* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
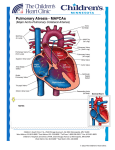
Download Left-to-Right Shunt Lesions
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
1 Chapter 18: Anesthesia for Left-to-Right Shunt Lesions Sabrina T. Bent, M.D., M.S. <h1> Introduction Left-to-right shunt lesions are the most common congenital heart defects, accounting for approximately 50% of all lesions, and are defined by a communication between the systemic and pulmonary circulations that allows shunting of better saturated (systemic) blood to the less saturated (pulmonary) circuit; whether the anatomic structures are located on the left or right side anatomically. For instance, a child with a ventricular septal defect and ventricular inversion will shunt blood from the systemic (right sided) ventricle to the lower pressure (left sided) ventricle. Left-to-right shunt lesions can be categorized on a physiologic basis according to the size of the defect and the resistance to blood flow. For example, shunting between high-pressure systems like the great arteries or ventricles is dependent upon the size of the defect and the ratio of pulmonary vascular resistance (PVR) to systemic vascular resistance (SVR). However, the amount of left-toright shunting through a lower pressure atrial septal defect is dependent upon the size of the defect and the relative compliance of the right and left ventricles. Because shunting occurs primarily with atrial contraction (i.e. during diastole and opening of the atrioventricular valves), the resistance is related to the diastolic compliance of the ventricles. 2 All left-to-right shunts produce a volume burden on the cardiovascular system. Shunting at the level of the great arteries results in increased pulmonary artery blood flow, increasing pulmonary venous return to the left atrium leading to increased left ventricular end-diastolic volume and left ventricular stroke work by the Frank-Starling mechanism. Shunting at the level of the great arteries produces a decrease in diastolic blood pressure from run off of blood into the low-pressure pulmonary circuit after closure of the aortic valve. Low diastolic pressures decrease coronary perfusion, potentially creating ischemia from the imbalance of decreased myocardial oxygen delivery and increased oxygen demand. Due to this volume burden, the left ventricle eventually will dilate and hypertrophy producing increased left ventricular end-diastolic pressure followed by increased left atrial pressure. The final result is pulmonary edema from pulmonary venous congestion and left heart failure. As pulmonary vascular resistance increases, there is an increased pressure burden on the right ventricle and eventual right heart failure. Shunting at the atrial or ventricular level, if large in size results in an increased right ventricular volume load in addition to the hemodynamic effects present with shunting at the great artery level. Prolonged exposure of the pulmonary vasculature to increased flow and pressure results in a fixed increase pulmonary vascular resistance. When pulmonary vascular resistance exceeds the systemic vascular resistance, shunt reversal occurs resulting in cyanosis and erythrocytosis known as Eisenmenger syndrome. Hemoglobin concentration is another contributing factor to the amount of left-to-right shunting. As the hemoglobin concentration increases blood viscosity will increase producing greater pulmonary and systemic vascular resistance; however the net effect is a reduction in left-to-right shunting. The physiologic decline in hemoglobin concentration in the first three months of life is thought to have a substantial role in the normal fall of pulmonary vascular resistance after birth. Figure 18.1 presents a schematic representation of the pathophysiology of the left-to-right shunting lesions. 3 The normal compensatory mechanisms that maintain systemic cardiac output and myocardial performance in the patient with a left-to-right shunt include the Frank-Starling mechanism, the sympathetic nervous system, and hypertrophy of the myocardium. Sweating and tachycardia are manifestations of these compensatory mechanisms in infants with left-to-right shunt lesions. Infants are typically tachypneic from decreased lung compliance associated with increased pulmonary blood flow. They do not feed well because of tachypnea and growth failure develops from both decreased caloric intake and increased caloric utilization. As noted above, significant left-to-right shunts induce biventricular failure. However, unlike adults, infants rarely manifest peripheral edema or jugular venous distension; the most consistent sign of right-sided failure is hepatomegaly. Anesthetic management for left-to-right shunt lesions should be individualized to the patient, but certain generalities do exist. Premedication with intravenous or oral drugs such as midazolam (0.05 - 0.1 mg/kg IV or 0.75- 1.0 mg/kg PO) can be safely administered decreasing anxiety and providing more controlled induction of anesthesia1. Standard ASA monitors along with use invasive arterial, central venous pressure, and urine output are recommend for all cases involving cardiopulmonary bypass. Transesophageal echocardiography, cerebral oximetry and cerebral blood flow monitoring are useful adjunctive monitors. (See Chapters 8 and 9 for more detailed discussion). Patients with severe, poorly controlled congestive heart failure may be intolerant to the myocardial depressant effects of inhalational anesthetics, and for this group of patients intravenous anesthesia with fentanyl and midazolam is preferred2 3,4. In most situations, however, inhalation induction with sevoflurane is a viable option when intravenous access is not initially available. Sevoflurane has been shown to better preserve myocardial function in patients with congenital heart disease as compared with halothane2. 4 Additional anesthetic issues include avoidance of air bubbles in intravenous lines to prevent paradoxical emboli. The anesthesiologist must be cognizant of the pulmonary vasodiltory effect of oxygen and hypocarbia and manipulate ventilation in order to balance the pulmonary and systemic vascular resistances. Such measures generally include minimizing the FiO2 and avoiding hyperventilation (PaCO2 between 40-50 mmHg). <h1> Patent Ductus Arteriosus The ductus arteriosus is an essential component in normal fetal circulation; it becomes functionally closed within 10-15 hours after birth, and permanently closes by thrombosis, intimal proliferation and fibrosis in the first 2-3 weeks after birth. Functional closure is initiated by several mechanisms including aeration of the lungs, removal of prostaglandins produced in the placenta, increased arterial PO2, and release of vasoactive substances (bradykinin, thromboxanes, and endogenous catecholamines) 5-7. Isolated persistent patent ductus arteriosus (PDA) occurs in approximately 1 in 2500 to 1 in 5000 live births, the incidence is higher for premature births and this defect is 2 - 3 times more common in females than in males5,8. PDA is also found as part of other complex congenital heart defects and is usually the source for pulmonary or systemic blood flow in patients with a functional single ventricle before palliative repair. <h2> Anatomy 5 Embrylogically, the ductus arteriosus arises from the distal portion of one of the sixth paired aortic arches5. The patent ductus arteriosus, is a vascular communication between the descending aorta and pulmonary artery. The PDA most commonly arises from the aorta, just distal to the left subclavian artery and attaches to the left pulmonary artery. (Figure 18.2). <h2> Pathophysiology and Natural History The degree of left-to-right shunting depends on several factors, the actual dimensions of the shunt as well as the relative ratio of pulmonary vascular resistance (PVR) and systemic vascular resistance (SVR). The shunt dimensions of importance include the diameter and length of the PDA, shorter connections with larger diameters produce less resistance, i.e. allow greater flow. In patients with large PDAs, the diastolic runoff into the pulmonary artery results in lowered aortic diastolic pressure, which may increase the risk of myocardial ischemia, especially in the presence of anemia or lowered SVR. The consequences of a PDA left untreated depend on many factors. A small PDA may be hemodynamically insignificant and unrecognized. The larger the PDA or left-to-right shunt, the more likely the progression to congestive heart failure, pulmonary hypertension, and in extreme cases, reversal of the shunt. In premature infants, PDA is associated with increased morbidity from associated respiratory distress syndrome, necrotizing entercolitis, and intracranial hemorrhage. <h2> Surgical Approaches 6 In newborns, surgical treatment is usually reserved for patients who fail medical treatment with indomethacin. The usual surgical options include posterolateral thoracotomy with ligation or division of the PDA or Video-Assisted Thoracoscopic Surgery (VATS). Surgical approaches have mortality approaching 0% and minimum morbidity, however, mortality rates in premature neonates is slightly higher6. Complications of surgical treatment include, bleeding, chylothorax, vocal cord paralysis (injury to recurrent laryngeal nerve), pneumothorax, atelectasis, recurrence of patency, and inadvertent ligation of the pulmonary artery or descending aorta6. VATS has increasing popularity due to decreased pain, decreased hospital cost (secondary to decreased hospital stay), and avoidance of post-thoracotomy syndrome (rib fusion, chest wall deformities, scoliosis, and compromise of pulmonary function). Disadvantages of VATS include intraoperative desaturations and hypercarbia, as well as higher morbidity during the surgical learning curve9-11. <h2> Transcatheter Closure Techniques Many catheter methods have been developed to nonsurgically close a PDA and include the Gianturco Coils, the Gianturco-Grifka coil bag and the Amplatzer Duct Occluder (not FDA approved) 8,12,13. These methods are considered safe, efficacious, and cost effective when compared to surgical closure. Risks of transcatheter approaches include arrhythmias, embolization of the device and incomplete closure12-14. In addition, there are size limitations in small infants. <h2> Anesthetic Considerations 7 The anesthetic management for PDA ligation depends upon factors such as patient's clinical condition, prematurity, coexisting disease, body weight, and surgical technique. Standard ASA monitors are used along with pulse oximetry of both upper and lower extremities will assist in detecting inadvertent ligation of the descending aorta. In addition, placing a non-invasive blood pressure cuff on both upper and lower extremites will assist in determining if the PDA ligation produced some degree of coarctation of the aorta. Large volume venous access (which may be a 22 or 24 ga IV in a premature infant) and forced air warming devices are also recommended. Among patients with coexisting disease, intra-arterial pressure monitoring provides a method of assessing arterial blood gases, electrolytes, hematocrit, and acid-base status. Neonatal patients commonly develop hemodynamic instability from exposure to inhaled anesthetics and benefit from an intravenous anesthetic technique using opioids such as fentanyl and possibly a benzodiazepine along with muscle relaxation. Fentanyl based anesthesia reduces the neonatal stress response and improves postoperative outcome15. Neonatal PDA ligation is often performed in the newborn intensive care unit to avoid the additional risks of transport, need for ventilator changes, and hypothermic exposure. High spinal anesthesia, caudal and thoracic epidural techniques have all been described as safe and producing faster recovery16. Lung isolation improves surgical exposure, especially for VATS surgical techniques, but may require ventilation with 100% inspired oxygen to maintain acceptable oxygenation. Prior to lung 8 isolation, efforts should be used to limit the degree of left-to-right shunting by maintaining or pulmonary vascular tone: minimize the FiO2 and maintain PaCO2 between 40-50. <h1> Aortopulmonary Window Aortopulmonary window (APW), also know as aortopulmonary septal defect is a rare congenital heart defect with an incidence of APW is approximately 0.1 to 0.6% of all congenital heart defects17,18. Fifty to eighty percent of patients with APW have associated defects including: patent ductus arteriosus (72%), right pulmonary artery from aorta (32%), anomalous origin of a coronary artery from the pulmonary artery (23%), ventricular septal defect (20%), agenesis of the ductus arteriosus (20%), and other lesions17,19. APW is thought to have separate embryologic etiologies accounting for the three morphologic subtypes described by Kutsche and Van Mierop. Nonfusion of the embryonic aortopulmonary and truncal septi is responsible for the first type, malalignment of the aortopulmonary and truncal septi results in the second type, and absence of the embryonic aortopulmonary septum leads to the third type17,20. <h2> Anatomy The basic anatomical defect in aortopulmonary window consists of a communication between the aorta and the pulmonary artery. Type I is a proximal defect midway between the semilunar valves and the bifurcation of the pulmonary arteries, Type II is a distal defect with ill-defined or absent posterior border and anomalous origin of the right pulmonary artery from the aorta, and Type III is a large defect combining the first two types17. (Figure 18.3) 9 <h2> Pathophysiology and Natural History The pressure gradient between the aorta and pulmonary artery will produce significant left-to-right flow depending upon the size of the defect and the relative resistances between the pulmonary versus systemic vascular. Coexisting associated cardiac anomalies may alter the pathophysiology. Irreversible pulmonary hypertension can develop as early as one year of age21, and if uncorrected, results in a 40% mortality in the first year of life19. A report of 20 patients from India, aged 2 to 38 years, found 29% of patients over the age of 15 years developed Eisenmenger's syndrome. <h2> Surgical Approaches A variety of surgical techniques have been described to separate the aorta and pulmonary artery and repair the remaining defect; however in general they include ligation and/or division with suture closure and patch closure18,19. The repair is usually performed via median sternotomy with the use of cardiopulmonary bypass and deep hypothermic circulatory arrest. Surgical repair of the aortic defect can be accomplished using a pulmonary artery flap with subsequent repair of the pulmonary artery with pericardial patch22,23. Care must be taken to explore and repair associated anomalies of the pulmonary and coronary arteries, and to repair coexisting cardiac abnormalities. Actuarial survival after repair of APW is approximately 90% at 1, 5, and 10 years19. Transcatheter closure of APW has been reported utilizing the Rashkind double umbrella as well as the Amplatzer occlusion device24,25. 10 <h2> Anesthetic Considerations The anesthetic management of APW is similar to that of truncus arteriosus. Younger patients may have considerable diastolic run-off from low pulmonary vascular resistance. Prior to cardiopulmonary bypass, efforts should focus on maintaining pulmonary vascular tone by lowering of the FiO2 and allowing the oxygen saturation to fall to levels between 80-85%, and by maintaining elevated PaCO2 thereby allowing respiratory acidosis to develop. Surgical snaring of the pulmonary artery prior to bypass is helpful. In patients undergoing later repair, after pulmonary vascular resistance is elevated, the anesthetic management should goal is to avoid increases in PVR. These patients are at risk to develop perioperative pulmonary hypertension, especially those with elevated PVR prior to surgical repair. The administration of inhaled nitric oxide as well as other maneuvers described above may be necessary to lower PVR. Those patients exhibiting signs of pulmonary hypertension should initially be maintained under deep sedation with or without neuromuscular blockade during the immediate postoperative periods (See Chapter 27). <h1> Atrial Septal Defects The right and left atriums are normally divided from fusion of two septa, the septum primum and the septum secundum. The septum primum develops during the fourth week and the septum secundum develops during the fifth week of gestation5. The septum secundum forms an incomplete partition and leaves an opening called the foramen ovale. The septum primum becomes the valve of 11 the foramen ovale5. Five different types of atrial septal defects exist, 1. Secundum, 2. Primum, 3. Sinus Venosus, 4. Patent Foramen Ovale (PFO), and 5. Coronary Sinus (Figure 18.4). Isolated atrial septal defects (ASD) are more common in females than males by a factor of 2:1. ASDs make up approximately 5 to 10 percent of all congenital heart defects with the secundum ASD comprising nearly 80 percent of ASD6. A probe patent foramen ovale is found in approximately 30 percent of normal adult hearts. ASD may be isolated or associated with other congenital heart defects, where it may be a life saving communication allowing mixing of blood between the pulmonary and systemic circulations, such as total anomalous pulmonary venous return, tricuspid atresia, and transposition of the great arteries. <h2> Anatomy <h3> Secundum Atrial Septal Defect The secundum ASD is contained within the area bordered by the limbus of the fossa ovalis26. It results from an abnormal reabsorption of the septum primum or defective formation or shortening of the septum secundum. Combinations of these abnormalities may contribute to large defects. <h3> Primum Atrial Septal Defect The primum ASD results from abnormalities in formation of the septum primum. It is frequently associated with atrioventricular canal (AVC) defects, especially the partial AVC that includes a 12 cleft in the anterior leaflet of the left atrioventricular valve. These AVC defects are due to defects in fusion of the endocardial cushions. <h3> Sinus Venosus Atrial Septal Defect Sinus venosus defects result from abnormal development of the septum secundum or the sinus venosus, the primitive venous collecting chamber. The most common type is located near the superior vena cava orifice and is associated with partial anomalous pulmonary venous return involving the right upper and middle pulmonary veins. Defects near the orifice of the inferior vena cava also exist and may involve partial anomalous pulmonary venous return of the right lower pulmonary vein6. <h3> Patent Foramen Ovale Patent foramen ovale (PFO) results from failure of fusion of the septum primum to the limbus of the septum secundum. PFO is normal during fetal life as blood passes from right-to-left bypassing the lungs in fetal circulation. Following birth, as the pulmonary vascular resistance drops and systemic vascular resistance increases, the foramen ovale closes, but may not fuse. <h3> Coronary Sinus Atrial Septal Defect Coronary Sinus ASD, also called an unroofed coronary sinus, results from an absence in the wall between the coronary sinus and the left atrium. This allows blood from the left atrium to drain into 13 the right atrium via the coronary sinus. Persistent left superior vena cava is also associated with this defect26. <h2> Pathophysiology and Natural History The amount of left-to-right shunting at the atrial level is dependent upon two factors, the size of the defect and the relative compliance of the right and left ventricles. Shunting occurs primarily during diastole, when the atria contract and atrioventricular valves open, and produces a volume burden on the cardiovascular system that is proportionate to the amount of shunting. See discussion in introduction. Isolated ASDs are usually asymptomatic in infants and during childhood despite the increased volume load on the right ventricle. Congestive heart failure usually occurs after the second or third decade of life due to chronic right ventricular volume overload.6 Pulmonary hypertension can occur in up to 13% of unoperated patients younger than 10 years of age however, progression to Eisenmenger Syndrome is unususal6. The increase in right atrial size may predispose to atrial arrhythmias, and patients with a QP: QS of 2:1 or less have an 11% incidence, whereas those with a Qp: QS of 3: 1 or greater have a 38% incidence of atrial arrhythmias27. An ASD is sometimes discovered during a neurologic work-up for transient ischemic attacks or strokes from paradoxical emboli26. <h2> Surgical Approaches Surgical repair of an ASD is usually recommended between the ages of 3 to 528. Spontaneous closure of small secundum type ASD can occur in up to 87% of infants in the first year of life6, and 14 controversy exists regarding the closure of small ASD that are asymptomatic. Conventional surgical treatment involves median sternotomy with the use of cardiopulmonary bypass to perform a primary repair or patch closure, with surgical mortality approaching 0%6. Sinus venosus defects are usually repaired using a patch to close the ASD and baffle the anomalous pulmonary veins to the left atrium. Many centers now favor minimally invasive surgery via a partial sternotomy29-31, because of the advantage of improved cosmetic result with similar morbidity and mortality to complete sternotomy. Postoperative dysrhythmias are reported in 23% of patients, and as many as 2% of patients may need a pacemaker following surgery6. <h2> Transcatheter Closure Techniques Transcatheter ASD closure in the cardiac catheterization laboratory has dramatically reduced the number of operative repairs. The CardioSEAL septal occluder (Nitinol Medical Technologies, Inc., Boston, MA) and the Amplatzer septal occluder (AGA Medical Corp, Golden Valley, MN) are the most common devices used13. These procedures are usually performed under general anesthesia with the use of transesophageal echocardiography to guide placement. However, new intracardiac echocardiography using intravascular 2-D imaging may eliminate the need for TEE and reduce the need for general anesthesia32. Transcatheter closure is safe, associated with decreased hospital stay, lack of a surgical scar, avoidance of cardiopulmonary bypass and limits the need for general anesthesia. Limitations to transcatheter closure of ASD is based on: patient size (large introducer sheaths), type of ASD (usually only PFO or secundum), and requires the presence of an adequate tissue rim for the device to attach. 15 <h2> Anesthetic Considerations Patients with ASD are generally asymptomatic, and do not have pulmonary hypertension. Therefore, the induction of anesthesia can be easily tailored to either inhalation or intravenous technique. Whenever possible, patients should have an intraoperative transesophageal echocardiography (TEE) performed prior to incision, because transthoracic echocardiographic studies are sometimes unable to visualize all four pulmonary veins thereby excluding the possibility of partial anomalous pulmonary venous return. During surgery, TEE can be helpful to assess deairing of the left heart and adequacy of the repair. The majority of patients have good myocardial function and do not require inotropic support perioperatively. Maintenance of anesthesia may consist of inhaled agents, intravenous agents, regional anesthesia, or a combination. Regional techniques are favored by some to assist in early extubation33,34. Tracheal extubation in the operating room has been shown to decrease patient charges, without compromising patient care when compared to extubation in the intensive care unit.35 Whatever technique is chosen, the primary goal for the uncomplicated ASD patient should include preparation for an early extubation either in the operating room or within the first four hours postoperatively. <h1> Ventricular Septal Defects Ventricular septal defect (VSD) is the most common congenital heart defect, comprising approximately 20% of all congenital heart defects, with an incidence between 2.6 to 5.7 in 1000 live births36-38. VSD is associated with a variety of inherited conditions, including Trisomy 13, 18, and 21 as well as VACTERL association and CHARGE syndrome.39 VSDs are found as isolated 16 defects and as part of other complex congenital heart defects. Embrylogically, the primitive left ventricle is formed from the ventricular portion of the bulbis cordis and the primitive right ventricle is formed from the proximal portion at approximately 23 to 25 days' gestation. A communication between the right and left ventricles defines a VSD and five different types of VSD exist, 1. Perimembranous, 2. Subpulmonary, 3. Muscular, 4. Malalignment and 5. Canal (Figure 18.5). <h2>Anatomy <h3> Perimembranous Ventricular Septal Defect The perimembranous VSD is a communication adjacent to a portion of the membranous septum and the fibrous trigone of the heart, where the aortic, mitral, and tricuspid valves are in fibrous continuity with the tricuspid, aortic and mitral valves6. These infracristal defects are the most common VSD subtype, occurring in approximately 80%. <h3> Subpulmonary Ventricular Septal Defect The subpulmonary VSD is located within the outlet septum, above the crista supraventricularis, and border of the semilunar valves; and comprises approximately 5% of all VSDs. As a result of the location of this defect, a Venturi effect may be produced by the jet of blood flowing through the VSD causing the right or noncoronary aortic cusp of the aortic valve to prolapse toward the defect producing aortic insufficiency6. This type of lesion is more common in the Asian population40. 17 <h3> Muscular Ventricular Septal Defect Muscular VSDs are located within the muscular portion of the interventricular septum. These defects can be multiple and represent approximately 2 to 7% of VSDs. <h3> Malalignment Ventricular Septal Defect Malalignment VSDs occur from malalignment of the infundibular septum and the trabecular muscular septum. These defects usually occur as a component of a more complex cardiac defect, most commonly tetralogy of Fallot6. <h3> Canal Type Ventricular Septal Defect Canal type VSDs are located in the posterior region of the septum beneath the septal leaflet of the tricuspid valve32. These inlet defects accounts for approximately 10% of VSDs. <h2> Pathophysiology and Natural History Isolated VSDs produce left-to-right shunting at the ventricular level, predominantly during systole. The term restrictive refers to a limitation in the amount of flow across the defect based on size; and in this case a pressure gradient exists between the left and right ventricles. An unrestrictive VSD has flow limited only from the relative pulmonary to systemic vascular resistance; and therefore, no pressure gradient exists between the left and right ventricles. Fifteen percent of patients with large 18 VSDs develop pulmonary hypertension which will progress to the development of pulmonary vascular obstructive disease by the age of twenty41. Symptoms range from asymptomatic to signs and symptoms of congestive heart failure. The rate and degree of progression of symptomatology depends on the patient age, size of the defect and the degree of left-to-right shunting. Infants who have unrestrictive VSDs develop symptoms of CHF in the first three months of life because of the physiologic decline in pulmonary vascular resistance. Spontaneous closure of small perimembranous and muscular VSDs occurs in as many as 50% of patients41-43, and such patients are typically asymptomatic. <h2> Surgical Approaches Surgical repair of VSD usually involves patch closure or occasionally by primary closure using cardiopulmonary bypass via median sternotomy. Perimembranous and canal type VSDs are most commonly repaired via a right atriotomy which may require detachment of the septal leaflet of the tricuspid valve for exposure. Subpulmonary VSDs are most commonly repaired via the transpulmonary approach. Midmuscular VSDs are most commonly repaired via right atriotomy, and anterior or apical muscular VSD may be approached using right ventriculotomy. However the use of right ventriculotomies carries the risks of conduction disturbances and ventricular dysfunction later in life. At our institution, symptomatic patients with lesions that are not approachable via right atriotomy are usually treated with pulmonary artery banding until the patient is larger allowing transatrial repair. Pulmonary artery banding is also utilized for multiple muscular VSDs and in patients that are high-risk candidates for cardiopulmonary bypass. Partial median 19 sternotomies as well as small right anterolateral thoracotomies are advocated by some because of improved cosmetic results44,45. Video-Assisted Cardioscopy (VAC) is used in some centers to improve visualization of small intracardiac structures in limited spaces during open heart surgery for congenital heart repairs31,46-48. VAC has been successfully utilized for a variety of intracardiac repairs including ASD, VSD, Tetralogy of Fallot, double outlet right ventricle, atrioventricular canal and others. Timing for surgical repair varies depending on age, signs and symptoms. Patients less than 6 months of age are repaired if they manifest uncontrollable congestive heart failure and failure to thrive. Patients between 6 to 24 months of age undergo repair to treat congestive heart failure symptoms or pulmonary hypertension. Patients older than 24 months undergo repair for Qp: Qs > 2:1. Among patients with subpulmonary VSD, the presence of aortic insufficiency is an indication for surgical repair to prevent further progression of the valvular insufficiency49,50, A defect size ( 5 mm is repaired to avoid progression to aortic cusp prolapse and aortic insufficiency, and defects ( 5mm can be managed conservatively40. Mortality for uncomplicated VSD in older patients is less than 1 to 2 %. 51 Mortality for VSD repair in infants during the first year of life is less than 5%52. <h2> Transcatheter Closure Techniques Transcatheter closure of muscular VSDs has been performed successfully53-56. The use of the CardioSEAL septal occluder (Nitinol Medical Technologies, Inc., Boston, MA) is approved for use 20 in the United States, and the Amplatzer septal occluder (AGA Medical Corp, Golden Valley, MN) is undergoing clinical trials in the United States. Indications for use of the devices include all types of muscular VSDs, including apical and multiple. Transcatheter techniques may serve as an adjunct to surgery or an alternative to surgery in selected patients. Intraoperative use of VSD closure devices during cardiopulmonary bypass for defects with difficult surgical closure has been described57, and postoperative residual VSDs or "swiss cheese" type muscular VSD may be preferentially treated by this technique. The major limitation in the application of this technique is related to the size of the sheaths necessary for device delivery, precluding use in infancy. Complications of device closure include need for blood transfusion, tricuspid valve regurgitation, and device embolization53,55. <h2> Anesthetic Considerations Anesthetic management for the patient with VSD is similar to that of ASD. Pulmonary hypertension may develop early, especially in patients with trisomy 21, and preoperative chest xray revealing decreased pulmonary vascular markings is indicative of pulmonary hypertension58-61. Such patients may respond to the use of inhaled nitric oxide prior to termination of cardiopulmonary bypass and/or in the post-operative period. Right heart failure with decreased cardiac output may result if pulmonary hypertension is not controlled, and is improved from the use of dopamine, milrinone, dobutamine, or isoproterenol. Conduction disturbances, particularly atrial-ventricular heart block may be transient or permanent and is reported to occur in up to 10% of patients post-VSD repair6; however the experience at 21 Texas Children's Hospital is less than 1% of patients require permanent pacing after VSD closure. If heart block develops, treatment with atrioventricular synchronous pacing using temporary pacing wires is indicated. Junctional ectopic tachycardia is sometimes observed in patients less than one year of age after repair for lesions that involve VSD repair, most commonly after tetralogy of Fallot repair. Treatment includes cooling to 35o C, increased anesthetic depth, paralysis, procainamide, esmolol, or amiodarone6. Intraoperative use of transesophageal echocardiography will help recognize residual VSDs, intracardiac air and assess ventricular volume and function. Small muscular VSDs will become apparent after closure of larger VSDs. Frequently these smaller defects, especially if near the apex, may not be amenable to surgical repair or worth the risk of returning to cardiopulmonary bypass. Patients with uncomplicated VSDs are good candidates for extubation in the operating room or early after arrival in the intensive care unit. <h1> Common Atrioventricular Canal Common atrioventricular canal (CAVC) results from failure of the endocardial cushions to fuse during the fifth week of fetal development5. Four to five percent of congenital heart disease involves defects of the atrioventricular septum, and CAVC defects occur in 0.19 in 1000 live births7,62. CAVC is associated with multiple syndromes and occurs in approximately 20 % of persons with Trisomy 21; accounts for 15% of congenital heart defects in persons with Noonan's syndrome, and nearly 50% in persons with Ellis-van Creveld63. 22 <h2>Anatomy Anatomically, CAVC consist of three basic defects: 1. ostium primum defect resulting in an interatrial communication, 2. abnormal atrioventricular valves, and 3. inlet VSD resulting in an interventricular communication.36 Three types of CAVC exists, 1. partial, 2. transitional, and 3. complete. <h3> Partial Atrioventricular Canal The partial atrioventricular canal defect consists of an interatrial communication or ostium primum defect and a cleft in the anterior leaflet of the mitral valve, usually resulting in some degree of insufficiency. The tricuspid valve is often abnormal as well, and no interventricular communication exists. <h3> Transitional Atrioventricular Canal The transitional atrioventricular canal defect consists of an ostium primum defect, abnormal atrioventricular valve, which may be partially separated into two valves, and usually a small or moderate interventricular communication that may be partially closed by bridging tissue of the atrioventricular valve to the crest of the ventricular septum6,26. Like the partial atrioventricular canal defect, the left atrioventricular valve is usually associated with a cleft and has some degree of insufficiency. 23 <h3> Complete Atrioventricular Canal The complete atrioventricular canal defect usually consists of a large nonrestrictive ostium primum and interventricular septal defect as well as a large common single atrioventricular valve. The left atrioventricular portion of the valve usually contains a cleft that is insufficient. Three classifications of the CAVC defects exist based on the chordal attachments of the anterior bridging leaflet of the common atrioventricular valve, and are commonly referred to as Rastelli Type A, B and C64 In Rastelli type A, the anterior leaflet is attached to the crest of the ventricular septum by thin chordae tendinae. The interventricular communication is present above the crest of the ventricular septum and between the anterior and posterior bridging leaflets, and the VSD does not extend to the aortic cusps. The left ventricular outflow tract is narrowed and elongated with this defect26. The Rastelli type B is characterized by the anterior leaflet attachment via chordae tendinae to a papillary muscle in the right ventricle near the septum. The interventricular communication is below the common valve and extends to the aortic valve cusps. This defect is also associated with a narrowed and elongated left ventricular outflow tract26. The Rastelli type C is defined by an anterior leaflet that lacks any ventricular septal attachments and "floats" above the septum. The interventricular communication lies below the atrioventricular valve and extends to the aortic cusps. As in the other Rastelli subtypes, the left ventricular outflow tract is narrowed and elongated. The Rastelli type C defect is most common type, and may be associated with other major cardiac or extracardiac anomalies such as tetralogy of Fallot or Trisomy 2126. 24 Other variants of atrioventricular canal also exist, including right or left ventricular dominant types in which one ventricle is hypoplastic. The physiology produced by such lesions are similar to other single ventricle lesions, and the reader is referred to Chapter 22. Multiple other associated lesions may also occur including patent ductus arteriosus, tetralogy of Fallot, coarctation of the aorta, subaortic stenosis, left superior vena cava, asplenia and polysplenia6. <h2> Pathophysiology and Natural History A left-to-right shunt may occur at the atrial, ventricular, and atrioventricular valvar level, depending on the type of atrioventricular canal present. This shunting, in addition to atrioventricular valve regurgitation, results in volume overload of both the atria and ventricles. Volume overload soon develops into congestive heart failure and may result in pulmonary hypertension as the ratio of pulmonary to systemic blood flow increases. As with other left-to-right shunts, pulmonary hypertension may develop by one year of age and eventually lead to Eisenmenger's syndrome65. The severity of congestive heart failure and symptoms will depend on the degree of left-to-right shunting and the severity of atrioventricular valvar regurgitation with partial atrioventricular canal being the least symptomatic followed by transitional, and then complete being the most symptomatic of the three. Patients with partial atrioventricular canal if left untreated, may do well through childhood, but have increased likelihood of developing congestive heart failure in adulthood especially as atrial dysrhythmias develop26. The presence of moderate to severe atrioventricular valvar regurgitation leads to earlier development of congestive heart failure and higher morbidity and mortality if untreated26. Those patients with PAVC presenting with CHF in the first year of life should be suspected of having additional lesions, most commonly left sided 25 obstructive lesions66. Patients with CAVC develop congestive heart failure, failure-to-thrive, and frequent respiratory infections in the first year of life, and those with trisomy 21 develop pulmonary hypertension earlier and with increased severity as compared to other children. Twelve percent of children with CAVC develop irreversible pulmonary hypertension within the first year of life, and a chest radiograph demonstrating black lung fields, indicating decrease pulmonary blood flow, is an ominous sign58. <h2> Surgical Approaches Surgical repair of the partial atrioventricular canal (PAVC) is usually performed at age 2 to 5 years unless there are signs of congestive heart failure or other lesions which necessitate earlier repair. Patients with transitional atrioventricular canal (TAVC) may be relatively asymptomatic and may tolerate surgical repair at an older age. Primary complete surgical repair for patients with complete atrioventricular canal (CAVC) is performed between three to six months of age because it is safe, controls congestive heart failure, prevents the development of fixed pulmonary hypertension and reduces annular dilation (a cause of atrioventricular valvar regurgitation) 3,66,67. Surgical techniques vary, but generally consist of a right atriotomy with patch closure of the atrial septal defect, closure of clefts in the anterior leaflet of the left atrioventricular valve and the ventricular septal defect is closed with a patch or occasionally in the case of the transitional atrioventricular canal, pledgetted sutures6,26,67. A one or two patch technique can be used (Figure 26 18.6). Pulmonary artery banding is reserved for cases of severe respiratory illness, sepsis, or anatomy not suitable for biventricular repair. Presence of other associated cardiac anomalies such as tetralogy of Fallot, double outlet right ventricle, left sided obstructive lesions and unbalanced canals (hypoplastic ventricle), further complicate the repair and result in higher mortality, especially in the patients with a hypoplastic ventricle68,69. Mortality for repair of the partial atrioventricular canal is less than 5%, and the mortality for complete repair of CAVC is between 3 and 10.5 %6,70-72. Pulmonary artery banding is associated with mortality near 5%6,26. Presence of preoperative pulmonary hypertension and increasing size of the VSD is associated with higher morbidity and mortality among patients undergoing complete repair of CAVC26,70. <h2> Anesthetic Considerations Anesthetic management of the atrioventricular canal defects depends primarily on the degree of left-to-right shunting, and the presence and severity of pulmonary vascular hypertension. As with other septal defects, balancing the ratio PVR to SVR thereby limiting the amount of pulmonary overcirculation is paramount to successful management, and is usually accomplished by manipulations in FIO2 and ventilation. See discussion above. Transesophageal echocardiography is very helpful in detecting residual intracardiac shunts, assessing atrioventricular valvar function and determining ventricular function and volume following repair. 27 Surgical placement of left atrial and pulmonary arterial pressure lines may be used to guide management of inotropes, use of nitric oxide, and volume replacement. Persistent pulmonary hypertension and acute increases in pulmonary hypertension contribute to acute right heart failure and increased mortality6,70. Pulmonary hypertension commonly develops in these patients and is treated with hyperventilation, 100% oxygen, opioid anesthetics like fentanyl, systemic alkalinization and nitric oxide. Increasing the pH is more effective than lowering of the pCO2 in controlling pulmonary pressures and may be accomplished by the administration of sodium bicarbonate. Pulmonary hypertension that is refractory to nitric oxide may respond to magnesium sulfate, at initial doses of 20 mg/kg/hr, or magnesium chloride70. Most patients require inotropic support upon weaning from cardiopulmonary bypass, and those with residual atrioventricular valvar regurgitation and/or VSD benefit from use of milrinone or other afterload reduction. Hypotensive patients who have elevated left atrial pressures should be evaluated for the presence of severe residual left atrioventricular valvar regurgitation or stenosis, a residual VSD, left ventricular outflow tract obstruction, or left ventricular dysfunction6. Intraoperative transesophageal echocardiography is essential for initial diagnosis of these conditions, and re-initiation of cardiopulmonary bypass and repair may be necessary. CAVC repair is associated with conduction abnormalities, especially atrioventricular and sinoatrial nodal dysfunction resulting in complete heart block. In this situation, atrioventricular sequential pacing is necessary to minimize atrioventricular valvar regurgitation and to improve cardiac output6. <h1> Double Outlet Right Ventricle 28 Double outlet right ventricle (DORV) describes a spectrum of congenital heart defects, anatomically defined by having the origin of one great artery and the majority of the other great artery arise from the morphologic right ventricle73. DORV comprises approximately 1 to 1.5 % of all patients with congenital heart disease with an incidence estimated at 1 per 10,000 live births73. Trisomy 13 and trisomy 18 are associated with DORV73. DORV results from bulboventricular malformations with failure of proper alignment of the conotruncus with the ventricular septum73. Characterization of the anatomy of DORV is crucial in understanding the physiologic consequences as well in determining the surgical approach for palliation or correction. Complete characterization of the anatomy will include: 1. the relationship of the VSD to the great arteries; 2. the relationship of the great arteries with respect to one another; 3. the morphology of the ventricles and their outflow tracts; and 4. the presence of other associated anomalies73. DORV may also occur with an intact ventricular septum, but is extremely rare74. Four different anatomic types of DORV are defined based on the relationship of the VSD to the great arteries: 1. Subaortic VSD with or without pulmonary stenosis. 2. Subpulmonary VSD with or without subaortic stenosis and/or arch obstruction. 3. Doubly committed VSD and 4. Noncommitted VSD73 . Reinsert figure here <h2> Anatomy <h3> Double Outlet Right Ventricle with Subaortic Ventricular Septal Defect Subaortic VSD represents approximately 51- 56 % of DORV,74,75 and involves normally related great vessels where the aorta is posterior and rightward or when the aorta is anterior and leftward. 29 When this defect is associated with pulmonary stenosis, the resulting physiology is similar to tetralogy of Fallot. <h3> Double Outlet Right Ventricle with Subpulmonary Ventricular Septal Defect Subpulmonary VSD represents approximately 30 % of DORV75,76; the aorta is to the right and/or anterior to the pulmonary artery. This type is associated with left-sided obstructive lesions such as subaortic obstruction or coarctation of the aorta, but may also occur without aortic obstruction73. 73 The Taussig-Bing malformation is included in this classification and is defined as having a juxtapulmonary pulmonary, supracristal VSD, with absence of the superior aspect of the ventriculoinfundibular fold, bilateral conus or infundibulum and malposed great arteries, commonly side-by-side73,77. <h3> Double Outlet Right Ventricle with Doubly Committed Ventricular Septal Defect Doubly committed VSD represents approximately 3 % of DORV75,76. The doubly committed VSD results from the hypoplasia of the infundibular septum and variable degrees of override of the VSD by both great arteries73. <h3> Double Outlet Right Ventricle with Noncommitted Ventricular Septal Defect 30 Noncommitted VSD represents approximately 12 -17 % of DORV,74,75 and the VSD is an apical muscular or the membranous-inlet type. The VSD is remote from the great arteries and is most frequently associated with atrioventricular canal defects73. <h2> Pathophysiology and Natural History The pathophysiology of DORV is dependent on the specific anatomy of the lesion and degree of pulmonary versus aortic blood flow as well as the degree of mixing of pulmonary and systemic venous blood. Three basic physiologic subtypes are tetralogy of Fallot, large VSD, and transposition of the great arteries. DORV associated with pulmonary stenosis resembles the physiology of tetralogy of Fallot with varying degrees of cyanosis depending on the severity of pulmonic stenosis. The patients have right-to-left shunting across the VSD and may have hypercyanotic spells, polycythemia, and failure to thrive73. Although there is a fixed component of obstruction, pulmonary blood flow may vary due to alterations in pulmonary vascular resistance. Pulmonary stenosis is present in approximately 50% of patients with DORV73. Subaortic VSD without pulmonary stenosis and noncommitted VSDs produce physiology similar to that of a large VSD. Because the VSD is typically large, the degree of left-to-right shunting will depend upon the relative ratio of PVR to SVR. 31 Subpulmonary VSD without pulmonary stenosis usually produces physiology similar to transposition of the great arteries. Streaming of pulmonary venous blood to the pulmonary artery and systemic venous blood toward the aorta, results in a relative parallel circulation with variable degrees of mixing of oxygenated and deoxygenated blood. The patients can present early with both cyanosis and congestive heart failure followed by development of pulmonary vascular occlusive disease if left untreated. DORV may be associated with multiple other anomalies such as multiple VSD, atrioventricular septal defects, PDA, aortic arch obstruction, interrupted aortic arch, subaortic stenosis, hypoplastic ventricle, as well as mitral valvar abnormalities that may further affect the physiology75-79. <h2> Surgical Approaches The surgical approach to DORV varies depending on the type of DORV and the associated anomalies, and the preoperative delineation of anatomy is crucial to determine the operative strategy. However, echocardiography, angiography, and magnetic resonance imaging may still result in incomplete information due to the complexity and anatomic variations of this lesion78,80. Often times only intraoperative inspection of the heart by the surgeon leads to the definitive operative plan. Four surgical treatment options generally exist, 1. palliative procedures such as Blalock-Taussig shunts, coarctation repairs, and pulmonary artery banding. 2. intraventricular repair with a baffle from the left ventricle to the aorta, 3. intraventricular baffle from the left ventricle to the pulmonary artery followed by arterial switch, and 4. bi-directional cavopulmonary 32 shunt staged to the Fontan procedure (univentricular heart repair) 75-79; with the primary goal of achieving a biventricular repair when possible. The overall early mortality for the repair of DORV is approximately 9%75,76,79. Ten year survival is 81-86%75,76. Significant risk factors for early mortality include congenital mitral valve anomalies, side-by-side great arteries, multiple VSDs and age at operation < 1 month75-77. Staged operations to Fontan or univentricular repair has the lowest early mortality of all repairs even though this group of patients usually have more complex forms of DORV75. <h2> Anesthetic Considerations Anesthetic management varies greatly depending on the specific type of DORV and associated anomalies. Management of palliative procedures, such as modified Blalock-Taussig shunts is reviewed in Chapter 20. Patients with pulmonary stenosis who present with physiology similar to tetralogy of Fallot should be managed to minimize the right-to-left shunting. See Chapter 20. Patients with subpulmonary VSD without pulmonary stenosis who have physiology similar to transposition of the great arteries should be managed as such. (Chapter 21). Patients with subaortic VSD without pulmonary stenosis, as well as the noncommitted VSD types present with physiology similar to that of a large VSD as described earlier in this chapter. Patients with complex DORV and other associated anomalies that proceed through the single ventricle staged palliation to the Fontan procedure are reviewed in Chapter 22. Common to all patients with DORV, intracardiac shunting must be balanced with manipulation of PVR and SVR to optimize systemic cardiac output and oxygen delivery. 33 Arrhythmias are common especially with repairs involving baffling and enlargement of the VSD. Ventricular tachyarrhythmias and complete heart block can occur in as many as 9% of patients postoperatively and may require permanent pacing73,75,76. Frequently, repair of DORV is complex and requires periods of circulatory arrest. Patients may have residual VSDs, valvar insufficiency, outflow tract obstruction, or ventricular dysfunction. Postoperative transesophageal echocardiography and left atrial pressure monitoring is helpful in determining the diagnosis and guiding management. <h1> Truncus Arteriosus Truncus arteriosus is an uncommon congenital heart defect representing less than 3% of all congenital heart defects6,81-83, and is defined by the presence of a single great artery arising from the base of the heart that supplies the coronary, pulmonary and systemic circulations and a ventricular septal defect. Embrylogically, this defect results from failure of the truncus arteriosus to divide into the aorta and pulmonary artery. Deletion of Chromosome 22q11 is present in approximately 11- 35% of patients with truncus arteriosus, and this chromosomal abnormality is associated with DiGeorge and velocardiofacial syndrome. Patients with these syndromes have other associated noncardiac anomalies such as aplasia or hypoplasia of the thymus and/or parathyroid glands (T-cell deficiency), hypocalcemia, palatal abnormalities, speech and learning disabilities, neuropsychological disorders and craniofacial dysmorhpia84-86. As many as 77% of patients with 22q11 deletion are immunocompromised86. 34 <h2> Anatomy Truncus arteriosus has been classified by two main systems, the first and most widely used classification system was initially described by Collett and Edwards in 1949 and the second by Van Praagh and Van Praagh in 196587,88. (Figure 18.7) The Collett and Edwards classification is based upon the embryologic arrested development of the pulmonary arteries from the sixth aortic arches and categorized into four different subtypes. <h3> Type I Truncus Arteriosus Type I truncus arteriosus accounts for 70% and is defined by the origin of the main pulmonary artery from the truncus dividing into left and right pulmonary arteries. <h3> Type II Truncus Arteriosus Type II truncus arteriosus accounts for 30% and is defined by separate origination of the left and right pulmonary arteries from the posterior surface of the truncus, with the branch pulmonary arteries arise very close to one another. <h3> Type III Truncus Arteriosus 35 Type III truncus arteriosus also has separate origination of the left and right pulmonary arteries, but in this case, the arteries arise from the lateral aspects of the truncus and are widely separated. This type accounts for approximately 1 % of cases. <h3> Type IV Truncus Arteriosus Type IV is not a form of truncus arteriosus, but is of historical note in the classification system. It is now defined as a variant of tetralogy of Fallot with pulmonary atresia. There is complete absence of the pulmonary arteries in this defect, with bronchial and collateral arteries of the descending aorta providing the blood supply to the lungs. Truncus arteriosus is most commonly associated with a ventricular septal defect, but intact septums can occur. The truncal valve may be abnormal with both abnormal numbers of leaflets, varying between two and six leaflets, as well as dysplastic6,88. Truncal valve insufficiency is estimated to occur in 25-50% of patients88. Anomalies of the coronary arteries may also exist. Additionally, truncus arteriosus is associated with other cardiac anomalies such as aortic arch obstruction, atrial septal defects (62%), right aortic arch (21-36%), aortic arch interruption (11-19%), patent ductus arteriosus (18%), aberrant subclavian artery (4-10%), absence of one pulmonary artery (10%), and persistent left superior vena cava (4- 9%)6,81,83. <h2> Pathophysiology and Natural History 36 Truncus arteriosus by definition has a common arterial trunk that provides blood flow to the coronary, pulmonary, and systemic arteries. As pulmonary vascular resistance falls in the early neonatal period, pulmonary blood flow progressively increases and results in congestive heart failure. A variable degree of mixing of the systemic and pulmonary venous blood occurs at the ventricular level through the ventricular septal defect. The large runoff provided by the pulmonary arteries results in low diastolic pressures, which may be worsened by the presence of truncal valve insufficiency. Low diastolic pressures in the face of increased myocardial work and increased ventricular pressures place the patient at risk of developing myocardial ischemia. Early congestive heart failure and increased pulmonary blood flow leads to rapid development of pulmonary vascular occlusive disease in infancy if left untreated. Patients without surgical treatment have a 74-100% mortality in the first year of life.80-82 Surgical repair in patients greater than two years of age is contraindicated when pulmonary vascular resistance is greater than 8 Wood units or in the presence of Eisenmenger's syndrome is present6,81. <h2> Surgical Approaches Definitive surgical repair is usually recommended in the neonatal period although some centers individualize patients, performing surgery between 2-3 months of age81-83,89. Early repair is indicated due to the rapid development of pulmonary hypertension and high mortality rate in patients in the first year of life if left untreated. Palliative surgery involving pulmonary artery banding has largely been abandoned except for those very few patients who are not suitable candidates for definitive repair83. Definitive surgical repair involves removal of the pulmonary 37 arteries from the truncal root and closing the resulting defect either primarily or with a patch. The VSD is usually closed via a transatrial or transventricular approach with a patch. A right ventricle to pulmonary artery connection is provided by a valved homograft. Direct anastomosis of the pulmonary artery with the right ventricle has been described, but may distort the pulmonary arterial architecture. A small ASD is sometimes created if high right ventricular pressures are anticipated in order to improve cardiac output at the expense of cyanosis6,81,82,89,90. This ASD creation can be closed at a later date by a transcatheter technique in the cardiac catheterization laboratory. Moderate to severe truncal valve regurgitation is repaired by valvuloplasty, "double-homograft" technique with coronary reimplantation, or mechanical valve implantation81,91,92. Valve repair has been successful even in neonates and avoids or delays serial truncal valve replacements91. Early mortality after repair of truncus arteriosus is 5-18%81,82,89,90, and mortality rates are higher among infants less than 3 kg, or from the presence of other associated cardiac anomalies82,89,92. <h2> Anesthetic Considerations Anesthetic management is dependent upon the patient's anatomy and age at presentation. Depending on the severity of congestive heart failure, the patient may require preoperative inotropic support, and the induction of anesthesia should be accomplished with drugs that maintain systemic vascular resistance (SVR) and preserve myocardial function. Therefore intravenous induction of anesthesia utilizing fentanyl and midazolam or etomidate with either vecuronium or pancuronium is ideal. Inhalational induction with careful titration of Sevoflurane should be performed with extreme caution. Doses of fentanyl exceeding 50 mg/kg is most commonly employed. Efforts to balance PVR and SVR to make the ratio of Qp: Qs approach unity is essential. 38 Care must be taken to avoid hyperventilation and excessive oxygenation which may result in lowering of pulmonary vascular resistance, further contributing to pulmonary overcirculation and lower diastolic blood pressure. Patients with truncal valvar insufficiency combined with excessive pulmonary blood run-off will be particularly susceptible to myocardial ischemia due to coronary hypoperfusion, and it may be necessary for the surgeon to temporarily place a vessel snare around the PA to limit pulmonary blood flow and increase diastolic blood pressure in the pre-bypass period. Those patients presenting late in infancy who have developed significant pulmonary hypertension from long-standing pulmonary overcirculation may require increased FiO2 to maintain oxygen saturations between 80 to 90%. Unless a chromosomal evaluation is known, patients with truncus arteriosus should be given irradiated blood products due to the high incidence of DiGeorge syndrome and associated T-cell deficiencies. Upon weaning from cardiopulmonary bypass most patients require inotropic support, afterload reduction, ventricular volume assessment, and efforts to minimize pulmonary arterial pressures in order to improve right heart function. Pulmonary hypertension is commonly present after cardiopulmonary bypass, and these patients have signs of right heart failure with high central venous pressures, desaturation, tachycardia, hypotension, acidosis, and oliguria.6 Management includes hyperventilation, 100 % oxygen, correction of acidosis, and nitric oxide as needed. These patients are usually kept sedated and paralyzed for at least 24 hours postoperatively to minimize early pulmonary hypertensive crises. Signs similar to right ventricular dysfunction may also occur from residual VSDs or truncal valve stenosis or regurgitation. VSD closure or right ventricular incision may produce complete right bundle branch block, complete heart block (3 -5%), junctional ectopic tachycardia, atrial tachycardias, and atrioventricular block in the postoperative period37. After bypass many patients 39 benefit from calcium infusions because of the hypocalcemia associated with DiGeorge syndrome, and citrate binding of ionized calcium from blood products administered. <h1> Partial and Total Anomalous Pulmonary Venous Return Partial and total anomalous pulmonary venous return (PAPVR and TAPVR) may be more appropriately defined as anomalous pulmonary venous connection. Since a patient may have normal pulmonary venous anatomy with presence of an atrial septal defect which allows abnormal return to the right atrium. PAPVR is defined as at least one pulmonary vein connected to the right atrium either directly or indirectly through a venous tributary93. In TAPVR, all of the pulmonary veins connect anomalously to the right atrium93. Both PAPVR and TAPVR are rare cardiac lesions with an incidence of approximately 0.6% and less than 5% of congenital heart disease respectively93-95. At 27-30 days of gestation, the pulmonary veins are derived from the splanchnic plexus which communicates with the cardinal and umbilicovitelline system of veins. Anomalous drainage to the left common cardinal system results in pulmonary venous connections to the coronary sinus or left innominate vein. Drainage to the right common cardinal system results in pulmonary venous connections to the superior vena cava and/or the azygous vein. Whereas, drainage to the umbilicovitelline system results in pulmonary venous connection to the portal vein, ductus venous or inferior vena cava93. Early atresia of the common pulmonary vein, while primitive pulmonarysystemic venous connections are still present results in TAPVR. If only the right or left portion of 40 the common pulmonary vein becomes atretic, persistence of the primitive pulmonary venoussystemic venous connection on that side leads to PAPVR93. Both PAPVR and TAPVR can be associated with other cardiac lesions. PAPVR is most commonly associated with sinus venosus type atrial septal defects. Congenital mitral stenosis, DORV, VSD, tetralogy of Fallot, coarctation of the aorta and patent ductus arteriosus have all been described with PAPVR93. Nearly 33% of patients with TAPVR have other associated anomalies, including single ventricle, CAVC, hypoplastic left heart, patent ductus arteriosus, and transposition of the great arteries. Abnormalities of the atrial and visceral situs with the heterotaxy syndrome, asplenia and polysplenia, are also common among patients with TAPVR.93 Scimitar syndrome which consists of either partial or complete anomalous drainage of the right pulmonary veins to the inferior vena cava, and sequestration of the right lower lobe producing a classic "scimitar" appearance on chest x-ray.6 <h2> Anatomy Multiple types of PAPVR exist. The most common is connection of the right pulmonary veins to the right superior vena cava or right atrium which represents approximately 74% of patients93. The next most common type is the right pulmonary veins to the inferior vena cava. The least common type is the connection of the left pulmonary veins to the left innominate vein or to the coronary sinus. Four different types of TAPVR exist based on the location of the anomalous connection (Figure 18.8). 41 <h3> Supracardiac Total Anomalous Pulmonary Venous Return Supracardiac connection comprises approximately 55% of cases of TAPVR93. In supracardiac TAPVR; the two pulmonary veins from each lung converge posterior to the left atrium. A vertical vein then arises from the left side of the confluence and usually passes anterior to the left pulmonary artery and the left mainstem bronchus to drain into the left innominate vein which then drains to the right superior vena cava93. Pulmonary venous obstruction is unusual, but may occur as a result of either intrinsic narrowing or extrinsic compression of the vertical vein. Although anomalous connection can occur to the right superior vena cava via a right-sided vertical vein, this is much less common93. <h3> Cardiac Total Anomalous Pulmonary Venous Return The cardiac type of TAPVR accounts for approximately 30% of cases. The pulmonary veins in the cardiac type develop a confluence at the coronary sinus or posterior to the right atrium. Obstruction to the pulmonary veins is uncommon, but may occur in up to 22% of TAPVR to the coronary sinus96. <h3> Infracardiac Total Anomalous Pulmonary Venous Return Infracardiac TAPVR comprises approximately 13% of cases, and is commonly referred to as infradiaphragmatic TAPVR93. This type of connection usually forms a confluence of pulmonary veins from both lungs posterior to the left atrium. A descending vein then courses anterior to the 42 esophagus through the diaphragm at the esophageal hiatus97. In 70-80% of patients, the descending vein joins the portal venous system at the splenic or the confluence of the splenic and superior mesenteric veins97. Nearly all of patients with infracardiac type of TAPVR have obstructed pulmonary veins, with the level of obstruction, either intrinsic or extrinsic, occurring at any location along the path. <h3> Mixed Total Anomalous Pulmonary Venous Return Mixed type of TAPVR makes up approximately 2% of cases. This type of TAPVR consists of anomalous connections at two or more levels. The most common connection involves the left pulmonary veins draining into the left innominate vein and the right pulmonary veins draining to the right atrium or the coronary sinus93. Obstruction to these pulmonary venous connections can occur. <h2> Pathophysiology and Natural History PAPVR results in a variable amount of left-to-right shunting that depends upon several factors: the number of anomalously draining veins as a percentage of the total pulmonary venous return, the pulmonary lobes or segments from which the anomalous veins originate from, and the relative resistances of the normally and anomalously drained pulmonary vascular beds and the compliance of the receiving chambers. The left-to-right shunt leads to increased pulmonary blood flow and enlargement of the right atrium and ventricle as well as dilation of the pulmonary artery93. 43 Most patients with an isolated single vein PAPVR and intact atrial septum are asymptomatic if left untreated and have normal life expectancy. Those patients with greater than 50% of the pulmonary veins draining anomalously or those with an associated atrial septal defect usually remain relatively asymptomatic until the third to fourth decades of life when progressive symptoms of dyspnea, recurrent bronchitis, hemoptysis, chest pain, and palpitations with supraventricular arrhythmias occurs. These patients may also present with right heart failure or with pulmonary hypertension and cor pulmonale93. The pathophysiology of TAPVR depends largely upon whether or not obstructed or unobstructed pulmonary venous return is present. In the presence of obstructed pulmonary veins, pulmonary venous hypertension exists with associated pulmonary edema. It is commonly confused with lung disease because of bilateral infiltrates secondary to pulmonary edema with a small heart size on chest x-ray. Pulmonary arteriolar vasoconstriction occurs as a compensatory mechanism to minimize the pulmonary edema. As pulmonary vascular resistance increases, the right ventricular systolic and end-diastolic pressures increase resulting in increased right atrial pressure and right-toleft shunting at the atrial level. Progressive systemic hypoxemia ensues with metabolic acidosis and multisystem organ failure. Left untreated, death occurs in the first few months of life6,93. In unobstructed TAPVR, the left-to-right shunt of pulmonary venous blood results in right atrial and ventricular enlargement with pulmonary overcirculation and subsequent right heart failure. The presence or absence of a restrictive interatrial communication is another major determinant in the pathophysiology of TAPVR, and 70- 80 % of infants have a patent foramen ovale which restricts filling of the left atrium and ventricle. The tremendous pulmonary overcirculation and right-sided 44 dilation and mimimal left-sided filling results in decreased size of the left atrium and ventricle. The abnormal displacement of the interventricular septum along with the chronic underfilling of the left ventricle leads to decreased systemic cardiac output. Symptomatic congestive heart failure usually develops in the second month of life and may be partially or totally relieved by transvenous balloon atrial septostomy93,98. Twenty percent of patients have an unrestrictive interatrial communication consisting of a secundum type atrial septal defect. These patients have a large left-to-right shunt with increased pulmonary blood flow, but may not develop signs of right heart failure or pulmonary hypertension until the third or fourth decade of life if left untreated93,98. <h2> Surgical Approaches Timing of surgical repair of PAPVR is dependent in part upon symptomatology. Patients with a single anomalous pulmonary vein with an intact atrial septum may never require surgical treatment. Surgical therapy is generally reserved for those patients with 1. hemodynamically significant leftto-right shunting with Qp:Qs greater than 2:1; 2. patients with recurrent pulmonary infections, especially those associated with Scimitar syndrome; 3. patients having surgical repair of other major cardiac lesions; and 4. patients with anomalous connections which affects surrounding structures by compression or obstruction93. Surgical repair for PAPVR varies depending on the specific anatomy present. The repair can consist of a direct anastomosis of the anomalous veins to the left atrium or an indirect communication is developed utilizing a patch to baffle the anomalous veins to the left atrium. 45 Obstructed TAPVR should be corrected emergently at time of diagnosis99. Patients with unobstructed TAPVR with restrictive interatrial communications may be palliated with blade and/or balloon atrial septostomies and medically managed for elective surgical repair in the first year of life. Those patients with nonrestrictive interatrial communications may be repaired electively, usually in the first year of life. Techniques for surgical repair of TAPVR depend upon the specific anatomy involved, and in some cases, a period of deep hypothermic circulatory arrest may be necessary. Surgical repair generally includes incision and enlargement of the anomalous pulmonary venous confluence and direct anastomosis with the left atrium. Occasionally, a patch is needed to baffle the veins to the left atrium. Operative mortality for repair of asymptomatic PAPVR should approach zero, and older symptomatic patients is less than 6%93,100. However, operative mortality for patients with TAPVR ranges from 8 to 13%, and TAPVR with heterotaxy approaches 100%93,95. <h2> Anesthetic Considerations The anesthesiologists' first encounter of the patient with PAPVR may be in the cardiac catheterization laboratory when scheduled for a transcatheter closure of an atrial septal defect, and the presence of an anomalous pulmonary vein is discovered, thereby preventing the utilization of the device. However, the first encounter with the patient with TAPVR may be in radiology, because an increasing number of newborns with suspected TAPVR, undergo magnetic resonance imaging 46 (MRI) which may be superior to echocardiography and angiography in the evaluation of TAPVR101,102. Intraoperative considerations for patients with PAPVR are similar to management of ASD, with increased pulmonary blood flow. Minimizing pulmonary blood flow by control of ventilation and consideration for early extubation following repair should be the primary goals. The pre-bypass management of the patient with obstructed TAPVR generally includes maximizing PO2, correcting metabolic acidosis, and maintening hemodynamic stability with use of inotropic medications as necessary. Transesophageal echocardiography is usually contraindicated due to risk of further compression and obstruction to pulmonary veins even in the presence of non-obstructed TAPVR. Perioperative monitoring of central venous, left atrial, and pulmonary arterial pressures is helpful for management. After bypass, nitric oxide should be used empirically in the case of obstructed TAPVR and should be readily available for immediate use in unobstructed TAPVR. Perioperative pulmonary hypertension occurs in as many as 50% of patients, and is a major risk factor for early mortality103,104. Pulmonary hypertensive crises may be avoided by employing hyperventilation, use of 100% oxygen, systemic alkalinization, sedation and paralysis along with nitric oxide. Magnesium sulfate and prostaglandin E1 have been used in some patients to treat severe pulmonary hypertension. Paradoxical pulmonary hypertension and systemic hypotension has been reported from the postoperative use of nitric oxide in patients with preoperative atrial obstruction and poorly compliant left ventricles with ventricular dysfunction. This paradoxical pulmonary hypertension is 47 thought to be due to acute increases in pulmonary blood flow and resultant preload to the noncompliant left side106. Pulmonary function may be compromised after bypass as a result of two pulmonary insults: 1) preoperative pulmonary edema secondary to pulmonary venous obstruction and 2) the inflammatory response from cardiopulmonary bypass. Pulmonary compliance is decreased and a large arterial-to-alveolar gradient develops. Pulmonary gas distribution may be optimized with the use of pressure control ventilation and altering PEEP to improve lung compliance. Following repair left atrial filling pressures following repair may be elevated due to the small size and noncompliant left ventricle. Accepting low blood pressures while weaning from cardiopulmonary bypass will help avoid overdistending the "unprepared" left side. Careful fluid management along with optimization of heart rate and rhythm and inotropic support will improve cardiac output. Perioperative dysrhythmias, especially supraventricular tachycardias, occur in as many as 20% of patients106. Optimize heart rate and rhythm with inotropic support and/or temporary pacing as needed. If tolerated an inovasodilator like milrinone will decrease left ventricular work and improve cardiac output. It is important to recognize that the Frank Starling curve is very flat in the small noncompliant LV and administration of only a few mls of fluid to an infant may cause the left ventricle to become overdistended and fail. <h1> Key Points for Anesthetic Management of Lesions 48 <h2> Patent Ductus Arteriosus 1. Avoid air bubbles in intravenous lines due to risk of paradoxical emboli. 2. Critically ill neonates may require a high dose narcotic technique to minimize the stress response to surgery. 3. Lung isolation is usually required for video assisted surgery to allow adequate surgical exposure. Aortopulmonary Window 1. Patients with pulmonary overcirculation should be managed to maintain pulmonary vascular tone. 2. Surgical snaring of the pulmonary artery can assist in increasing diastolic blood pressure and coronary perfusion. 3. Perioperative pulmonary hypertension frequently requires hyperventilation, 100% oxygen, systemic alkalinization, deep sedation, and paralysis. <h2> Atrial Septal Defects 1. Avoid air bubbles in intravenous lines due to risk of paradoxical emboli. 2. Tailor anesthetic techniques to allow early extubation. Ventricular Septal Defects 1. Maintain pulmonary vascular tone in those patients with pulmonary overcirculation prior to repair. 2. Diagnose and treat possible dysrhythmias, especially heart block, should be made. 49 3. Patients with uncomplicated VSDs should be considered for early extubation. <h2> Common Atrioventricular Canal 1. Maintaining pulmonary vascular tone is usually necessary. 2. Perioperative pulmonary hypertension frequently requires hyperventilation, 100% oxygen, systemic alkalinization, deep sedation, and paralysis. 3. TEE is helpful for post-repair assessments. 4. Inotropic support is frequently required with dopamine and/or milrinone. 5. Diagnose and treat dysrhythmias. <h2> Double Outlet Right Ventricle 1. Patients with physiology associated with pulmonary overcirculation should be managed by maintaining or increasing PVR. 2. Patients with physiology associated with inadequate pulmonary blood flow should be managed to improve pulmonary blood flow. 3. Perioperative pulmonary hypertension frequently requires hyperventilation, 100% oxygen, systemic alkalinization, deep sedation, and paralysis. 4. Diagnose and treat dysrhythmias. 5. Inotropic support is frequently required. <h2> Truncus Arteriosus 50 1. Patients with pulmonary overcirculation should be managed to maintain or increase PVR.. 2. Surgical snaring of the pulmonary artery can assist in increasing diastolic blood pressure and coronary perfusion. 3. Perioperative pulmonary hypertension frequently requires hyperventilation, 100% oxygen, systemic alkalinization, deep sedation, and paralysis. 4. High incidence of DiGeorge syndrome may require perioperative calcium infusions and use of irradiated blood products. 5. Inotropic support is frequently required perioperatively. <h2> Partial and Total Anomalous Pulmonary Venous Return 1. Maximizing oxygenation by mechanical ventilation, FiO2 = 1.0, hyperventilation and other maneuvers to decrease PVR, as well as inotropic support for cyanotic patients. 2. Perioperative pulmonary hypertension frequently requires hyperventilation, 100% oxygen, systemic alkalinization, deep sedation, and paralysis. 3. Avoid use of TEE which may worsen obstructed pulmonary veins and obstruct non-obstructive veins. 4. Avoid overfilling the left heart. 5. Inotropic support is frequently required perioperatively. 6. Diagnose and treat dysrhythmias. 51 Reference List 1. Levine MF, Hartley EJ, Macperson BA, Burrows FA, Lerman J. Oral midazolam premedication for children with congenital cyanotic heart disease undergoing cardiac surgery: a comparative study. Can J Anaesth 1993;40:934-938. 2. Rivenes SM, Lewin MB, Stayer SA, Bent ST, Schoenig HM, McKenzie ED, Fraser CD, Andropoulos DB. Cardiovascular effects of sevoflurane, isoflurane, halothane, and fentanylmidazolam in children with congenital heart disease: an echocardiographic study of myocardial contractility and hemodynamics. Anesthesiology 2001; 94: 223-229. 3. Hickey PR, Hansen DD, Wessel DL, Lang P, Jonas RA. Pulmonary and systemic hemodynamic responses to fentanyl in infants. Anesth Analg 1985; 64: 483-486. 4. Hickey PR, Hansen DD. Fentanyl- and sufentanil-oxygen-pancuronium anesthesia for cardiac surgery in infants. Anesth Analg 1984; 63: 117-124. 5. Moore KL. The Circulatory System, The developing human: clinically oriented embryology, sixth Edition. Philadelphia, Saunders, 1998, pp 298-343 6. Chang AC, Wells W, Jacobs J, Burke RP, Reddy M. Shunt Lesions In: Chang AC, Hanley FL, Wernovsky G, Wessel D. (eds.) Pediatric Cardiac Intensive Care. Baltimore, Williams & Wilkins, 1998, pp 201-232. 7. Allen HD. Moss and Adams' heart disease in infants, children, and adolescents: including the fetus and young adult. 6th Edn. Philadelphia, Lippincott Williams and Wilkins, 2001, pp 746-64 52 8. Mullins CE, Pagatto L. Patent Ductus Arteriosus. In: Garson JrA, Bricker JT, Fisher DJ, Neish SR. (eds.) The Science and Practice of Pediatric Cardiology. 2nd Edn. Baltimore, Williams & Wilkins, 1998, pp 1181-97 9. Lavoie J, Burrows FA, Hansen DD. Video-assisted thoracoscopic surgery for the treatment of congenital cardiac defects in the pediatric population. Anesth Analg 1996; 82: 563-567. 10. Shaw AD, Mitchell JB. Anaesthesia for video-assisted thoracoscopic patent ductus arteriosus ligation. Anaesthesia 1998; 53: 914-917. 11. Uezono S, Hammer GB, Wellis V, Boltz MG, Pike NA, Black MD. Anesthesia for outpatient repair of patent ductus arteriosus. J Cardiothorac Vasc Anesth 2001; 15: 750-752. 12. Radhakrishnan S, Marwah A, Shrivastava S. Non-surgical closure of large ductus arteriosus using Amplatzer Duct Occluder feasibility and early follow-up results. Indian J Pediatr. 2001; 68: 31-35. 13. Bilgic A, Celiker A, Ozkutlu S, Ayabakan C, Karagoz T, Ocal T. Transcatheter closure of secundum atrial septal defects, a ventricular septal defect, and a patent arterial duct. Turk J Pediatr. 2001; 43: 12-18. 14. Prieto LR, DeCamillo DM, Konrad DJ, Scalet-Longworth L, Latson LA. Comparison of cost and clinical outcome between transcatheter coil occlusion and surgical closure of isolated patent ductus arteriosus. Pediatrics. 1998; 101: 1020-1024. 15. Anand KJ, Sippell WG, Aynsley-Green A. Randomised trial of fentanyl anaesthesia in preterm babies undergoing surgery: effects on the stress response. Lancet 1987; 1: 62-66. 16. Williams RK, Abajian JC. High spinal anaesthesia for repair of patent ductus arteriosus in neonates. Paediatr Anaesth. 1997; 7: 205-209. 53 17. Wiggins JW. Aortopulmonary Septal Defect. In: Garson JrA, Bricker JT, Fisher DJ, Neish SR. The Science and Practice of Pediatric Cardiology. 2nd Edn. Baltimore, Williams & Wilkins, 1998, pp 1199-1205. 18. Tanoue Y, Sese A, Ueno Y, Joh K. Surgical management of aortopulmonary window. Jpn J Thorac Cardiovasc Surg 2000; 48: 557-561. 19. Tkebuchava T, von Segesser LK, Vogt PR. Congenital aortopulumonary window: diagnosis, surgical technique and long-term results. Eur J Cardiothorac Surg 1997; 11: 293-297. 20. Kutsche LM, Van Mierop LH. Anatomy and pathogenesis of aorticopulmonary septal defect. Am J Cardiol. 1987; 59: 443-447. 21. Blieden LC, Moller JH. Aorticopulmonary septal defect. An experience with 17 patients. Br Heart J 1974; 36: 630-635. 22. Di Bella I, Gladstone DJ. Surgical management of aortopulmonary window. Ann Thorac Surg. 1998; 65: 768-770. 23. Matsuki O, Yagihara T, Yamamoto F, Nishigaki K, Uemura H, Kawashima Y. As originally published in 1992: new surgical technique for total-defect aortopulmonary window. Ann Thorac Surg.1999; 67: 891. 24. Tulloh RM, Rigby ML. Transcatheter umbrella closure of aorto-pulmonary window. Heart 1997; 77: 479-480. 25. Richens T, Wilson N. Amplatzer device closure of a residual aortopulmonary window. Catheter Cardiovasc Interv. 2000; 50: 431-433. 26. Vick GW. Defects of the Atrial Septum Including Atrioventricular Septal Defects. In: Garson JrA, Bricker JT, Fisher DJ, Neish SR. The Science and Practice of Pediatric Cardiology. 2nd Edn. Baltimore, Williams & Wilkins, 1998, pp 1141-1179. 54 27. Sealy WC, Farmer JC, Young WG, Jr., Brown IW, Jr. Atrial dysrhythmia and atrial secundum defects. J Thorac Cardiovasc Surg. 1969; 57: 245-50 28. Reybrouck T, Bisschop A, Dumoulin M, van der Hauwaert LG. Cardiorespiratory exercise capacity after surgical closure of atrial septal defect is influenced by the age at surgery. Am Heart J. 1991; 122: 1073-1078. 29. Nicholson IA, Bichell DP, Bacha EA, del Nido PJ. Minimal sternotomy approach for congenital heart operations. Ann Thorac Surg. 2001; 71: 469-472. 30. Khan JH, McElhinney DB, Reddy VM, Hanley FL. A 5-year experience with surgical repair of atrial septal defect employing limited exposure. Cardiol Young. 1999; 9: 572-576. 31. Black MD, Freedom RM. Minimally invasive repair of atrial septal defects. Ann Thorac Surg. 1998; 65: 765-767. 32. Hijazi Z, Wang Z, Cao Q, Koenig P, Waight D, Lang R. Transcatheter closure of atrial septal defects and patent foramen ovale under intracardiac echocardiographic guidance: feasibility and comparison with transesophageal echocardiography. Catheter Cardiovasc Interv. 2001; 52: 194199. 33. Peterson KL, DeCampli WM, Pike NA, Robbins RC, Reitz BA. A report of two hundred twenty cases of regional anesthesia in pediatric cardiac surgery. Anesth Analg 2000; 90: 1014-1019. 34. Hammer GB. Regional anesthesia for pediatric cardiac surgery. J Cardiothorac Vasc Anesth 1999; 13: 210-213. 35. Laussen PC, Reid RW, Stene RA, et al. Tracheal extubation of children in the operating room after atrial septal defect repair as part of a clinical practice guideline. Anesth Analg 1996; 82: 988993. 36. Ventricular Septal Defect. MMWR Recomm Rep 1981; 30: 609-10 55 37. Mehta AV, Chidambaram B. Ventricular septal defect in the first year of life. Am J Cardiol. 1992; 70: 364-366. 38. Meberg A, Otterstad JE, Froland G, Sorland S, Nitter-Hauge S. Increasing incidence of ventricular septal defects caused by improved detection rate. Acta Paediatr. 1994; 83: 653-657. 39. Baptista MJ, Fairbrother UL, Howard CM, et al. Heterotrisomy, a significant contributing factor to ventricular septal defect associated with Down syndrome? Hum Genet. 2000; 107: 476482. 40. Lun K, Li H, Leung MP, et al. Analysis of indications for surgical closure of subarterial ventricular septal defect without associated aortic cusp prolapse and aortic regurgitation. Am J Cardiol. 2001; 87: 1266-1270. 41. Hoffman JI, Rudolph AM, Heymann MA. Pulmonary vascular disease with congenital heart lesions: pathologic features and causes. Circulation 1981; 64: 873-877. 42. Moe DG, Guntheroth WG. Spontaneous closure of uncomplicated ventricular septal defect. Am J Cardiol. 1987; 60: 674-678. 43. Ramaciotti C, Vetter JM, Bornemeier RA, Chin AJ. Prevalence, relation to spontaneous closure, and association of muscular ventricular septal defects with other cardiac defects. Am J Cardiol. 1995; 75: 61-65. 44. Murashita T, Hatta E, Miyatake T, Kubota T, Sasaki S, Yasuda K. Partial median sternotomy as a minimal access for the closure of subarterial ventricular septal defect. Feasibility of transpulmonary approach. Jpn.J Thorac Cardiovasc Surg. 1999; 47: 440-444. 45. Wang YQ, Chen RK, Ye WW, et al. Open-heart surgery in 48 patients via a small right anterolateral thoracotomy. Tex.Heart Inst.J. 1999; 26: 124-128. 56 46. Burke RP, Michielon G, Wernovsky G. Video-assisted cardioscopy in congenital heart operations. Ann Thorac Surg. 1994; 58: 864-868. 47. Rao V, Freedom RM, Black MD. Minimally invasive surgery with cardioscopy for congenital heart defects. Ann Thorac Surg. 1999; 68: 1742-1745. 48. Miyaji K, Hannan RL, Ojito J, Dygert JM, White JA, Burke RP. Video-assisted cardioscopy for intraventricular repair in congenital heart disease. Ann Thorac Surg.2000; 70: 730-737. 49. Ishikawa S, Morishita Y, Sato Y, Yoshida I, Otaki A, Otani Y. Frequency and operative correction of aortic insufficiency associated with ventricular septal defect. Ann Thorac Surg.1994; 57: 996-998. 50. Karpawich PP, Duff DF, Mullins CE, Cooley DA, McNamara DG. Ventricular septal defect with associated aortic valve insufficiency. Progression of insufficiency and operative results in young children. J Thorac Cardiovasc Surg. 1981; 82: 182-189. 52. Backer CL, Winters RC, Zales VR, et al. Restrictive ventricular septal defect: how small is too small to close? Ann Thorac Surg. 1993; 56: 1014-1018. 52. Hardin JT, Muskett AD, Canter CE, Martin TC, Spray TL. Primary surgical closure of large ventricular septal defects in small infants. Ann Thorac Surg. 1992; 53: 397-401. 53. Waight DJ, Bacha EA, Kahana M, Cao QL, Heitschmidt M, Hijazi ZM. Catheter therapy of Swiss cheese ventricular septal defects using the Amplatzer muscular VSD occluder. Catheter Cardiovasc Interv. 2002; 55: 355-361. 54. Hijazi ZM, Hakim F, Al Fadley F, Abdelhamid J, Cao QL. Transcatheter closure of single muscular ventricular septal defects using the amplatzer muscular VSD occluder: initial results and technical considerations. Catheter Cardiovasc Interv. 2000; 49: 167-172. 57 55. Lock JE, Block PC, McKay RG, Baim DS, Keane JF. Transcatheter closure of ventricular septal defects. Circulation 1988; 78: 361-368. 56. O'Laughlin MP, Mullins CE. Transcatheter occlusion of ventricular septal defect. Cathet.Cardiovasc.Diagn. 1989; 17: 175-179. 57. Okubo M, Benson LN, Nykanen D, et al. Outcomes of intraoperative device closure of muscular ventricular septal defects. Ann Thorac Surg. 2001; 72: 416-423. 58. Malec E, Mroczek T, Pajak J, Januszewska K, Zdebska E. Results of surgical treatment of congenital heart defects in children with Down's syndrome. Pediatr Cardiol. 1999; 20: 351-354. 59. Hasegawa N, Oshima M, Kawakami H, Hirano H. Changes in pulmonary tissue of patients with congenital heart disease and Down syndrome: a morphological and histochemical study. Acta Paediatr.Jpn. 1990; 32: 60-66. 60. Yamaki S, Horiuchi T, Sekino Y. Quantitative analysis of pulmonary vascular disease in simple cardiac anomalies with the Down syndrome. Am J Cardiol. 1983; 51: 1502-1506. 61. Chi TPL. The pulmonary vascular bed in children with Down syndrome. J Pediatr. 1975; 86: 533-538. 62. Eidem BW, Jones C, Cetta F. Unusual association of hypertrophic cardiomyopathy with complete atrioventricular canal defect and Down syndrome. Tex Heart Inst J 2000; 27: 289-291. 63. Marino B, Digilio MC, Toscano A, Giannotti A, Dallapiccola B. Congenital heart diseases in children with Noonan syndrome: An expanded cardiac spectrum with high prevalence of atrioventricular canal. J Pediatr. 1999; 135: 703-706. 64. Rastelli G, Kirklin JW, Titus JL. Anatomic observations on complete form of persistent common atrioventricular canal with special reference to atrioventricular valves. Mayo Clin Proc. 1966; 41: 296-308. 58 65. Newfeld EA, Sher M, Paul MH, Nikaidoh H. Pulmonary vascular disease in complete atrioventricular canal defect. Am J Cardiol. 1977; 39: 721-726. 66. Giamberti A, Marino B, di Carlo D, et al. Partial atrioventricular canal with congestive heart failure in the first year of life: surgical options. Ann Thorac Surg.1996; 62: 151-154. 67. Michielon G, Stellin G, Rizzoli G, Casarotto DC. Repair of complete common atrioventricular canal defects in patients younger than four months of age. Circulation 1997; 96: II-22. 68. Redmond JM, Silove ED, De Giovanni JV, et al. Complete atrioventricular septal defects: the influence of associated cardiac anomalies on surgical management and outcome. Eur J Cardiothorac Surg 1996; 10: 991-995. 69. Oshima Y, Yamaguchi M, Yoshimura N, Oka S, Ootaki Y. Anatomically corrective repair of complete atrioventricular septal defects and major cardiac anomalies. Ann Thorac Surg. 2001; 72: 424-429. 70. Schaffer R, Berdat P, Stolle B, Pfammatter JP, Stocker F, Carrel T. Surgery of the complete atrioventricular canal: relationship between age at operation, mitral regurgitation, size of the ventricular septum defect, additional malformations and early postoperative outcome. Cardiology 1999; 91: 231-235. 71. Hanley FL, Fenton KN, Jonas RA, Mayer JE, Cook NR, Wernovsky G, Castaneda AR. Surgical repair of complete atrioventricular canal defects in infancy. Twenty-year trends. J Thorac Cardiovasc Surg 1993; 106: 387-394. 72. Stark J, Gallivan S, Lovegrove J, et al. Mortality rates after surgery for congenital heart defects in children and surgeons' performance. Lancet 2000; 355: 1004-1007. 59 73. Silka MJ. Double-Outlet Ventricles. In: Garson JrA, Bricker JT, Fisher DJ, Neish SR. The Science and Practice of Pediatric Cardiology. 2nd Edn. Baltimore, Williams & Wilkins, 1998, pp 1505-1523. 74. Troise DE, Ranieri L, Arciprete PM. Surgical repair for double outlet right ventricle and intact ventricular septum. Ann Thorac Surg. 2001; 71: 1018-1019. 75. Kleinert S, Sano T, Weintraub RG, Mee RB, Karl TR, Wilkinson JL. Anatomic features and surgical strategies in double-outlet right ventricle. Circulation 1997; 96: 1233-1239. 76. Belli E, Serraf A, Lacour-Gayet F, et al. Biventricular repair for double-outlet right ventricle. Results and long-term follow-up. Circulation 1998; 98: II360-II365. 77. Takeuchi K, McGowan FX, Jr., Moran AM, et al. Surgical outcome of double-outlet right ventricle with subpulmonary VSD. Ann Thorac Surg. 2001; 71: 49-52. 78. Cil E, Ozme S, Saraclar M, et al. The angiocardiographic analysis of 73 patients with doubleoutlet right ventricle. Turk J Pediatr. 1997; 39: 27-33. 79. Belli E, Serraf A, Lacour-Gayet F, et al. Double-outlet right ventricle with non-committed ventricular septal defect. Eur J Cardiothorac Surg 1999; 15: 747-752. 80. Beekmana RP, Roest AA, Helbing WA, et al. Spin echo MRI in the evaluation of hearts with a double outlet right ventricle: usefulness and limitations. Magn Reson Imaging 2000; 18: 245-253. 81. Barbero-Marcial ML, Tanamati C. Repair of Truncus Arteriosus. Adv Card Surg. 1998, pp 4374. 82. Brown JW, Ruzmetov M, Okada Y, Vijay P, Turrentine MW. Truncus arteriosus repair: outcomes, risk factors, reoperation and management. Eur J Cardiothorac Surg 2001; 20: 221-227. 83. Williams JM, de Leeuw M, Black MD, Freedom RM, Williams WG, McCrindle BW. Factors associated with outcomes of persistent truncus arteriosus. J Am Coll Cardiol. 1999; 34: 545-553. 60 84. Goldmuntz E, Clark BJ, Mitchell LE, et al. Frequency of 22q11 deletions in patients with conotruncal defects. J Am Coll Cardiol. 1998; 32: 492-498. 85. Momma K, Ando M, Matsuoka R. Truncus arteriosus communis associated with chromosome 22q11 deletion. J Am Coll Cardiol. 1997; 30: 1067-1071. 86. Frohn-Mulder IM, Wesby SE, Bouwhuis C, et al. Chromosome 22q11 deletions in patients with selected outflow tract malformations. Genet Couns. 1999; 10: 35-41. 87. Collett RW, Edwards JE. Persistent Truncus Arteriosus: A Classification According to Anatomical Types. The Surgical Clinics of North America 1949; 29: 1245-1270. 88. Van Praagh R, Van Praagh S. The anatomy of common aorticopulmonary trunk (truncus arteriosus communis) and its embryologic implications. A study of 57 necropsy cases. Am J Cardiol. 1965; 16: 406-425. 89. Brizard CP, Cochrane A, Austin C, Nomura F, Karl TR. Management strategy and long-term outcome for truncus arteriosus. Eur J Cardiothorac Surg 1997; 11: 687-695. 90. McElhinney DB, Rajasinghe HA, Mora BN, Reddy VM, Silverman NH, Hanley FL. Reinterventions after repair of common arterial trunk in neonates and young infants. J Am Coll Cardiol. 2000; 35: 1317-1322. 91. Black MD, Adatia I, Freedom RM. Truncal valve repair: initial experience in neonates. Ann Thorac Surg.1998; 65: 1737-1740. 92. Rajasinghe HA, McElhinney DB, Reddy VM, Mora BN, Hanley FL. Long-term follow-up of truncus arteriosus repaired in infancy: a twenty-year experience. J Thorac Cardiovasc Surg 1997; 113: 869-878. 93. Ward KE, Mullins CE. Anomalous Pulmonary Venous Connections, Pulmonary Vein Stenosis, and Atresia of the Common Pulmonary Vein, In: Garson JrA, Bricker JT, Fisher DJ, Neish SR 61 (Eds.) The Science and Practice of Pediatric Cardiology, 2nd Edn. Baltimore, Williams & Wilkins, 1998, pp 1431-1461. 94. Wessels MW, Frohn-Mulder IM, Cromme-Dijkhuis AH, Wladimiroff JW. In utero diagnosis of infra-diaphragmatic total anomalous pulmonary venous return. Ultrasound Obstet Gynecol. 1996; 8: 206-209. 95. Boger AJ, Baak R, Lee PC, Boersma E, Meijboom FJ, Witsenburg M. Early results and longterm follow-up after corrective surgery for total anomalous pulmonary venous return. Eur J Cardiothorac Surg 1999; 16: 296-299. 96. Jonas RA, Smolinsky A, Mayer JE, Castaneda AR. Obstructed pulmonary venous drainage with total anomalous pulmonary venous connection to the coronary sinus. Am J Cardiol. 1987; 59: 431435. 97. Duff DF, Nihill MR, McNamara DG. Infradiaphragmatic total anomalous pulmonary venous return. Review of clinical and pathological findings and results of operation in 28 cases. Br Heart J 1977; 39: 619-626. 98. Ward KE, Mullins CE, Huhta JC, Nihill MR, McNamara DG, Cooley DA. Restrictive interatrial communication in total anomalous pulmonary venous connection. Am J Cardiol. 1986; 57: 1131-1136. 99. Burroughs JT, Edwards JE. Total Anomalous Pulmonary Venous Connection. Am Heart J 1960; 59: 913-931. 100. John Sutton MG, Tajik AJ, McGoon DC. Atrial septal defect in patients ages 60 years or older: operative results and long-term postoperative follow-up. Circulation 1981; 64: 402-409. 62 101. Masui T, Seelos KC, Kersting-Sommerhoff BA, Higgins CB. Abnormalities of the pulmonary veins: evaluation with MR imaging and comparison with cardiac angiography and echocardiography. Radiology 1991; 181: 645-649. 102. Choe YH, Lee HJ, Kim HS, Ko JK, Kim JE, Han JJ. MRI of total anomalous pulmonary venous connections. J Compu .Assist Tomogr. 1994; 18: 243-249. 103. Sano S, Brawn WJ, Mee RB. Total anomalous pulmonary venous drainage. J Thorac Cardiovasc Surg 1989; 97: 886-892. 104. Lincoln CR, Rigby ML, Mercanti C, Al Fagih M, Joseph MC, Miller GA, Shinebourne EA. Surgical risk factors in total anomalous pulmonary venous connection. Am J Cardiol. 1988; 61: 608-611. 105. Lin SC, Teng RJ, Wang JK. Management of severe pulmonary hypertension in an infant with obstructed total anomalous pulmonary venous return using magnesium sulfate. Int J Cardiol. 1996; 56: 131-135. 106. Raisher BD, Grant JW, Martin TC, Strauss AW, Spray TL. Complete repair of total anomalous pulmonary venous connection in infancy. J Thorac Cardiovasc Surg 1992; 104: 443438. 107. Cooley DA, Norman JC. Closure of patent ductus arteriosus. In, Cooley DA, Norman JC. Techniques in cardiac surgery. Houston, Texas, Texas Medical Press, 1975, pp. 10-17. 108. Chang AC, Wells W. Aorticopulomonary window. In Chang AC, Hanley FL, Wernovsky G, Wessel D, (eds). Pediatric Cardiac Intensive Care. Philadelphia, Lippincott, Williams, & Wilkins, 1998, pp. 201-2. 63 109. Cooley DA, Norman JC. Closure of atrial septal defect. In, Cooley DA, Norman JC. Techniques in cardiac surgery. Houston, Texas, Texas Medical Press, 1975, pp. 70-79. 110. Cooley DA, Norman JC. Closure of ventricular septal defect. In, Cooley DA, Norman JC. Techniques in cardiac surgery. Houston, Texas, Texas Medical Press, 1975, pp. 80-87. 111. Cooley DA, Norman JC. Repair of atrioventricularis communis. In, Cooley DA, Norman JC. Techniques in cardiac surgery. Houston, Texas, Texas Medical Press, 1975, pp. 88-93. 112. Hernanz-Schulman M, Fellows KE. Persistent truncus arteriosus. Pathologic, diagnostic and therapeutic considerations. Semin Roetgenol 1985;20:121-29. 113.Hanley FL. Total anomalous pulmonary venous connection. In, Kouchoukos NT, Blackstone EH, Doty DB, Hanley FL, Karp RB (eds). Kirklin/Barratt-Boyes Cardiac Surgery: 3ed. Churchill Livingstone, Philadelphia, 2003. pp. 753-779. Figure Legends 64 Figure 18.1. Pathophysiology of left-to-right shunting lesions. The flow diagram depicts factors that affect left-to-right shunting at the atrial, ventricular and great artery level and the pathophysiology produced by these shunts. A large shunt will result in LV failure, RV failure and pulmonary edema. Increased pulmonary blood flow and pulmonary artery pressures leads to pulmonary hypertension and eventually Eisenmenger’s syndrome. These final common outcomes, are highlighted in bold lettering. PVR, pulmonary vascular resistance; SVR, systemic vascular resistance; RV, right ventricle; LA, left atrium; LV, left ventricle; BP, blood pressure; RVEDV, right ventricular end-diastolic volume; RVEDP, right ventricular end-diastolic pressure; LVEDP, left ventricular end-diastolic pressure; LVEDV, left ventricular end-diastolic volume. See text for detailed discussion. Figure 18.2. Patent ductus arteriosus. Used with permission from Cooley et al107. Figure 18.3. Composite of the types of aortopulmonary window. A. Communication between the ascending aorta and main pulmonary artery. B. Communication between the aorta and both the main and right branch pulmonary artery. C. Right pulmonary artery originating separately from the aorta. Used with permission from Chang108. Figure 18.4. Composite of major types of atrial septal defect. See text for explanation. Used with permission from Cooley et al109. 65 Figure 18.5. Composite of major types of ventricular septal defect. Type I, subpulmonary; Type II, perimembranous; Type III, canal or inlet-type; Type IV, muscular. See text for further explanation. Used with permission from Cooley et al110. Figure 18.6. Single patch technique for repair of complete atrioventricular canal defect. Used with permission from Cooley et al111. Figure 18.7. Major classification systems for truncus arteriosus. Type I is the same as A1. Types II and III are grouped together as a single type A2. Type IV is a variant of Tetralogy of Fallot with pulmonary atresia and major aortopulmonary collaterals. Type A3 is unilateral pulmonary artery atresia with collateral supply to the affected lung. Type A4 is associatedw ith interrupted aortic arch. See text for full explanation. Used with permission from Hernanz-Schulman et al112. Figure 18.8. Four major subtypes of total anomalous pulmonary venous return. See text for further explanation. Used with permission from Hanley113.