* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CHF
Adherence (medicine) wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Theralizumab wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
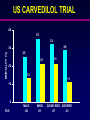
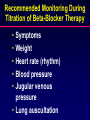
CURRENT APPROACH TO THE TREATMENT OF CONGESTIVE HEART FAILURE Treatment of CHF in 1970 • Digitalis • Diuretics • Salt restriction Modern Rx of CHF • Diuretics • Vasodilators • Beta-blockers • Inotropic agents • Digoxin • Adrenergic agents • Milrinone • Aldactone • BiV Pacing Diuretics • Decrease edema • Do not improve cardiac output • Improve exercise capacity • No known beneficial molecular effects • No reversed remodeling • Do not slow progression of disease • Cause pre-renal failure • Increase mortality Hospitalizations (%) Digitalis: Effect on Hospitalizations 67.1% 64.3% Digoxin Placebo N Engl J Med 1997;336:525-533 Digitalis: Effect on Mortality Mortality % 40 34.8% 0 Digoxin 35.1% Placebo N Engl J Med 1997;336:525-533 “Newer” Therapies • ACE inhibitors (class effect) • Hemodynamic and molecular effects • Beta-blockers (may not be class effect) • Long-term hemodynamic benefits • Probably achieved by molecular effects • Aldactone • Probably just molecular effects • Angiotensin receptor blockers • Similar to ACE inhibitors in most ways CLINICAL ASSESSMENT OF CHF • • • • • • • • BLOOD PRESSURE JVP RALES EDEMA SERUM CREATININE MITRAL REGURGITATION POSTURAL SYMPTOMS BNP WHAT TO EXPECT FROM DIURETICS • RAPID RESPONSE • DECREASED FILLING PRESSURES • EDEMA BUT the tendency is for • CARDIAC OUTPUT • CREATININE • NEUROHUMORAL ACTIVATION VASODILATORS • NITRATES • • VENOUS ARTERIOLAR • ARTERIAL DILATORS • HYDRALAZINE • BALANCED VASODILATORS • • • • NITROPRUSSIDE ACE INHIBITORS ANGIOTENSIN RECEPTOR BLOCKERS OMEPATRILAT (combined ACEI and NEP) WHAT TO EXPECT FROM VASODILATORS • FILLING PRESSURES • CARDIAC OUTPUT • EXERCISE TOLERANCE • NEUROHUMORAL ACTIVATION • REVERSE REMODELING • HOSPITALIZATIONS and MORTALITY HOW TO USE ACE INHIBITORS • PHYSIOLOGICAL APPROACH • DOSES SHOULD BE MAXIMUM TOLERATED • IN CHF, TWICE A DAY (CAPTOPRIL 3-4 TIMES/DAY) • IDEAL BLOOD PRESSURE OFTEN <100 mmHg IF NO POSTURAL SYMPTOMS • IF CHF WORSE AND HYPOTENSIVE, DON’T REDUCE THE DOSE UNLESS CLEARLY NECESSARY • KEEP PATIENT ON IT DESPITE MINOR INCREASES IN CREATININE OR POTASSIUM ATLAS (high vs low dose lisinopril) % Decrease 0% -5% -10% -15% -20% -25% -30% Risk of all cause Risk of death or Frequency of HF mortality hospitalization hospitalizations 8% p=0.12 12% p=0.002 25% p=0.002 WHAT TO EXPECT OF NITRATES • • • • • • VENODILATATION AT LOW DOSES ARTERIAL DILATATION AT HIGH DOSES CARDIAC OUTPUT MITRAL REGURGITATION BENEFICIAL REMODELING IMPROVED EXERCISE TOLERANCE DRUG COMBINATIONS • ACE INHIBITORS AND NITRATES • ACE INHIBITORS AND ANGIOTENSIN RECEPTOR BLOCKERS • BETA-BLOCKERS • ALDACTONE • HYDRALAZINE • INOTROPES Nitrates and Hydralazine • Reduce mortality • ACE/ARB-intolerant patients • Combination with ACE Inhibitors • No adverse effect on renal function • ACE Inhibitors more effective in reducing mortality • Nitrates and Hydralazine - better hemodynamic responses Beta-Adrenergic Blockade in Congestive Heart Failure • • • • • • Historically contraindicated in CHF Counter-intuitive Early studies not definitive Anecdotes impressive Recent trials definitive Still slow to be adopted US CARVEDILOL TRIAL 40 35 32 29 MORTALITY (%) 30 25 21 21 20 13 11 10 0 R.R. MILD .50 MOD .61 DOSE-RES SEVERE .67 .41 LVEF Carvedilol Causes a Dose-Related Improvement in LV Ejection Fraction 8 *p<0.005 vs. placebo 7 **p<0.0001 vs. placebo ** p<0.0001 * 6 * 5 4 3 2 1 0 6.25 mg Placebo 12.5 mg 25 mg bid Carvedilol Circulation 1996;94:2807-2816 Beta-Blockers: Patient Selection • • • • Stable Class I-IV patients LVEF < 35% - 40% Ischemic or non-ischemic On ACE inhibitor, diuretics, with or without digoxin • Heart Rate > 60 bpm, no high degree a-v block • Systolic BP > 85 - 90 mmHg • No contraindications to beta-blockade Initiation of Beta-Blockers in Heart Failure • Optimize control of failure first • Start at the lowest dose • Increase the dose gradually as tolerated (No sooner than every 2 weeks) • Monitor vital signs, weight, and clinical status • Adjust concomitant medications as needed Time course of effects Beta-Blockade Therapy Clinical Benefit Clinical Deterioration 0 1-2 3-4 5-6 11 - 12 Months Am J Cardiol 1997;79:794-798 Recommended Monitoring During Titration of Beta-Blocker Therapy • • • • • Symptoms Weight Heart rate (rhythm) Blood pressure Jugular venous pressure • Lung auscultation Management of Adverse Effects • Control chf before initiation or up-titration • Persist if possible (symptoms usually improve) • May need to consider pacing • If hypotension symptomatic, consider reducing vasodilator or diuretic dose • Deterioration on maintenance Rx, dose reduction or stopping drug usually unnecessary General Approach to Rx • Look for precipitating cause • B.P, JVP and Creatinine – central to assessment and monitoring • A quick fix probably won’t work as well as re-optimizing Rx • Follow up is usually essential Blood pressure • BP ~ 90-100 well-tolerated. Some tolerate 70. • If asymptomatic, don’t decrease vasodilators. • If symptomatic and JVP low, consider reducing diuretic. • If JVP increased and BP is low, can either diurese or add nitrate). • Nitrates have greater potential benefit. • Can add ARB when ACE dose is maximum tolerated. JVP Elevated If BP low, consider adding a nitrate (diuretic often but not always necessary). If blood pressure ok, increase ACE/add nitrate. Fine tune with diuretic when necessary. Creatinine Increasing: • Most often, this means cardiac output is decreasing, not renal artery stenosis. • Need to increase output. Don’t decrease vasodilators unless it clearly is required. • Vasodilators often improve status, diuretics are a throwback to the ’70s and signal defeat. If a patient deteriorates on vasodilators and beta-blockers: •don’t decrease the vasodilators •the beta-blocker should probably also be continued (perhaps after the first few hours which are needed to stabilize the patient). •consider tailored therapy if vasodilators appear to be at maximum-tolerated dose. Case Study • 49 year old man chf due to cardiomyopathy. • BP 135/90, pulse was 90 • Jugular venous pressure 12 cm. asa. • On lasix (40 mg b.i.d.),enalapril (5 mg qd) and digoxin (.25 mg qd). One approach is to diurese aggressively until dry. If you do that, you can expect decreased edema. The patient will feel better and the response is easy to measure (decreased weight, JVP, edema) and the blood pressure will probably change little. Another approach is to view this as an opportunity to improve his therapy by: • Increasing vasodilators • ?Reduce diuretics • ?Combine vasodilators • Add beta-blocker • Add aldosterone antagonist Case Study An 83 year old woman with chf presents with not feeling well. B.P. is 90/60, JVP is 12 cm ASA, Creatinine is 250. Meds include Enalapril 10 mg qd, lasix 60 mg bid, Carvedilol 12.5 mg bid You could just give more diuretic. What will happen? or You could manipulate the vasodilators And possibly reduce the diuretics. Case Study Same patient but the JVP is low and the BP is 80/60 mmHg. What would you do? Short and Long-term Goals Short-term goals • Improve hemodynamic status • decrease filling pressures • increase output • Improve exercise capacity Long-term goals • Reverse remodeling/slow progression • Improve cardiac function • Maintain improved hemodynamic status