* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ANPS 020 01-23
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Rheumatic fever wikipedia , lookup
Aortic stenosis wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Artificial heart valve wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
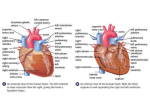
ANPS 020 Beneyto-Santonja 01/23/13 Anatomy of the Heart and the Conduction System The heart lies in the thoracic cavity, in the area called the mediastinum between the two lungs Note that the heart rests on the diaphragm The Heart The heart lies just to the left of midline, posterior to the sternum and ribs 2-4 The wide is located superiorly, and is attached by large blood vessels The pointed apex lies inferiorly, and rests on the diaphragm The heart is enclosed in a fibrous sac called the pericardial sac Within the fibrous sac, the heart is surrounded by the pericardial cavity The pericardial cavity is formed from a moist membrane The heart sticks to one side of this membrane, the visceral pericardium The rest of the pericardium sticks to the fibrous sac as the parietal pericardium The heart is not IN the cavity, but is surrounded by it on all sides There is no space in the cavity, but there is a thin layer of fluid that allows the visceral and parietal pericardial layers to slide against one another without friction as the heart fills and empties Pericarditis is a life-threatening condition Infection or inflammation within the pericardial cavity leads to swelling around the heart, and compression of the heart. This prevents the heart from adequately filling with blood, and effects it ability to pump. The heart has 4 chambers On the right side: Right atrium & Right ventricle On the left side: Left atrium & Left ventricle On each side, a valve separates the atrium from the ventricle: Atrioventricular valves (AV valves) Surface Anatomy of the Heart Atria are thin-walled, and have an expandable outer flap called the auricle most visible from the anterior view Ventricles are thick-walled The apex is the most inferior part of the left ventricle; the base is the superior end where the great vessels attach Grooves (sulci) separate the atria from ventricles Coronary arteries and veins travel in the surface grooves before entering the heart wall Coronary Arteries First branches from the aorta carry oxygenated blood to the heart tissue Right Coronary Artery supplies Right atrium, both ventricles, SA and AV nodes, and posterior wall Left Coronary Artery immediately splits into: o Circumflex Artery, which supplies left atrium, septum, and posterior wall o Left Anterior Descending (LAD) or Anterior Interventricular Artery, which supplies both ventricles anteriorly Arterial anastomoses interconnect anterior and posterior interventricular arteries to stabilize blood supply to cardiac muscle Coronary arteries lie in grooves in the heart surface The heart wall has 3 layers Endocardium: innermost; endothelium supported by connective tissue Myocardium: middle layer; cardiac muscle Epicardium: outer layer; connective tissue with fat, vessels, and visceral pericardium The left ventricle wall is thicker than the right The right ventricle is a low pressure pump The left ventricle is a high pressure pump The heart has TWO sets of valves Atrioventricular valves; between atria and ventricles o Right AV valve has 3 flaps: Tricuspid valve o Left AV valve has 2 flaps: Bicuspid valve, also called Mitral valve Semilunar valves o Leaving right ventricle: Pulmonary valve o Leaving left ventricle: Aortic valve Valves assure flow in one direction only The right side pump Blood enters the right atrium from the superior and inferior venae cavae. Venous blood returning from the heart wall empties directly into the right atrium Blood passes through the open tricuspid valve to enter the right ventricle Blood leaves the right ventricle through the pulmonary valve to enter the pulmonary trunk The pulmonary trunk branches into right and left pulmonary arteries, carrying blood to the lungs. The left side pump Blood returns from the lungs to the left atrium through the right and left pulmonary veins Blood passes through the open bicuspid valve to enter left ventricle Blood leaves the left ventricle through the aortic valve to enter the aorta The aorta gives off right and left coronary arteries before ascending to the aortic arch Anatomy of the AV Valves AV valves have fibrous flaps anchored by string-like chordae tendineae to muscular pegs protruding from ventricle wall – papillary muscles During the filling stage of the heart, AV valve flaps are pushed into the ventricle by the flow of blood. This is the “open” stage of the valve As the ventricle fills with blood, AV valve flaps float up on the column of the blood toward the atrium. As the ventricle contracts, the papillary muscles also contract, pulling on the chordae tendineae and preventing the flaps from swinging back into the atrium. This is the “closed” stage of the valve Anatomy of the Semilunar Valves A semilunar valve has 3 fibrous flaps attached to the wall of the vessel (aorta or pulmonary trunk); no muscles or chordae tendinae are involved with these passive valves Contraction of the ventricle creates enough pressure to push blood up out of the ventricle, pushing the semilunar valve flaps out of the way. This is the “open” stage of the valve As the ventricle relaxes, blood in the aorta or pulmonary trunk flows backward towards the ventricle and is “caught” on the valve flaps. This causes the valve flaps to balloon out as blood collects in the valve pockets. This is the “closed” stage of the valve. Two types of cardiac muscle cells in the heart Contractile Cells (99%) o Cardiac muscle cells which contract to push blood o The cells of the myocardium Pacemaker Cells (<1%) of the Conducting System o Specialized cardiac muscle cells; do not contract o Initiate and distribute action potentials that stimulate contraction o “autorhythmic” – heart beats on its own o Autonomic nervous system can regulate these cells to adjust heart rate with needs of the body The Conducting System of the Heart Pacemaker cells are specialized cardiac muscle cells Not Neurons Burried in the heart wall, so not visible at the gross level Pacemaker cells are leaky, and cannot maintain a stable resting potential They are slowly depolarize to threshold, then fire an action potential The rate of spontaneous depolarization determines the heart rate SA node generates 80-100 action potentials per minute o Fastest rate of firing, so drives all the other cells of conducting system at this rate AV node generates 40-60 action potentials per minute Anatomy of the Conducting System 1. Sinoatrial (SA) node a cluster of cells in the wall of the right atrium next to the superior vena cava a. Connected to the AV node b. Usually sets the rate of heart contraction c. Begins atrial contraction 2. Atrioventricular (AV) node a. A cluster of cells at the junction between the atria and ventricles receives electrical signal from SA node, slows impulse before passing it on 3. Bundle of His and bundle branches a. Fibers carrying impulse down septum between right and left ventricles 4. Purkinje Fibers a. Distribute throughout myocardium, from base upward in ventricle walls Disorders of the Conducting System Abnormal Pacemaker Function o Bradycardia: abnormally slow heart rate o Tachycardia: abnormally fast heart rate o Ectopic pacemaker Abnormal cells generate high rate of action potentials Bypass conducting system: don’t wait for signals through the regular pathway Disrupt ventricular contractions; ventricle may not contract bottom-to-top A pacemaker device may be implanted to regulate abnormal heart activity