* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Consequences of Untreated Ventricular Septal Defect
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Echocardiography wikipedia , lookup
Aortic stenosis wikipedia , lookup
Myocardial infarction wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
DiGeorge syndrome wikipedia , lookup
Turner syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Marfan syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
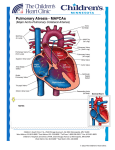
Consequences of Untreated Ventricular Septal Defect Norra Kwong, MD; Maya Mitchell, MD, FACP University of California, Davis Medical Center, Sacramento, CA Eisenmenger syndrome INTRODUCTION PATHOPHYSIOLOGY Eisenmenger syndrome is a triad of pulmonary vascular resistance and right-to-left shunting of blood with a systemic-to-pulmonary circulation connection and cyanosis. Although rare, patients with congenital heart disease can present in their adulthood. Primary care doctors need to recognize this syndrome and execute initial work-up since prognosis and quality of life is very poor when it is left untreated. CASE Cardiomegaly, prominent central pulmonary arteries with rapid tapering of distal pulmonary arteries. Right ventricle hypertrophy (R > S in V1, S > 7 mm in V5 or V6, Right Axis Deviation). RAE (P > 2.5 mm in II) DISCUSSION 40 year old female with Down syndrome presented with progressive shortness of breath, fatigue and altered mental status. RA Physical exam: BP 90/50, HR102, O2 sat 80% ►Lungs: scattered, bilateral rales. ►Heart: 3/6 harsh holosystolic murmur heard best at the apex radiating to the axilla. ►Extremities: clubbing, 2+ pitting edema up to knees bilaterally. 75% RA 76% LV 87% † ►Complications: Bleeding, thrombotic diathesis, stroke and bacterial endocarditis. Initial evaluation should include: Transesophageal Echocardiogram showed a large ventricular septal defect (VSD). Graph1: Testing for Reversibility of Pulmonary Vascular Resistance with Right Heart Cath Mean Pulmonary Arterial Pressure (mm Hg) Hospital course: ►Trial of inhaled nitric oxide (iNO) decreased the patient oxygen requirement. ►Cardiac Cath (Graph 1)– shows a persistent high pulmonary resistance despite increasing iNO. Patient is not a candidate for VSD closure and mitral valve repair. ►She was treated with Sildenafil and was placed on a waiting list for possible heart and lung transplant. ►Symptoms include: Central cyanosis, clubbing and exercise intolerance. RV RV LV Studies: Hematocrit of 58. ►Transthoracic echocardiogram (TTE): severe right ventricle hypertrophy, 4+ mitral regurgitation. EF 55-70%. ►Echocardiogram w/ bubble study: a right-to-left shunting. ►Transesophageal echocardiogram (TEE): 2.6 cm ventricular septic defect with bidirectional flow. A ventricular septal aneurysm and small secundum atrial septal defect is noted. 99% LA VSD LA Recognizing both cardiac and pulmonary symptoms in patients with risk factors for cardiac anomalies is very important. Patients with genetic disorders listed in Table 2 may have cardiovascular malformations that may not present until adulthood. 70 60 50 40 30 20 10 0 Favorable candidate for cardiac repair ( >10mm Hg drop and final PAP < 40 mm Hg w ith iNO) Our patient FiO2 40%, FiO2 100%, FiO2 100%, iNO 1ppm iNO 1ppm iNO 10 ppm Higher O2 sat in LA compared to LV indicated a possible shunt. Mosaic pattern shown bidirectional flow at VSD site. Table 2: Genetic disorders associated with cardiovascular malformations Down Syndrome Atrioventricular canal defect, mitral valve prolapse Turner Syndrome Bicuspid aortic valve, coarctation, aortic root dilation 22q11.2 deletion Truncus arteriosus, Tetralogy of Fallot Ehlers-Danlos Marfan Myotonic dystrophy Neurofibromatosis Tuberous sclerosis Cystic fibrosis Friedreich ataxia Rupture of large vessels Aortic aneurysm, AI, MVP Cardiomyopathy COA, renal artery stenosis Myocardial rhabdomyoma, WPW Cor pulmonale Cardiomyopathy ►Chest radiography, ECG, arterial oxygen saturations, exercise tolerance and echocardiography. ►TTE is often the initial test, but it is associated with low sensitivity for smaller defects. ►If suspicion for cardiac defect is high, TEE should be performed even with a negative TTE. ►Other diagnostic tools include: Echocardiogram with bubble study, cardiac catheterization, cardiovascular magnetic resonance imaging or computed tomography. Although prognosis for Eisenmenger syndrome is poor, emerging medications such as pulmonary vasodilating agents and advances in transplant technology may bring hope for these patients. REFERENCES: Additional reference is provided in a separate sheet.