* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chest Pain - UNC School of Medicine
Remote ischemic conditioning wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Marfan syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Aortic stenosis wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Cardiac surgery wikipedia , lookup
Drug-eluting stent wikipedia , lookup
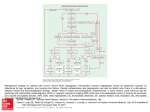
Chest Pain and Shortness of Breath Brett Sheridan, M.D., F.A.C.S Assistant Professor Cardiothoracic Surgery Department of Surgery Causes of Chest Pain and SOB • • • • • • • • Myocardial Infarction Pulmonary Embolism Pneumothorax Hemopneumothorax Thoracic Aortic Dissection Esophageal Rupture Gastro-esophageal Reflux Empyema 47 y/o man is jogging with his daughter when he suddenly collapses unconscious…… Most common causes of death in the US… 1) Heart Disease 2) Cancer 3) Stroke How many people in the US died from cardiovascular disease in 2001? Do more men or women die from cardiovascular disease? Acute coronary syndrome (ACS) is defined by EITHER acute myocardial infarction OR unstable angina. These patients are divided into 3 subsets: ST elevation myocardial infarction non-ST elevation MI Unstable angina (STEMI) Describe the initial stabilizing treatment for symptomatic ischemic heart disease presenting in the ER • • • • • • • • ECG within 10 minutes Supplemental O2 IV access continuous ECG monitoring Sublingual NTG if SBP > 90 mmHG Morphine ASA (chewed) Labs If ST elevation > 1mV or LBBB then reperfusion (fibrinolysis or PTCA) What is AMI management in first 24 hours? • Limited activity 12 hrs and monitor 24 hrs • No prophylactic antiarrythmics • IV heparin if: – large anterior MI, – PTCA, LV thrombus or – thrombolytics administered • • • • • • SQ heparin for all others ASA indefinitely IV NTG x 24 hrs IV beta-blocker if stable ACE inhibitor if BP permits Statin therapy Acute coronary Syndrome: On-going myocardial ischemia despite initial Rx Thrombolytics Revascularization PCI CABG Why are patients referred for CABG instead of undergoing a PCI approach to coronary artery disease? Percutaneous coronary angioplasty (PTCA, PCI,…) Percutaneous coronary angioplasty (PTCA, PCI,…) Percutaneous coronary angioplasty (PTCA, PCI,…) Natural history of percutaneous coronary angioplasty…..uh-oh! Cite 2 prospective randomized trials comparing PCI vs CABG for the treatment of multivessel CAD • Inclusion Criteria – Symptomatic – Multivessel CAD – LVEF > 30% • Baseline Characteristics – – – – Class III/IV angina - 66% Previous MI - 42% 3 vessel CAD - 30% mean LVEF = 60% Comparison of Coronary-Artery Bypass Surgery and Stenting for the Treatment of Multivessel Disease (Arterial Revascularization Therapies Study Group) CABG Patients (n) Late outcome Death MI CVA Revascularization * Event-free survival * Symptom-free * Cost * PCI 605 600 ---------------------1 year----------------2.8% 2.5% 4.0% 5.3% 2.0% 1.5% 4% 17% 88% 74% 90% 79% $13,638 $10,665 Event –free Survival: CABG vs PCIS 14% benefit w/ CABG! Risk of Repeat Revascularization 16 % benefit w/ CABG! Risk of Death 3.7 % SURVIVAL benefit w/ CABG! Conclusions-SoS Trial • Again, repeat revascularization remains more common after PCI (with or without a stent) in multivessel CAD. • In this study, higher rate of all cause mortality with PCI Contrast the difference between “off-pump” CABG versus the typical cardiopulmonary bypass supported CABG. Traditional CABG • General anesthetic • Median sternotomy • Conduit harvest (LITA, radial, vein) • Institution of cardiopulmonary bypass (CPB) • Cardiac arrest • Placement of aorto-coronary grafts • Seperation from CPB • Close Advantages - Traditional CABG • • • • Still Heart Exposure and access Visualization The most intensely scrutinized procedure in US medicine SAFETY Disadvantages - Traditional CABG • Proinflammatory response to CPB • Suggestion of end-organ injury – CNS – Pulmonary – Renal • Increased fluid shifts Off-Pump Stabilizer Off-Pump- Snare Off-Pump Stabilizing Devices Off-Pump Exposure of PDA List 10 complications of CABG and there relative frequency • • • • • • • • • • • Death Stroke Bleeding requiring re-op Wound Problems Myocardial infarction Arrhythmias Pneumonia Pneumothorax Cardiac Tamponade Pericardial Inflammation Renal Insufficiency 3% 1-2% 3-5% 0.5-5% 2-30% 10-60% 4% 1-2% 3-6% 18% 15-20% What four medications prevent MI and death following a myocardial infarction. “Class I” Indications • • • • ASA Beta-blockers ACE inhibitor Statins Risk Of Pneumothorax • • • • • Pain SOB ( dyspnea) Hypoxia Hypotension (embarrassed CO) Death DDX of Underlying Pulmonary Pathology Spontaneous • Primary – Subpleural bleb • Secondary – – – – – – – – Chronic Obstructive lung disease Bullous disease Cystic fibrosis Pneumocystis-related Idiopathic pulmonary fibrosis Pulmonary embolism Catamenial Esophageal perforation • Neonatal Acquired • Trauma • Iatrogenic Treatment options • Observation • Tube thoracostomy • Surgery • Other “dated” options – Needle aspiration – Chemical pleurodesis Observation • • • • • Asymptomatic Pneumothorax less than 20% ER for 4-6 hours w/ repeat CXR F/U within 48 hours and CXR Any doubts --admit Tube Thoracostomy • • • • Primary Method of Management Prompt re-expansion of lung Prevents life-threatening sequelae Allows pleural-pleural apposition –sealing injured lung • Tube removed once air leak resolves for 12 hours Prognosis • Usually resolves within 1-2 days • 30% chance of recurrence • Increases to 60-70% if second pneumothorax Surgery- Indications • • • • • • Recurrent pneumothorax Persistent air leak or incomplete expansion Massive air leak with incomplete expansion History of bilateral pneumothoraces Occupational hazard or lack of access Hemopneumothorax Surgery-Procedure • • • • • Video-assisted thorascopic surgery (VATS) Resection of offending bleb Mechanical pleurodesis Tube thoracostomy Chemical pleurodesis – Tetracycline – Talc Treatment of Secondary Pneumothoraces • Usually associated with significant comorbid disease and debilitated patients • Individualize treatment (less is more) • AIDS and Pneumocystis carinii • COPD • Cystic fibrosis Hemothorax - Etiologies Pulmonary Bullous emphysema Necrotizing Infections • PE with lung infarction • Tuberculosis • AV malformation • Hereditary hemorrhagic telangiectasia Pleural • Neoplasm (mesothelioma) • Endometriosis Pulmonary Neoplasm • Primary • Metastatic – Melanoma – Trophoblastic tumors Blood Dyscrasia • Thrombocytopenia • Hemophilia • Complication of systemic anticoagulation • Von Willebrand’s disease Abdominal Pathology • Pacreatic pseudocyst • Splenic artery aneurysm • Hemoperitoneum Thoracic Pathology • Ruptured thoracic aortic aneurysm Top Causes Trauma . . . Cancer Pulmonary embolism Hemothorax- What to do? • Traumatic – Tube thoracostomy- large bore – IF more than 1500 mL or more than 200 mL/hour x 3 hours THEN surgical exploration • Non-Traumatic – Needle aspiration – Cytology – Tube thoracostomy if HCT > 50% Aortic Dissection…What is it? • A bad problem to have • A sudden (usually) intimal tear of the aorta creating a true lumen and a false lumen • Consequences of this tear are variable depending on location and progression of the dissection Classification-DeBakey Histology and Structure • Normal aorta- 3 layers – intima – tunic media – adventitia Histology and Structure • Media- strongest – – – – – usually 1.2 mm most affected by dissection elastic collagen fibers 20-30 % of aortic wall smooth muscle cells 5 % Microfibrils contain the glycoprotein “fibrillin.” These act as scaffolding for deposition of elastin to produce concentric rings of tunica media. more….Histology and Structure • Aortic dissection denotes one or more tears b/w the the aortic lumen and a medial cleavage plane • May be localized to the point of “primary tear” but often extends. • Rarely circumferential • Re-entry tears occur often… providing communication b/w true and false channels. even more….Histology and Structure • The dissection usually splits the outer layers of the media and weakens the external coat. The false channel may dilate or rupture. • The false channel eventually develops an endothelial lining but may contain extensive thrombus. • Acute stage –14 days • Subacute - 2 months • Chronic - after 2 months Incidence • Annual estimated @ 2-5 cases per million • Pathology series the prevalence ranged from 0.2 to 0.8% in Chicago and Boston • Males > Females 2:1 • Type A - 50-55 years • Type B - 65 years Risk Factors pregnancy Marfan’s hypertension aortic coarctation congenital aortic valve anomalies Presentation- acute dissection • Sudden severe chest pain (90%) worst at onset not previously experienced …adjectives such as “ripping” and “tearing” Presentation- acute dissection • Sudden severe chest pain (90%) worst at onset not previously experienced …adjectives such as “ripping” and “tearing” • History of hypertension • Type A- pain mid-sternal • Type B-pain inter-scapular • If extension… neurologic deficit, abdominal pain, or peripheral extremity ischemia Differential Dx- acute dissection • • • • • • Coronary ischemia/ myocardial infarction Aortic aneurysm w/o dissection Musculoskeletal Pericarditis Biliary colic Pulmonary embolism Physical exam- acute dissection • Blood pressure usually elevated • Hypotension associated w/ pericardial tamponade, rupture, aortic insufficiency, or massive MI • New pulse deficit- 60% • Diastolic decrescendo murmur @ LSB- aortic regurgitation • Diminished left-sided breath sounds- hemothorax • Neurologic exam – mental status, – focality --peripheral vs central Diagnostic studies- acute dissection • CXR – deformity of Aortic knob, – widened mediastinum, – left pleural effusion, etc. • EKG- chest pain w/ normal EKG sine qua non Diagnostic studies- acute dissection Echocardiography currently thought to be the preferred diagnostic test –rapid and accurate. Evaluates aortic valve, segmental wall function, pericardial effusion. Unfortunately operator dependent. Diagnostic studies- acute dissection CT- expeditious w/ reasonable sensitivity and specificity Diagnostic studies- acute dissection MRA-excellent sensitivity and specificity but slow Diagnostic studies- acute dissection Aortography - lacks sensitivity as imaging requires blood flow which may not occur in false lumen. Indication for coronary angiogram remains controversial. DeBakey, Surgery, 1982 Medical Treatment • • • • 24 hrs 2 wks 5 yrs 10 yrs Type A 72% 43% 34% 28% Type B 100% 92% 76% 56% Masuda, Circulation, 1991 Medical Treatment- Aortic Dissection Masuda, Circulation, 1991 Medical vs Surgical - Type B Ao Dissection Glower, Ann Surg, 1991 Conclusion • • • • • • Aortic dissection is a bad problem to have High index of suspicion Control heart rate and blood pressure URGENTLY Type A requires immediate surgery Type B - best served w/ medical treatment If ischemic complications, the patient faces a grim prognosis with (or without) surgery therefore a surgical approach may be advocated. Esophageal Rupture- Causes • Iatrogenic – Esophageal endoscopy /dilation – Paraesophageal surgery • • • • Boerhaave syndrome Trauma Foreign Body Caustic Esophageal RuptureMost common sites of iatrogenic perforation • Proximal to the upper esophageal sphincter • Gastric cardia • Esophageal stricture Untreated perforation • Medianstinitis • Death Nonoperative Management of Esophageal perforation Criteria – – – – • • • • Disruption contained within the mediastinum Free drainage back into the esophagus Minimal symptoms Minimal signs of sepsis Nasogastric decompression Percutaneous drainage IV antibiotics (oral flora) Parenteral nutrition Esophageal RupturePrinciples of surgical treatment • Debridement • Treat the underlying problem – Cancer – Stenosis – Reflux • Repair of perforation • Drainage Gastroesophageal Reflux Disease • 50% of asthma patients have objective evidence of esophageal reflux • Pathophysiology: Reflux vs Reflex • Anti-reflux surgery improves asthma symptoms – 90% of children – 70% of adults GERD – Diagnostic evaluation • History and Physical Exam • Tests – – – – 24 hour ambulatory pH Monitoring Manometry Barium swallow Upper endoscopy GERD- Complications • • • • Stricture Barrett’s esophagus Esophageal ulcer Hemorrhage 4-20% 10-15% 2-7% 2% GERD- Pathophysiology • More frequent and prolonged relaxations of the lower esophageal sphincter • Increased exposure of esophageal mucosa to acid, pepsin and bile salts • Hiatal hernia ??? GERD- Goals of treatment • Heal the injured mucosa • Eliminate symptoms • Prevent or treat complications of GERD GERD – Treatment Options • • • • • • Lifestyle modifications H2 Blockers Proton Pump Inhibitors Surveillance for persistent symptoms Endoscopy Anti-reflux surgery Empyema • Infection of the pleural space • Usually a complication of a bacterial pneumonia or lung abscess Empyema- Common organisms • • • • • • • Staphylococcus aureus (most common) Streptococcus Pseudomonas Klebsiella pneumoniae E. Coli Proteus Bacteroides Empyema - Diagnosis • • • • History and Physical Exam Chest radiograph Chest CT scan Needle aspiration Empyema- Treatment Goals • Resolve sepsis • Complete expansion of lung • Antibiotics • Drain the space (abscess) – Chest tube – Child vs Adult • Decortication – VATS – Thoracotomy