* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 16 Unit 3
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
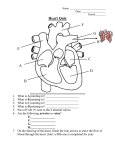
The Cardiovascular System: Blood Vessels and Circulation 16 Unit 3 Chapter 16 Blood Vessels • 16 Arteries- from heart • • Capillaries- thin walled for diffusion Veins- to heart 1. Venules => from capillaries 2. Veins from tissue to vena cavae to heart Unit 3 1. Elastic => large 2. Muscular => distribution to organs 3. Arterioles => distribution to capillaries- mostly muscle Figure 16.1ab Figure 16.1c Blood Vessel Structure 16 • Three layers • Arteries-> thicker tunica media • Veins- bigger lumen and thinner walls • Veins-> valves to prevent backflow Venules very thin, no valves Unit 3 Elastic tissue and/or muscle As they get smaller-> more muscle Arterioles-> very muscular- control • Muscular arteries & arterioles regulate flow • Sympathetic activity to smooth muscle vasoconstriction (narrowing) • Decreased sympathetic activity or NO causes relaxation or dilation • Arterioles adjust flow into capillaries • Systemic veins & venules serve as blood reservoirs (~64% total blood volume) 16 Unit 3 Vessel Functions Capillary Details 16 • Capillaries only have endothelium Very thin cells & cell nuclei protrude into lumen- easy diffusion Sometimes direct route from arteriole to venule • Filling controlled by small arterioles & precapillary sphincters Unit 3 • Connected from arterioles to venules in networks Figure 16.2a Figure 16.2b Capillary Exchange 16 • Slow flow through capillaries Allows time for exchange through wall • Blood pressure filtration of fluid out of capillary Mostly in first ½ of vessel length Reabsorption of fluid from outside to inside Mostly in last ½ of vessel length • Balance determines fluid in circulation Excess fluid returned via lymphatic system Local signals can adjust capillary flow Unit 3 • Osmosis (protein concentration) Figure 16.3 • Blood enters veins at very low pressure. • Needs more pumping to get back to heart • = action of heart; muscle pumps; respiratory pump • Some pressure from heart action • Not enough to overcome gravity 16 Unit 3 Venous Return • Contracting skeletal muscles squeeze veins emptying them • Because of venous valves flow is toward heart • Respiratory pump has similar action • Inhalation decreased thoracic pressure & increased abdominal pressure Blood flows toward heart • Exhalation allows refilling of abdominal veins 16 Unit 3 Muscle & Respiratory Pumps Figure 16.4 Blood Flow 16 • from high pressure area to lower pressure area, i.e. down pressure gradient Greater gradient greater flow • Ventricular contraction blood pressure (BP) • Resistance= opposition to flow • depends on lumen diameter & length & blood viscosity Smaller lumen greater resistance Higher viscosity greater resistance viscosity of blood depends on Hct Unit 3 Highest in aorta and declines as flows through vessels 110-70 mmHg in aorta ~16 mmHg at venules 0 at R. Atrium Resistance 16 • Depends on vessel lumen diameter Smaller lumen greater resistance • And blood viscosity Higher viscosity greater resistance viscosity of blood depends on Hct Longer the length of flow the more friction with wall Total body resistance increases with growth and addition of tissue Unit 3 • And total vessel length Anatomical Design 16 Unit 3 • Length and pressure • Design and local flow control- central pressure • Adult anatomy gives constant length • If central blood pressure is controlled it is constant • Only variable is radius of the arterioles • Each tissue can do it separately • Review design in picture below All tissues have the same pressure gradient 16 Unit 3 Pressure Gradients Pressure Gradients (Cont.) 16 • Note pulse in aorta & large arteries MAP • pressure fall related to resistance • Note low venous pressures can’t get back to the heart! Unit 3 Note role of arterioles Figure 16.5 • Fast responses: e.g. standing up • Slower responses: e.g. blood volume • Distribution: e.g. to working muscles • Balance of CO with flow to body • Interacts with many other control systems • Cardiovascular (CV) Center major regulator 16 Unit 3 Regulation of Blood Pressure & Flow Inputs 16 • Higher centers: • Sensory receptor input: proprioceptors, baroreceptors chemoreceptors Unit 3 cerebral cortex, limbic system, hypothalamus HR increases before race; flow adjusted for body temperature Inputs (Cont.) 16 • Proprioceptors: Start HR change as activity starts • Baroreceptors: in aorta & carotid • Chemoreceptors: in aorta & carotid Low O2, high H+, CO2 vasoconstriction BP Unit 3 pressure parasympathetic & sympathetic stimulation CO Figure 16.6 Output 16 • ANS to heart Sympathetic HR & force of contraction Parasympathetic HR to arterioles vasomotor tone To veins move blood to heart BP Unit 3 • Vasomotor Hormone regulation 16 • Renin-Angiotensin system Angiotensin II vasoconstriction+ thirst aldosterone Na+ & water loss in urine on constriction BP Thirst & water retention in kidney BP • ANP- from cells in atria Vasodilation & loss of salt & water in urine BP Unit 3 • Epinephrine & Norepinephrine CO • ADH = Vasopressin Figure 16.7 Checking Circulation- Pulse 16 • Pulse in arteries = HR • Tachycardia = rapid rest rate (>100 bpm) • Bradycardia= slow rest rate (<50 bpm) Unit 3 Use radial artery at wrist, carotid artery, brachial artery Blood Pressure 16 • Use sphygmomanometer Usually on brachial artery • Raise pressure above systolicstop flow • Lower pressure in cuff until flow just starts • Lower until sound suddenly gets faint Diastolic pressure • Normal values <120 mmHg for systolic & < 80 mmHg for diastolic Unit 3 first sound Systolic Pressure Circulatory Routes 16 • Two parts: Systemic & Pulmonary • Systemic circulation- throughout body • All systemic arteries branch from aorta • All systemic veins empty into Superior Vena Cava, Inferior Vena Cava or the Coronary Sinus Carry deoxygenated blood to heart Unit 3 Oxygenated blood deoxygenated as it goes Figure 16.8 Figure 16.9 Figure 16.10a Figure 16.10b Figure 16.10c Figure 16.11 Figure 16.12 Figure 16.13 Figure 16.14a Figure 16.14b Figure 16.14c Figure 16.15 Pulmonary Circulation 16 • From right ventricle pulmonary trunk • R. & L. pulmonary arteries Carry deoxygenated blood • R. & L. lungs • 2 R. & 2 L. pulmonary veins Carry oxygenated blood • L. atrium Unit 3 Gas exchange occurs • Portal vein transports blood from one capillary bed to another • GI organs • Splenic & superior mesenteric veins • hepatic portal vein • sinusoids in liver Mixes with oxygenated blood • hepatic vein inferior Vena Cava 16 Unit 3 Hepatic Petal Circulation Figure 16.16a Figure 16.16b Fetal Circulation 16 • Specialized for exchange of materials with maternal blood and bypass of lungs • Exchange in placenta umbilical vein • liver ductus venosus • inferior vena cava R. atrium • foramen ovale L. Atrium • Or R. Ventricle Pulmonary trunk ductus arteriosus aorta • internal iliacs umbilical arteries Placenta Unit 3 Mixes with deoxygenated blood from lower body Figure 16.17 • Umbilical arteries medial umbilical ligaments • Umbilical vein ligamentum teres • Ductus venosus ligamentum venosum • Placenta expelled • Foramen ovalis closes fossa ovale • Ductus arteriosus ligamentum arteriosum 16 Unit 3 At Birth Aging 16 • Stiffening of aortae • Loss of cardiac muscle strength • Coronary artery disease • Congestive heart failure • atherosclerosis Unit 3 Reduced CO & increased systolic pressure