* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Poster
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
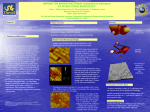
Glycoprotein VI: Thrombosis and Collagen Reaction Sheboygan North High School Colleen Anson, Matt Cain, Sam Ehrenreich, Otto Kletzien, Rachel Mayer, Mark Robitaille, Melanie Signer, Zhexi Wang, and Logan Vander Wyst Advisor: Ms. Amy Reinholtz Abstract GPVI Structure and Function Platelets normally circulate in the bloodstream in an inactive state. When a blood vessel is damaged and proteins in the extracellular matrix surrounding the blood vessel are exposed, platelets become activated, stick to one another to form a thrombus, and close up the wound. One of the major components of the extracellular matrix is collagen. Glycoprotein VI (GPVI) is a protein that plays a major role in allowing platelets to bind to and become activated by collagen. GPVI is embedded in the membrane of platelets; the extracellular region of GPVI is the section that binds to collagen, whereas the intracellular region is active in sending a signal to the inside of the platelet that enables the platelet to become activated. Activation of platelets by collagen can be beneficial during wound healing but, if platelets are activated and form a thrombus on the inside of a blood vessel, a heart attack or a stroke can result. An example of situation associated with clinical thrombosis complications is the use of coronary angioplasty to open up blocked blood vessels. Patients undergoing coronary angioplasty may have damaged artery walls with exposed collagen, which can cause excessive formation of thrombi that block the blood vessel up again. Researchers in the laboratory of Dr. Debra Newman at BloodCenter of Wisconsin have discovered that individuals who have GPVI deficient platelets exhibit only minor bleeding disorders. They are therefore interested in trying to develop a drug that would shed GPVI molecules from the platelet’s surface so as to treat patients with clinical thrombosis complications, with the expectation that such a drug would not cause major bleeding disorders. Heart Attack and Stroke Information Mentor : Dr. Debra Newman 1 GPVI: Structural Model 2 4 Figure 3. Structural model of GPVI. Collagen binds to IgD1 of GPVI. The amino acids in IgD1 that are not involved in collagen binding are colored cyan. The amino acids within IgD1 that comprise the base of the collagen binding site are colored red, whereas those that make up the sides of the collagen binding site are colored dark blue. IgD2 is colored light gray. The disulfide bonds that stabilize IgD1 and IgD2 are colored green. IgD1 IgD2 S-S–Disulfide bond Figure 1. A schematic diagram of the GPVI/FcRγ-chain collagen receptor complex on the surface of a platelet. The extracellular region of GPVI has two Immunoglobulin Domains (IgD1 and IgD2), which are the only portions of GPVI that are included in the model. The transmembrane and intracellular portions of GPVI interact with the FcRγγ-chain, which is responsible for transmitting signals in to the platelet that activate it upon binding of collagen to IgD1 of GPVI. Figure 3A. Side view of the GPVI structure. • There are about 1.2 million heart attacks in the United States every year. • There were about 450,000 deaths from heart attacks in the United States in 2004. • Heart attacks account for about 20% of all deaths in the United States each year. Platelets in Thrombus Formation 3 • There are about 700,000 strokes in the United States every year. • Strokes account for 1 out of every 15 deaths and ranks third among all causes of death in the United States, behind diseases of the heart and cancer. Normal Flow Reduced Flow Figure 3B. Top view of the GPVI structure. No Flow References 1. Heart Disease and Stroke Statistics – 2004 and 2005 (http://www.cdc.gov) (http://www.americanheart.org/downloadable/heart/1105390918119HDSStats2005Update.pdf) 2. Moroi, M. and S.M. Jung. Platelet glycoprotein VI: its structure and function. Thrombosis Research 114:221-33, 2004. 3. Platelet Activation During Thrombosis (http://mail.bris.ac.uk/~pmawp/Thrombus-figure.jpg) 4. Horii, K., M.L. Kahn and A.B. Herr. Structural basis for platelet collagen responses by the immune-type receptor glycoprotein VI. Blood 108:936-42, 2006. 5. Samaha, F.F. and M.L. Kahn. Novel platelet and vascular roles for immunoreceptor signaling. Arteriosclerosis Thrombosis and Vascular Biology 26:2588-93, 2006. Supported by the National Institutes of Health (NIH) – National Center for Research Resources Science Education Partnership Award (NCRR-SEPA) Therapeutic Implications 5 Collagen Figure 2. Effect of thrombus formation on blood flow. When a thrombus forms in an artery, the area for blood flow is lessened. This decreases the amount of blood that flows past the thrombus (reduced blood flow). In addition, rate at which blood flows past the thrombus is increased, which can cause the thrombus to detach from the artery, get carried in the bloodstream to smaller blood vessels, and get stuck (no blood flow). In both cases, the tissue served by the artery is starved for oxygen. When the tissue served is the heart, a heart attack results. When the tissue served is the brain, a stroke occurs. Exposed collagen in injured blood vessels is a primary stimulus for activation of circulating platelets. Inhibition of platelet responses to exposed collagen, therefore, holds significant promise for prevention and treatment of heart attack and stroke. GPVI is the major activating receptor for collagen on the platelet surface. Therapeutic agents that interfere with the interaction of GPVI with collagen are currently under development. The most welldeveloped of these agents is an antibody that blocks GPVI-mediated activation of platelets by collagen. Also promising is an antibody that temporarily cleaves GPVI from the platelet surface. Since GPVI deficiency results in only a mild bleeding disorder, this latter type of agent could reduce the risk of myocardial infarction or stroke without creating an intolerable long-term risk of extensive bleeding.