coronary occlusion consistently produced a shift of the function curve downward and to the right (curve A to C); nitroprusside both before and after coronary occlusion shifted the curves upward and toward the left (A to B, C to D). Figure 5 provides a schematic analysis of the rela- VOL 61, No 2, FEBRUARY 1980 CI RCULATION 332 B A 3000 * * CONJTROL A * COROINARY OCCLUSIOIN (n=7) CORONARY OCCLUSION INITROPRUSSIDE DUR/IVG CORONlARY OCCLUSION (n=7) 1=c .E 2000- :m C/) nr U) L.U 2E 1000 CI = 7A+ -7.4 ± 1.3S mt.Kg-' AACBV = +6.3+0.6 mlKg-' \ \ \ l l l l Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 8 6 4 2 0 -2 l 2 10 6 RIGHT ATRIAL PRESSURE mmHg RIGHT ATRIAL PRESSURE mmHg FIGURE 3. A) Average venous return curves (fi SD) obtained under control conditions and after coronary occlusion in seven dogs. B) A verage venous return curves obtained after coronary occlusion before and during nitroprusside infusion in seven dogs. The venous return data are normalized to an average body weight of 20 kg. CBV= central blood volume. tioni between the venous return and cardiac output curves. In this figure, the values for the systemic venous return and for the left ventricular function curves were obtained from the same dog as illustrated in figure 4, and left ventricular end-diastolic pressure was used to represent the mean left atrial pressure. The right ventricular function curves were adapted from the data of Guyton et al.'8-20 The pulmonary venous return was not represented, because in the steady state it is equal to the systemic venous return. Under control conditions (fig. 5A) the systemic venous return was the limiting factor for cardiac out- A 3000 F B D i=E . c _ FIGURE 5. Schematic analysis of the relation between venous return and right or left ventricular output curves before and during nitroprusside infusion under control conditions (A) and after coronary occlusion (B). Points A, B, C and D indicate the equilibrium points between cardiac output and venous return curves. 2000K CD W c0 C-, C-, * CONITROL 1000o 0 NVITROPRUSSIDE CONTInuL * CORONARY OCCLUSION A 1 l l A A NITROPRUSSIDE DURINAG CORONARY OCCUlSIO/I l l 16 12 24 20 LEFT VENT. END DIASTOLIC PRESSURE mmHg 4 8 28 EFFECTS OF NITROPRUSSIDE ON VENOUS RETURN/Pouleur et al. 333 RIGHT VENTRICULAR OUTPUT 3000 cn_ C,, 2000 U) cr_ C), I-.C Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 --- NVitroprusside c= During Control . 1000 W -4 8 4 0 12 FIGURE 4. Relation between cardiac output and left ventricular end-diastolic pressure obtained in one representative dog under differing experimental conditions. Points A, B, C and D indicate the positions of the plateau of the venous return curve in control, control + nitroprusside, coronary occlusion, and coronary occlusion + nitroprusside, respectively. 16 RIGHT OR LEFT ATRIAL PRESSURE (mmHg) A RIGHT VENTRICULAR OUTPUT :IC= c) 2000 Cl C) ILJ- CL -Coronary Occlusion 1000 C) cz_ C -4 B 0 4 8 12 16 20 RIGHT OR LEFT ATRIAL PRESSURE (mmHg) 24 334 CIRCULATION Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 put, the equilibrium point being on the plateau of the systemic venous return curve (point A). This was also the case when nitroprusside was infused under control conditions (point B). Despite a moderate shift upward of the left ventricular function curve during nitroprusside, cardiac output fell as left ventricular filling pressure decreased (fig. 5A, points A, to B1). The trend illustrated in figure 5 was observed in all six dogs, and average hemodynamic data at the equilibrium points in all dogs is summarized in table 1. After coronary occlusion (fig. 5B), the left ventricle was unable to maintain an output equal to the plateau of systemic venous return, and the right atrial pressure increased to reach an equilibrium between the systemic venous return and the left ventricular output (point C); in our controlled experimental setting, this was accomplished by reducing the speed of the roller pump. Nitroprusside infusion under these conditions markedly shifted the cardiac output curve upward, and because the venous return curve was unchanged at equilibrium, a substantial rise in the cardiac output occurred (points C to D). A marked shift upward of the left ventricular function curve occurred during nitroprusside, and the cardiac output was higher at a considerably lower filling pressure (fig. SB, C1 to D1). Average equilibrium points in all seven dogs are shown in table 1. The relations between cardiac output and venous return schematized in figure 5 were observed in all dogs during control and in five of the seven dogs after coronary occlusion. In the remaining two dogs (not illustrated), the left ventricular depression was less pronounced, and equilibrium points before and after nitroprusside were at the plateau of the venous return curve. Thus, both during control and in the failing heart the venous return was the limiting factor of the cardiac output in all dogs during nitroprusside infusion; during failure, cardiac output at this new equilibrium point was increased in five dogs and unchanged in two. The average increase in cardiac output in the failing heart for the whole group was +600 ml/min (p < 0.05), and significant decreases in mean aortic pressure and in left ventricular systolic and enddiastolic pressure also occurred (table 1). Discussion The concept that peripheral factors are as important as cardiac factors in the regulation of cardiac output was discussed by Starling in 189527 and recently has received extensive and quantitative confirmation from the studies of Guyton and co-workers',18-21 Vasodilators now have an important role in the therapy of acute and chronic congestive heart failure, and the effects of these agents on arterial impedance, cardiac filling pressures, and ventricular performance have been investigated extensively.' 6, 28 However, their effects on the systemic venous circulation and the consequent role of the venous bed in regulating the cardiac output in the absence and presence of heart failure have not been quantitatively explored, and the VOL 61, No 2, FEBRUARY 1980 aim of the present investigation was to apply the general approach of Guyton to this problem. The method used herein to measure venous return is a modification of one previously used by Guyton and co-workers to determine venous return curves in openchest dogs." In the present study, instead of suddenly changing the right atrial pressure and measuring the resulting venous return, venous outflow was abruptly altered and held constant and the right atrial pressure was measured as it reached the new equilibrium point. The striking similarity between the venous return curves thus obtained and those reported in dogs11 23, 29 make it likely that the two experimental approaches provide comparable data. In all methods that use transient responses to determine the venous return curve, some blood is unavoidably trapped within or released from the pulmonary circulation during the 8-10second study period, which could modify the mean systemic pressure and the venous return. However, this volume was shown to be small (< 1 ml/kg) and of similar magnitude during the various interventions. Moreover, it has been previously shown that venous return curves determined either in the steady state or by the transient method are identical in areflexic dogs," further supporting the use of the approach. The fact that relatively small changes in blood volume can produce marked reductions in venous return raises the question of artifactual changes due to spontaneous bleeding and/or to fluid shifts into the extravascular spaces during the course of the study.'0 Significant bleeding was prevented by careful homeostasis during surgery; moreover, changes in total blood volume sufficient to bias our conclusions did not appear to occur during the time of data collection (120 minutes) for the following reasons: 1) In the five dogs in which nitroprusside was infused both in the control period and after coronary occlusion, the two venous return curves during nitroprusside infusion were identical; if significant changes in total blood volume had occurred, the increase in venous capacitance produced by the same dose of nitroprusside should have resulted in a lower venous return at the end of the experiment during the second infusion. 2) In two dogs, the time between control studies and coronary occlusion was deliberately reduced by eliminating the control nitroprusside infusion; the control venous curve and that during acute heart failure were performed within less than 30 minutes of each other, and the results were identical to those observed in the other dogs. When nitroprusside was infused in the absence of heart failure, mean systemic pressure fell and the systemic blood volume increased only slightly. Nitroprusside markedly increases the capacitance of the systemic bed, particularly on the venous side,"3 suggesting that the amount of blood transferred from the central circulation to the systemic bed was smaller than the increase in systemic venous capacitance. In this connection, Tarazi et al." reported only a small, nonsignificant fall in cardiopulmonary blood volume (measured by indicator-dilution technique) during nitroprusside infusion in hypertensive subjects without EFFECTS OF NITROPRUSSIDE ON VENOUS RETURN/Pouleur et al. 5 ,4 c; 0 00 N 0 CD Cl 0) 0 (o c1- c 0 0 0 0 V H "? A- 0 0) CO 0V cl 0 0 ~o cl 0 C) CS7 v ci a' 1'- CO m z 0) IC c m 0 m CO 0 0 cl V V- 0 cO -H LC= z c'3 P-H cC CO CO 0 r-H (o cl z m m 1-0 CI Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 -H +a P0 x. 4^ 0 0)' U 0 0 C= CO m-H 0 10 o 0 0 Co 0 0 0 c- 0 0 0 C) CD co v V m cq V kc 10 2) 2) 2) 1. -H ---0 5.4 10 ko 0 0)e 0 o U c;0 ;o cz ¢. v V CO 't t- 0 CO 6 co V a) S 0) Q 0) 0) 0 X 0)a) C 2) 2) cr- cH Cv C Q) v. 600 C;. 0 C= 01) o) 0 0) c; 0) 0) 0 C V 0 -H 0 - 0) 0 0 03 - CO - CO u: In 0 C 1o CS -H~; oi v tIl-H 0 0 cO 0 LO 6 0) V -H c) co 0 10 fo C 6 0 0) 0 0 V 2) 0)1 X blJ 0) I.' CO CI 0 Cd "5 2) V --- 0) -H p 0 m m kl0 cM l c CD v V - q 2) C 'C 0 2) 0 0 m H 335 heart failure. If circulatory reflexes do not compensate under such circumstances, the cardiac output (after a transient increase reflecting the small transfer of blood from the lungs) should decrease below control because venous return is the factor limiting cardiac output under normal conditions.18 This was found to be the case; the observed shift downward of the venous return curve and the fall in cardiac output when vasomotor tone was reduced by nitroprusside resembled the response previously reported when venomotor tone was altered by ganglionic blockade together with a decreased rate of epinephrine infusion.'1' 12, 30, 33 The responses we observed in cardiac output and filling pressures are similar to those observed in patients with heart disease who do not have elevated left-heart filling pressures.' The response is also similar to that in some normal patients with nitroprusside administration, although when the reflexes are intact the cardiac output sometimes increases. Such circulatory effects of nitroprusside in the normal circulation are characterized by strong secondary neurogenic and humoral responses, with persistent tachycardia in dogs34 and an increase in heart rate and plasma catecholamine concentrations in patients.35 Thus, in the normal circulation, marked reflex responses can come into play which tend to restore the venous return, cardiac output and the aortic pressure toward normal.34 Other effects of nitroprusside include direct vasodilation of the pulmonary vasculature,'2 which may also play a role in observed hemodynamic responses. With the production of acute heart failure, the systemic blood volume fell because blood was translocated from the systemic vascular bed into the pulmonary circulation and left heart, as pointed out in other analyses of acute left-heart failure.'9' 20 We reduced pump flow and cardiac output in order to prevent cardiac overdistension, but a fall in the cardiac output also occurs during acute heart failure in the uncontrolled circulation.20 That a significant amount of blood is trapped in the pulmonary circulation during acute heart failure has been previously shown by Lindsey et al.,2' who demonstrated an increase in central blood volume from 10.3 ml/kg to 17.5 ml/kg after 3 minutes of major left-heart failure. Evidence of s.tress relaxation in the pulmonary circulation36 suggests that this volume could increase with time. In our study, a mean of 6.3 ml/kg of blood was displaced from the systemic circulation into the central circulation during heart failure. Previous studies by Guyton et al.12 Harlan et al.22, and Drees and Roth30 have shown that such a loss of blood from the systemic circulation significantly decreases the mean systemic pressure and the venous return. In the normal circulation, carotid sinus baroreceptor reflex activity can significantly reduce the venous capacitance and compensate for a hemorrhage of 7.5-10 ml/kg;3'0 37 ventricular afferent fibers also may be stimulated during coronary occlusion and cause increased sympathetic tone.9 38 However, in the open-chest animal under sodium pentobarbital anesthesia, sympathetic tone is 336 CIRCULATION already near maximal,39 and it seems likely that the changes in the position of the venous return curve during acute heart failure were due largely to the shift in blood volume to the central circulation. When nitroprusside was infused in the presence of left ventricular failure during the transient period as the aortic pressure fell, the left ventricular stroke volume increased while the ventricular end-diastolic pressure decreased; when the new steady state was reached, approximately 7.4 ml/kg of blood had been transferred from the central circulation to the systemic circulation. No significant changes in the venous return curves or the mean systemic pressure were observed, indicating that the amount of blood shifted from the central circulation was roughly equal to the increase in systemic venous capacitance produced by nitroprusside. This lack of effect on the venous return curve allowed a steady-state increase in the cardiac output. Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 Clinical Implications This experimental preparation represents an artificial, controlled setting for studying the circulatory effects of acute left ventricular failure and the actions of nitroprusside, and extrapolations to the clinical setting of heart failure, therefore, should be made with caution. This applies in particular to the setting of chronic left ventricular failure, in which the venous return curve may be displaced upward and to the right,18' 19 although even under such circumstances the responses to nitroprusside could be similar to those we observed. The experimental findings reported might have particular relevance, however, to the condition of acute left ventricular failure in man, as may occur after acute myocardial infarction. The fact that administration of nitroprusside to patients with relatively low left-heart filling pressures after acute myocardial infarction can cause a fall in the cardiac output has been well documented.1 Based on our observations, this response can be largely explained by the lack of a sufficient shift in blood volume from the undistended central circulation and left heart to the peripheral circulation to compensate for the venodilator action of nitroprusside. Under such circumstances, other adverse effects, such as reflex tachycardia, can also occur. In acute heart failure in man, if the shift in blood volume from the central to the peripheral circulation during nitroprusside infusion is similar in magnitude to the increase in systemic capacitance produced by this agent, an explanation is provided for the opposite effect, a rise in the cardiac output, which has been observed in such patients.1' 3 17 This lack of shift of the venous return curve was associated with a marked upward shift in the function curve of the left ventricle, which led to the increase in cardiac output. There may be other causes for the differences between the normal and failing circulations. The unloading of the failing heart appears to have a more dramatic effect on its pump function than on the normal ventricle.1' 40 As illustrated in figure 4, the failing VOL 61, No 2, FEBRUARY 1980 ventricle was working at a high end-diastolic pressure on a flat ventricular function curve, and the steep diastolic pressure-volume curve allowed relatively small reductions in ventricular volume (with correspondingly small effects on the Frank-Starling mechanism) to be associated with large decreases in the filling pressure.41 In addition, there is evidence that an apparent "descending limb" of the function curve in heart failure can be due to excessive afterload.40 42 In recent studies we have shown that unloading of the ventricle by nitroprusside can be explained by a decrease in the afterload, defined as the left ventricular wall stress during systole, which is determined both by the aortic input impedance and by geometrical factors.28 In acute heart failure, by markedly reducing the wall stress, nitroprusside allows the ventricle to improve its stroke volume and to function at a lower enddiastolic volume. Because in acute cardiac failure the pumping ability of the heart was usually the limiting factor for cardiac output, in contrast to the normal situation in which the venous return was limiting, the lack of a downward shift in the venous return curve during nitroprusside administration in heart failure allowed the markedly improved pumping ability of the left ventricle produced by systolic unloading to be expressed as an increase in the cardiac output (fig. 4). The fact that the ventricle can achieve a higher cardiac output when nitroprusside is used in heart failure leads to a smaller decrease in aortic pressure than occurs under normal conditions, despite a substantially greater decrease in the calculated total peripheral resistance (table 1). These responses should produce a reduced change in baroreceptor activity and less marked reflex responses in patients with heart failure than under normal conditions. Moreover, the documented reductions in the gain of high- and lowpressure baroreceptors in heart failure43' 4 may be contributory. Such conclusions are consistent with the minimal change in heart rate1' 3 and the decrease in plasma catecholamine concentrations that have been observed with nitroprusside therapy in patients with heart failure.35 References l.Chatterjee K, Parmley WW, Ganz W, Forrester J, Walkinsky P, Crexells C, Swan HJC: Hemodynamic and metabolic responses to vasodilator therapy in acute myocardial infarction. Circulation 48: 1183, 1973 2. Cohn JN, Mathew JK, Franciosa JA, Snow JA: Chronic vasodilator therapy in the management of cardiogenic shock and intractable left ventricular failure. Ann Intern Med 81: 777, 1974 3. Franciosa JA, Guiha NH, Limas CJ, Rodiguera E, Cohn JN: Improved left ventricular function during nitroprusside infusion in acute myocardial infarction. Lancet 1: 650, 1972 4. Goodman DJ, Rossen RM, Holloway EL, Alderman EL, Harrison DC: Effect of nitroprusside on left ventricular dynamics in mitral regurgitation. Circulation 50: 1025, 1974 5. Miller RR, Vismara LA, Williams DO, Amsterdam EA, Mason DT: Pharmacological mechanisms for left ventricular unloading in clinical congestive heart failure: differential effects of nitroprusside, phentolamine and nitroglycerin on cardiac function and peripheral circulation. Circ Res 39: 127, 1976 6. Miller RR, Vismara LA, Zelis R, Amsterdam EA, Mason DT: EFFECTS OF NITROPRUSSIDE ON VENOUS RETURN/Pouleur et al. 7. 8. 9. 10. 11. 12. 13. Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 14. 15. 16. 17. 18. 19. Clinical use of sodium nitroprusside in chronic ischemic heart disease. Circulation 51: 328, 1975 Gold HK, Lienbach RC, Sanders CA: Use of sublingual nitroglycerin in congestive failure following acute myocardial infarction. Circulation 46: 839, 1972 Gray R, Chatterjee K, Vyden JK, Ganz W, Forrester JS, Swan HJC: Hemodynamic and metabolic effects of isosorbide dinitrate in chronic congestive heart failure. Am Heart J 90: 346, 1975 Williams DO, Amsterdam EA, Mason DT: Hemodynamic effects of nitroglycerin in acute myocardial infarction. Circulation 51: 421, 1975 Chatterjee K, Parmley WW, Massie B, Greenberg B, Werner J, Klausner S, Norman A: Oral hydralazine therapy for chronic refractory heart failure. Circulation 54: 879, 1976 Guyton AC, Lindsey AW, Abernathy B, Richardson T: Venous return at various right atrial pressures and the normal venous return curve. Am J Physiol 189: 609, 1957 Guyton AC, Polizo D, Armstrong GG: Mean circulatory filling pressure measured immediately after cessation of heart pumping. Am J Physiol 179: 261, 1954 Mason DT, Braunwald E: The effects of nitroglycerin and amyl nitrite on arteriolar and venous tone in the human forearm. Circulation 32: 755, 1965 Cohn JN, Franciosa JA: Vasodilator therapy of cardiac failure. N Engl J Med 297: 27, 1977 Schlant RC, Tsagaris TS, Robertson RJ: Studies on the acute effects of intravenous sodium nitroprusside. Am J Cardiol 9: 51, 1962 Guiha NH, Cohn JN, Mikulic E, Franciosa JA, Limas CJ: Treatment of refractory heart failure with infusion of nitroprusside. N Engl J Med 291: 589, 1974 da Luz PL, Forrester JS, Wyatt HL, Tyberg JV, Chagrasulis R, Parmley WW, Swan HJC: Hemodynamic and metabolic effects of sodium nitroprusside on the performance and metabolism of regional ischemic myocardium. Circulation 52: 400, 1975 Guyton AC, Jones CE, Coleman TG: Graphical analysis of cardiac output regulation: In Circulatory Physiology: Cardiac Output and its Regulation, edited by Guyton AC, Jones CF, Coleman TG. Philadelphia, WB Saunders Co, 1973, pp 237-262 Guyton AC, Jones CE, Coleman TG: Cardiac output in heart failure: I. bilateral failure. In Circulatory Physiology: Cardiac Output and its Regulation, edited by Guyton AC, Jones CF, Coleman TG. Philadelphia, WB Saunders Co, 1973, pp 45 1-468 20. Guyton AC, Jones CE, Coleman TG: The pulmonary circulation in left sided heart failure. In Circulatory Physiology: Cardiac Output and its Regulation, edited by Guyton AC, Jones CF, Coleman TG. Philadelphia, WB Saunders Co, 1973, pp 473-475 21. Lindsey AW, Banahan BF, Cannon RH, Guyton AC: Pulmonary blood volume of the dog and its changes in acute heart failure. Am J Physiol 190: 45, 1957 22. Harlan JC, Smith EE, Richard TQ: Pressure-volume curves of systemic and pulmonary circuit. Am J Physiol 213: 1499, 1967 23. Caldini P, Permutt S, Waddell JA, Riley RL: Effect of epinephrine on pressure, flow, and volume relationships in the systemic circulation of dogs. Circ Res 34: 606, 1974 24. Charlier AA, Jaumin P, Pouleur H: Circulatory effects of deep inspirations, blocked expirations and constant positive pressure inflations at equal transpulmonary pressure in conscious dogs. J 337 Physiol (Lond) 241: 589, 1974 25. Pouleur H, Jaumin PM, Charlier AA: Pulmonary blood volume and haemodynamic changes during steady lung inflations in dogs. Acta Anaesth Scand 17: 253, 1973 26. Gregg DE, Fisher LC: Blood supply to the heart. In Handbook of Physiology. Circulation. Section 2, vol II, edited by Hamilton WF, Don P. Washington DC, Am Physiological Society, 1963, pp 1517-1584 27. Starling EG: Some points in the pathology of herat disease. Lancet 1: 652, 1895 28. Pouleur H, Covell JW, Ross J Jr: Effects of alteration of aortic input impedance on the force-velocity-length relationship in the intact canine heart. Circ Res 45: 126, 1979 29. Green JF: Pressure-flow and volume flow relationships of the systemic circulation of the dog. Am J Physiol 229: 761, 1975 30. Drees JA, Rothe CF: Reflex venoconstriction and capacity vessel pressure-volume relationships in dogs. Circ Res 34: 360, 1974 31. Rubin S, Misbach G, Lekven J, Parmley WW, Tyberg J: Volume and resistance changes of the peripheral circulation during nitroprusside infusion in the areflexic dog: role of the spleen. (abstr) Clin Res 26: 266, 1978 32. Tarazi RC, Justan HP, Bravo EL, Niarchos AP: Vasodilating drugs: contrasting haemodynamic effects. Clin Sci Mol Med 51: 575s, 1976 33. Trapold JH: Role of venous return in the cardiovascular response following injection of ganglion-blocking agents. Circ Res 5: 444, 1957 34. Pagani M, Vatner SF, Braunwald E: Hemodynamic effects of intravenous sodium nitroprusside in the conscious dog. Circulation 57: 144, 1978 35. Cohn JN, Taylor N, Vrobel T, Moskowitz R: Contrasting effects of vasodilators on heart rate and plasma catecholamines in patients with hypertension and heart failure. (abstr) Clin Res 26: 547, 1978 36. Sarnoff SJ, Berglund E: Pressure-volume characteristics and stress relaxation in the pulmonary vascular bed of the dog. Am J Physiol 171: 238, 1952 37. Shoukas AA, Sagawa K: Control of total systemic vascular capacity by the carotid sinus baroreceptor reflex. Circ Res 33: 22, 1973 38. Zucher IH, Gilmore JP: Atrial receptor discharge during acute coronary occlusion in the dog. Am J Physiol 227: 360, 1974 39. Guyton AC, Jones CE, Coleman TG: Effect on cardiac output of opening the chest. In Circulatory Physiology: Cardiac Output and its Regulation. Philadelphia, WB Saunders Co, 1973, pp 432-433 40. MacGregor DC, Covell JW, Mahler F, Dilley RB, Ross J Jr: Relations between afterload, stroke volume, and descending limb of Starling's curve. Am J Physiol 227: 884, 1974 41. Ross J Jr, Braunwald E: Studies on Starling's law of the heart. IX. The effects of impeding venous return on performance of the normal and failing left ventricle. Circulation 30: 719, 1964 42. Ross J Jr: Afterload mismatch and preload reserve: a conceptual framework for the analysis of ventricular function. Prog Cardiovasc Dis 18: 255, 1976 43. Greenberg TT, Richmond WH, Stocking RA, Gupta PD, Meehan JP, Henry JP: Impaired atrial receptor responses in dogs with heart failure due to tricuspid insufficiency and pulmonary artery stenosis. Circ Res 32: 424, 1973 44. Higgins CB, Vatner SF, Eckberg DL, Braunwald E: Alterations in the baroreceptor reflex in conscious dogs with heart failure. J Clin Invest 51: 715, 1972 Effects of nitroprusside on venous return and central blood volume in the absence and presence of acute heart failure. H Pouleur, J W Covell and J Ross, Jr Downloaded from http://circ.ahajournals.org/ by guest on April 29, 2017 Circulation. 1980;61:328-337 doi: 10.1161/01.CIR.61.2.328 Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1980 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/content/61/2/328.citation Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation is online at: http://circ.ahajournals.org//subscriptions/