* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download DEPRESSION
Survey
Document related concepts
Transcript
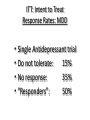
DEPRESSION PREVALENCE OF CLINICAL DEPRESSION (1994) • LIFETIME • YEARLY • Bipolar 17% (?) 10% 5% TREATMENT OF DEPRESSION IN PRIMARY CARE* • Depression: 2nd. Most Common Disorder in Primary Care • 40% Diagnostic Hit Rate • 87% Somatic Sx, 13% Mood Sx (Greist, 2002) A RECURRING ILLNESS • 20% SINGLE EPISODE • 80% RECURRENT or CHRONIC Depression: Fluctuating Course • • • • N= 431 ( ¼ : 1st.episode, ½ recurrent, ¼ : double D.) 12 year Follow-up Symptomatic: 58%, 42%: Sx-free Time Symptomatic: > 15% MDD > 43% Sub-Syndromal …… Depression: Fluctuating Course • • • • N= 431 ( ¼ : 1st.episode, ½ recurrent, ¼ : double D.) 12 year Follow-up Symptomatic: 58%, 42%: Sx-free Time Symptomatic: > 15% MDD > 43% Sub-Syndromal …… WORLD HEALTH ORGANIZATION STUDY • Each day in Primary Care Medical Settings: > 25% of patients have Clinical Depression > 10% have Anxiety Disorders > 10% have Substance Abuse Disorders cont. MOST COMMON DISORDERS SEEN IN PRIMARY CARE • Hypertension • Depression • Anxiety Disorders Most “Reactive Depressions” If they reach the intensity level of Major Depression, will show vegetative symptoms. BIOLOGIC SYMPTOMS • • • • • ANHEDONIA SLEEP DISTRUBANCES APPETITE DISTURBANCES LOSS OF SEXUAL DRIVE FATIGUE Dysthymia “Ill-Humor” • 5% Of the Population (lifetime prevalence) • Most eventually also develop Major Depression Dysthymia • Pharmacologic Outcome: 33% Excellent Response 33% Good Response 34% Poor Response (Akiskal, 1997) Has the Success of Antidepressants Been Over-Sold? 15 Patients Recruited in Antidepressant Drug Studies Zimmerman, et al. (2002) • N= 346 (MDD, outpatient practice) • 86% would be excluded from drug studies ITT: Intent to Treat Response Rates: MDD • Single Antidepressant trial • Do not tolerate: 15% • No response: 35% • “Responders”: 50% ITT Rates • “Responder” = 50% HAM-D, or HAM-D Score of 7 or less • Responders: > Full Responders: HAM-D < 7 50% > Partial Responders: HAM-D: 9-14: 50% ITT: The Rest of the Story • “Full Responders”: > 18% truly asymptomatic > 82% subtle residual symptoms Nierenberg, et al. (1999) Partial Responders: Is Symptomatic Improvement Good Enough? Partial Responders • Time to Next Episode: * 3 times longer to next episode remitters vs. partial responders • Quality of life (espec. Social Functioning) Evidence-Based Medicine and Treatment Algorithms Depression Implications for Treatment Success 1. Hopelessness and Drop-outs (long time to response) 2. Compliance: high risk patients 3. Extreme response to side effects 4. Premature discontinuation (skepticism about meds : 62% ↑ in DC) 5. Patient preferences 6. Inaccurate diagnosis Rating Scales First weeks of Treatment • • • • • Aim to get some immediate relief Medication strategies Exercise Bright light (details later) Combat social withdrawal 26 On-Line Algorithms • International Psychopharmacology Algorithm Project: endorsed by WHO www.IPAP.org • www.MHC.com (also P 450: drug interactions) Choosing a First-line Antidepressant 29 Targeting Neurotransmitters NE: norepinephrine 5-HT: serotonin DA: dopamine 33 NEWER GENERATION ANTIDEPRESSANTS • SSRIs: Serotonin (5-HT) • NRIs: Norepinephrine (NE) • Dual Action: Wellbutrin: NE and Dopamine Effexor: 5-HT and NE (SNRI) Remeron: 5-HT and NE (SNRI) Cymbalta (duloxetine): 5-HT and NE Pristiq 5-HT and NE Neurotransmitters and Behavior • Serotonin: Anxiety, Rumination, Irritability, Aggression, Suicidality Shelton and Tomarken (2001); Metzner, (2000) Neurotransmitters and Behavior • Catecholamines: Dopamine and Norepinephrine: Anhedonia, Apathy, Impaired Attention Shelton and Tomarken (2001); Metzner, (2000) Antidepressants Agorithm Texas Medication Algorithm Project TMAP ANTIDEPRESSANT ALGORITHM With Anxiety or Agitation: SSRIs Anergic: Atypical: PMDD: 38 Activation vs Switching • Activation: within hours; anxiety and/or initial insomnia • Switching: 3+ weeks; manic symptoms 39 Benzodiazepine Augmentation Start up (Ward Smith, et al.) • Check for history of substance abuse • Antidepressant and tranquilizers • Early response…fewer drop outs 40 Benzodiazepine use: HMO Setting (Samari, 2007) • N: 2440 • Treated for 2 years with tranquilizers • Percent of those requesting increased doses: 1.6 % 41 ANTIDEPRESSANT ALGORITHM With Anxiety or Agitation: Anergic: Wellbutrin Atypical PMDD 42 Stimulant augmentation with anergic depressions 43 ANTIDEPRESSANT ALGORITHM With Anxiety or Agitation: Anergic Atypical: watch for bipolar PMDD 44 ANTIDEPRESSANT ALGORITHM Pre-Menstrual Dysphoria: SSRIs 45 ANTIDEPRESSANT ALGORITHM Very Severe and/or Recurrent: Dual Action: Effexor, Pristiq, Cymbalta, Remeron, Wellbutrin 46 Standard vs. Targeted Treatment Improved % of Patients Improved 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 96% 65% Standard Targeted Metzner, 2000 47 • GUIDELINES for MEDICAL TREATMENT of DYSTHYMIA • IRRITABILITY: SSRIs • LOW ENERGY, APATHY, LOW-GRADE ANHEDONIA: Wellbutrin not based on empirical studies Additional Considerations in Medication Choices • Side Effects • Patient Preferences • Pharmacokinetics PHASES OF TREATMENT • ACUTE: Until Asymptomatic • CONTINUATION: 6 months @ Same Dose • MAINTENANCE: Third Episode: Lifetime Treatment → Continuation Phase of Treatment • • • • • Minimum of six months…same dose Patient-initiated discontinuation High rates of acute relapse Serotonin and emotional blunting Dampens dopamine Antidepressant Discontinuation Syndromes • Symptoms: nausea, dizziness, malaise, electric shock-like sensations • Most likely: Paxil, Effexor, Cymbalta, Pristiq • Least likely: Prozac Maintenance Phase ADEQUATE TRIAL • DOSE • COMPLIANCE • TIME • BLOOD LEVELS TIME TO RESPONSE EARLY RESPONDERS: 2-4 WEEKS LATE RESPONDERS: SEVERE SYMPTOMS FIRST EPISODE BEFORE 18 LONG DURATION (more than three months) 4-6 WEEKS Response • Remission • Partial • Poor Overview: Options for Inadequate Response Optimization Augmenting > Combination Treatments Switching Drug Classes Optimization dose; time Augmenting: Combination Switching Classes e.g serotonin norepinephrine reuptake inhibitor Empirical Studies STAR-D: Sequenced Treatment Alternatives to Relieve Depression (NIMH) STAR-D (2007) • N= 4100 • Ages 18-75 • Average patient: 3 medical illnesses • 65%: psychiatric co-morbidity 62 STAR-D • 80%: chronic or recurrent • 25%: have been depressed for 2+ years • 53%: anxious depressions 63 STAR-D Rating Scale page Side effect scale Page Overview: Options for Inadequate Response Optimization Augmenting > Combination Treatments Switching Drug Classes 65 STAR-D (2006) PHASE ONE: Celexa: average doses 40 mg Response rates: 60% Remission rates: 30% Average time to remission: 7 weeks KEY: aggressive dosing 66 STAR-D (2006) PHASE TWO Non-remitters: randomized: > Switch > Augmentation 67 STAR-D: Switch (2006) Effexor: Wellbutrin: Zoloft: 25% 21% 17% Average time to remission: six weeks 68 STAR-D: Augment (2006) Wellbutrin: BuSpar: 30% 30% Augmenting: slightly higher yield than switching 69 New Study 70 STAR-D: After Phase 2 •55% reach remission 71 STAR-D (2006) PHASE Three: > Switch: nortriptyline (tricyclic) or Remeron > Augment: lithium T3 72 STAR-D (2006) PHASE Three: > Switch: nortriptyline or Remeron 13% > Augment: lithium 20% T3 20% 73 T3 Augmentation • • • • 4 double bind studies: indicate efficacy STAR-D study: very high yield Few Side Effects Dose: Cytomel 25-75 micrograms qd 74 STAR*D Final Outcomes 67% Complete remission 75 STAR-D Cumulative Sustained Recovery Rate 43% 76 STAR-D Monotherapy STAR-D Monotherapy STAR-D Augmentation Guidelines What Can Be Learned from STAR-D • • • • Use of rating scales Aggressive dosing Some suggestions: next steps Testament to the difficulties in treating very severe depression Head-to-Head Comparisons: SSRIs • N= 26,000……….117 trials • Efficacy and tolerability • Among SSRIs: Sertraline (Zoloft) comes out on top • Lexapro #2 (not generic….no drug-drug interactions) • Cochran Database Surveys (2009) 81 Head-to-Head Comparisons • SSRIs: versus Effexor and Remeron better efficacy (dual action drugs) • SSRIs versus Wellbutrin: Wellbutrin: better tolerability • Best for headaches: Elavil Cochran Database Surveys (2009) 82 PARTIAL RESPONSE STRATEGIES • FIRST: Check Compliance & Substance Abuse • INCREASE DOSE • AUGMENT Other augmentation Strategies Augmentation Strategies • Lithium: 0.3-0.6 mEq/l > relapse x 3 > 7 fold suicides THYROID • Adding T3 or T4: augmentation • T4 for rapid cycling • Hypothyroid in Lithium therapy Thyroid Augmentation • T4: levo-thyroxine: > Synthroid, Levothyroid, Levoxyl > 1 mcg per pound of weight qd • T3: triiodothyronine: > Cytomel > 25-75 mcg. qd Hypothalamus TRH Pituitary TSH Thyroid T3 Gland T4 TSH Thyroid Stimulating Hormone Depression and Hypo-Thyroid The most common medical cause of depression (10%) Grade I: T3 and T4: TSH Grade II: Normal T3/T4, but TSH (Wolkowitz, 2003; Zweifel, 1997) “Normal” TSH Levels High Normal Range 3.0 | | Median 1.3 | | Low Normal Range 0.3 miliIU/Liter “Normal” TSH Levels High Normal Range | | Median | | Low Normal Range 3.0 2.5 1.3 0.3 miliIU/Liter Stimulant Augmentation MAOIs New MAOI: Emsam selegiline transdermal: 6-12 mg per day Augmentation Strategies • Atypical Antipsychotics: * Zyprexa *Abilify *Geodon *Risperdal * Seroquel ? Reducing Treatment-Resistant Unipolar Depression MADRS Total: Acute Treatment Fluoxetine Mean Change from Baseline (LOCF) Improvement 0 (n=10) -5 Olanzapine (n=8) *p<0.05 vs Flx. +p<0.05 vs Olz. -10 -15 *+ -20 0 *+ *+ * *+ *+ *+ *+ 1 2 3 4 5 6 7 Weeks of Double-Blind Therapy Mean modal dose during double-blind therapy: Flx = 52 mg/d, Olz = 12.5 mg/d, Olz + Flx = 13.5 mg/d + 52 mg/d. Shelton RC et al. Am J Psychiatry 2001; 158:131-134. 8 Olanzapine/ Fluoxetine (n=10) Folic Acid • Low serum levels in treatmentresistant depression and early relapse • Co-factor: Serotonin • 500 mcg 2 X per day • With Depakote: 1-2 mg per day High Intensity Light Therapy • Seasonal and non-seasonal • Caution with: Bipolar POOR RESPONSE STRATEGIES • CHECK COMPLIANCE and SUBSTANCE ABUSE • INCREASE DOSE • SWITCH CLASSES: e.g. SSRI NE NE SSRI Within Class Switches • Reasons for switch: > Tolerability > Efficacy (espec. with partial Response) • Two SSRI failures: switch classes LATE EMERGING SEROTONIN SIDE EFFECTS • SEXUAL DYSFUNCTION > Inorgasmia • APATHY and EMOTIONAL BLUNTING • WEIGHT GAIN (10% after one year) Prevalence Sexual Problems / Complaints • Reporting: 14% • Elicited on questionnaire 60% • N: 6300: only 29% had no other risk factors except antidepressant exposure…… Prevalence Sexual S.E. without other probable causes • • • • • Celexa, Lexapro, Effexor Zoloft, Paxil Prozac, Remeron Serzone Wellbutrin 30% 28% 24% 14% 7% Clayton, et al. 2002 LATE EMERGING SEROTONIN SIDE EFFECTS • SEXUAL DYSFUNCTION > Inorgasmia • APATHY and EMOTIONAL BLUNTING • WEIGHT GAIN (10% after one year) GENDER DISTRIBUTION DEPRESSION Disorder Female : Male • CHILDREN • TEENS • ADULTS 1:1 2:1 2:1 • BI-POLAR I • BI-POLAR II 1:1 2:1 Premenstrual Dysphoric Disorder: PMDD Average female: 400 periods 70 %: PMS at some point in time 30 %: significant PSM 4 %: PMDD Premenstrual Dysphoric Disorder: PMDD Premenstrual exacerbation of Major Depression symptoms 90% of women who successfully commit suicide: premenstrual Premenstrual Dysphoric Disorder: PMDD Treatments: > reduce caffeine, alcohol, salt, sugar, and stop smoking > exercise > Serotonin antidepressants > St. John’s Wort (case reports) Premenstrual Dysphoric Disorder: PMDD Antidepressant treatments Must target Serotonin Intermittent versus continuous Quick onset of actions PMDD and SEROTONIN Fluctuating estrogen levels can have an impact on Tryptophan hydroxylase (rate-limiting enzyme for production of 5-HT) Allopregnenolone • Neuro-steroid: synthesized in the brain • Potent GABA-A agonist • Low levels in MDD CSF (↑ with successful treatment) Allopregnenolone • PMDD: marked reduction • Rapid increase with SSRIs but not with nonserotonin antidepressants Premenstrual Dysphoric Disorder: PMDD Calcium supplementation 2 double blind, placebo controlled studies 1200 mg per day (4 Tums) 55% vs 36% Myths about Pregnancy and “Well Being” • Risks of major depression: prenatal and postpartum: 21% (highest risk for women) • Risks of discontinuing medications: Bipolar: 83% acute relapse Major depression: 68% relapse 116 Depression and Pregnancy Depression and pregnancy: > Hypercortisolemia > Substance abuse > Suicide attempts > Post-partum exacerbation (bonding and attachment) Depression and Pregnancy Depression and pregnancy: > Hypercortisolemia > Substance abuse > Suicide > Poor self care > Post-partum exacerbation (bonding and attachment) FDA RATINGS: USE DURING PREGNANCY A: B: C: D: X: No Risk. Well controlled studies No Evidence of Risk Risk Cannot Be Ruled Out Positive Evidence of Risk Contraindicated in Pregnancy 120 Newer Antidepressants and Pregnancy • FDA classifications: all “C” except: • Paxil: D > Discontinuation syndrome > 2nd and 3rd trimester exposure: risk of cardiac defects (2% vs 1%) 121 Antidepressants: Meta-analysis (Einarson and Erinarson, 2005) • • • • N: 1774 exposed fetuses First trimester exposure Major malformations: 2-3% This equals the base rate in un-exposed fetuses 122 Antidepressants: Risks (Hauser, et al., JAMA 2009) • Small but statistically non-significant increase in miscarriages • Not compared to non-depressed subjects • Premature birth: 20% greater: in both medicated and non-med mothers 123 Antidepressants: Risks • No specific birth defects • ??? Cardiac defects in SSRIs ??? 124 The Jury is Still Out 126 PSYCHOTIC DEPRESSIONS • • • • Antidepressants (AD) Antipsychotics (AP) AD + AP ECT 35% 45% 75% 90% Note: Continuation Phase: One Year AD and AP Electroconvulsive therapy ECT: Electro-convulsive Therapy Shock Treatments V DEPRESSION IN CHILDREN and ADOLESCENTS MAJOR DEPRESSION • Children 3% • Teens: 10% 35% recurrent 50% bipolar Depression in Young Children • • • • Luby, et al. (2002) N=49 Using DSM-IV criteria: 12 Dx as MDD Thus must use modified criteria… MDD Children: Modified Diagnostic Criteria • Most of the day, more days than not • Play: themes of death, suicide, selfdestruction (61%) • Depressed or irritable mood or Diminished interest plus 4 Sx (vs 5 for adults) SYMPTOMS IN CHILDREN • • • • • • ANHEDONIA / WITHDRAWAL (60%) IRRITABILITY (81%) LOW SELF-ESTEEM (78%) SCHOOL FAILURE LONLINESS VEGETATIVE Sx: Sleep and Appetite Disturbance (80%) • LOW ENERGY (58%) ….. Child and Adolescent Depression:Additional Signs • • • • • • • Vague, non-specific physical complaints Running away from home Being bored Extreme sensitivity to rejection or failure Reckless behavior; Acting Out Difficulty with relationships Substance Use / Abuse Problems with the studies Meta analysis: Effect Size: 0.25 TAD S Treatment for Adolescents with Depression Study Effectiveness Outcomes (2004) Random Assignment • • • • • • NIMH Study N: 432 Placebo Prozac Cognitive Behavioral Therapy Combo: drug and CBT Responders Percent Treatment Response: Week 12 100 90 80 70 60 50 40 30 20 10 0 71 61 43 COMB FLX CBT 35 PBO TAD S Effect Size 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 COMB FLX CBT TAD S Time to Onset of Effects • Anxiety: 1-2 weeks • Depression: 4-6 weeks but responders in 10-12 week range ! Paxil and Increased Suicidality • UK study…N=1300 adolescents • Increased suicidality: Placebo: 1.2% Paxil: 3.4% • No actual Suicides • 33 suicidal incidents ….. Paxil and Increased Suicidality • Acute Treatment data • Discontinuation • State of Connecticut: Human Implications TADS (2004) • At baseline: 29% suicidal ideas • Attempts: 1.6% • Actual Suicides: 0 Suicidality Is Reduced Overall 29.2 30 27 Percent 25 20 14.6 13 15 11.6 10 5 CDRS13 > 1 SIQ >= 31 2.7 0 Baseline Week 6 Week 12 TAD S FDA Data N= 4400 N= 300 http://www.fda.gov/ohrms/dockets/ac/04/slides/2004-4065s1.htm All trials, all indications (Fixed effect model) Risk ratio (95% CI) % Weight Study CELE(MDD,18) CELE(MDD,94404) EFFEX(MDD,382) EFFEX(MDD,394) PAXIL(MDD,329) PAXIL(MDD,377) PAXIL(MDD,701) PAXIL(SAD, 676) PROZ(MDD,HCCJ) PROZ(MDD,HCJE) PROZ(MDD,X065) PROZ(OCD,HCJW) REMER(MDD,045) SERZ(MDD,141) SERZ(MDD,187) ZOLO(MDD,501001) ZOLO(MDD,501017) 0.42 (0.15,1.15) 0.41 (0.16,1.04) 1.82 (0.75,4.39) 0.84 (0.37,1.88) 2.00 (0.96,4.18) 0.70 (0.25,1.97) 3.92 (0.45,34.50) 4.73 (0.23,97.73) 0.90 (0.26,3.12) 0.78 (0.44,1.39) 0.71 (0.35,1.45) 0.90 (0.08,9.58) 0.81 (0.40,1.65) 0.80 (0.33,1.94) 1.28 (0.58,2.79) 1.04 (0.44,2.45) 0.93 (0.43,1.99) Overall (95% CI) 0.93 (0.75,1.15) .01 .1 1 7.2 8.9 4.2 7.1 5.8 4.9 0.6 0.3 2.6 13.7 8.7 0.9 9.0 6.2 6.6 5.8 7.4 10 100 Risk ratio Emergence of Suicidality 147 Discontinuation All trials, all indications (Fixed effect model) Risk ratio (95% CI) % Weight Study CELE(MDD,18) CELE(MDD,94404) EFFEX(MDD,382) EFFEX(MDD,394) PAXIL(MDD,329) PAXIL(MDD,377) PAXIL(MDD,701) PAXIL(SAD, 676) PROZ(MDD,HCCJ) PROZ(MDD,HCJE) PROZ(MDD,X065) PROZ(OCD,HCJW) REMER(MDD,045) SERZ(MDD,141) SERZ(MDD,187) ZOLO(MDD,501001) ZOLO(MDD,501017) 0.82 (0.19,3.57) 0.60 (0.26,1.38) 2.50 (0.52,11.93) 0.81 (0.21,3.19) 1.55 (0.49,4.94) 0.80 (0.21,3.10) 1.69 (0.36,7.98) 8.79 (0.47,165.62) 0.67 (0.15,2.98) 1.34 (0.66,2.71) 0.88 (0.31,2.48) 1.09 (0.11,10.83) 1.31 (0.39,4.46) 0.51 (0.11,2.30) 1.29 (0.12,13.43) 1.75 (0.21,14.28) 1.50 (0.29,7.65) Overall (95% CI) 1.11 (0.81,1.50) .01 .1 1 10 100 Risk ratio Worsening/Emergence of Suicidality/discont 5.1 18.3 3.1 5.8 6.1 6.2 3.7 0.7 3.7 16.5 8.5 2.0 5.9 7.3 1.9 2.1 3.1 149 Impact of Antidepressants on Suicide Rates • 1957-1985: USA: suicide rates 31% • 1986-1999: USA: suicide rates 13.5% • 1986-1999: 4-fold Rx for antidepressants • Most people who die from suicide were not receiving treatments for depression Grunebaum, et al. (2004) CDC Data: Ages 5-14 (Am. J. Psychiatry, 2006) 1996-1998…Suicides: 933 Low rates of SSRI Rx: 1.7 / 100,000 / year High rates of SSRI Rx: 0.7 / 100,000 / year Impact on Prescribing CDC: Lubell, et al. 2007 • 1990-2003: suicides 29% (ages: 10-24) • 30-40% decrease in prescriptions for antidepressants for kids and teens • 2003-2004: teenage suicides increased by 18% When antidepressants can provoke suicide V:OTC Products Endorsed By: • USP (US Pharmacopia) ST. JOHN’S WORT 157 Cochrane Data Base: Systematic Studies • Meta analysis • St. John’s Wort; equal efficacy to prescription antidepressants • Linde, et al. (2008) 158 ST. JOHN’S WORT TREATMENT Reasons for use 900-1800 mg per day Three, divided doses Cost: $1.00 per day 159 ST. JOHN’S WORT Side effects: mild GI, sedation. No: weight gain or sexual dysfunction Watch for Drug-Drug Interactions! Washout time before starting another antidepressant: 5 Days 160 S-Adenosylmethionine SAM-e Comprehensive review of literature (Papakostas, et al. , 2003) 76 studies world-wide Comparable efficacy to ADs Much better tolerated 162 SAM-e Treatment: Major Depression 400-1600 mg per day $3-5 per day IV Dosing Methyl donor: serotonin and norepinephrine 163 SAM-e So Far lack of significant drugdrug interactions Problems: homocysteine Take: B vit. including Folate Can provoke mania Treats osteoarthritis 164 Low Folic Acid: Associated with • Depression: > meta analysis: 10 epidemiologic studies: > significant relationship between low folate and depression (Gilbody, et al. 2007) 165 Low Folic Acid: Associated with • Decreased CSF metabolites: Serotonin (5-HIAA) Dopamine (HVA) Norepinephrine (MHPG) • Depression may lead to low folate 166 Folic Acid Low serum levels in treatmentresistant depression and early relapse Low folate: increased risk for dementia 167 Folic Acid Dosing: 500 mcg per day Significant augmenter vs placebo Prozac…took ten weeks (Coppen, 2000) Deplin (L-methylfolate) > no advantage over folic acid With Depakote: 1-2 mg per day 168 Omega-3 Fatty Acids: essential fatty acids Families of Fatty Acids Omega-3 > LNA: seed and nut oils > EPA: fish oil > DHA: fish oil Omega-6 > LNA: seed and nut oils > Soy bean oil and corn oil > Arachidonic acid: Animal Tissue 170 Omega 3:6 ratios • Typical USA diet: 1:20 • Ideal: 1:3 Omega 3 Fatty Acids: Bipolar Disorder Mixed findings (Stoll, et al. 1999; Peet and Horrobin, 2002; Nemets, et al., 2002) 172 Omega-3 and Depression • Fish oil: Much better bio-availability • 1-2 grams a day (EPA + DHA) • 6 published studies: major depression > all: add-on studies > all significant better than placebo • ↑ omega 3, ↑ serotonin and dopamine transmission 173 Omega-3, Pregnancy and Major Depression (Su, Chin, et al. 2008) • • • • • • N: 36 8 weeks, double blind, placebo EPA: 2.2 grams, DHA: 1.2 grams Response: Omega-3: 62%...placebo: 27% Remission: Omega-3: 38%...placebo: 18% No side effects Omega-3 Fatty Acids Side effects: GI (diarrhea, nausea) Take with food…ginger root or ginger ale The mercury issue 175 176 5-HTP Tryptophan 5-HTP 5-HT (serotonin) 5-HTP 2 well controlled double-blind studies (total 108) 300 mg per day (600 TRD) Main Side effect: Sedation (pm) Compounding pharmacy Watch for serotonin syndrome Other OTC Options • Melatonin • Kava Kava • Valerian CAUTION! High-Intensity Light Therapy High Intensity Light Therapy SAD and winter blues: 1:4 Psychoanalytic views of seasonal mood changes (1945) High Intensity Light Therapy Dosing: 2500 lux Average time: 20 minutes Morning light is 2 x more effective Effects seen: 2-3 days Lost with placebo or discontinuation High Intensity Light Therapy Use in non-seasonal depression Side effects: nausea, jitteriness, eye strain, dizziness Blue lights: forget it High Intensity Light Therapy Contraindications: macular degeneration, retina diseases, post cataract surgery UV effect on the skin Bipolar disorder Dawn Simulation Sunlight Exposure (melanocytes…endorphins) Exercise Dosing • • • • 10,000 steps per day Aerobic …in keeping with fitness Two 10 minute sessions a day 20 minutes: 3 times a week St. Mom’s Wort Given to pre-schoolers: renders them unconscious for 6 hours Practice Case: 1 • 54 year old man. Profession: undertaker. No history of depression. • 6 months ago funeral home was sold and he was not hired by the new owner. He had worked for the former funeral home for 25 years • 3 months of unsuccessful job searching. Felt frustrated. Possibly low grade depression Practice case: 1 • 3 months ago at family gathering, a relative made a comment about his “chronic unemployment” • From that point there has been a downward spiral…increasing low self-esteem.. increasing depression Clinical Symptoms • • • • • • • Marked apathy and anhedonia Early morning awakening 11 pound weight gain Suicidal ideas Fatigue Social withdrawal (impact on job search) No sex drive (impact on marriage) Other factors to consider • • • • • • Caffeine use: 4 – 12 oz. cups of coffee per day Occasional alcohol use Chronic headaches (takes OTC meds) No significant medical illnesses No use of prescription drugs No drug abuse Initial Questions • What is the diagnosis? • Given the clinical picture, what class of antidepressants should be considered as a first-line choice?....and why? • He is started with an antidepressant (one that does not require initial titration)…the dose is considered to be in the therapeutic range Three weeks • He reports: no noticeable changes since starting medication treatment • What do you do first? And why? (highest yield next step strategies) You implement revised treatment plan • Week 6 (since first dose): no improvement • What do you do?...and why New Strategy Works • 4 weeks into new treatment: 20% improvement on current medications… • What do you do? • New scenario: 4 weeks: 50% improvement • 4 additional weeks: still at 50% improvement • What do you do? New Scenario • Week 3 into the initial treatment and you discover that the patient has cold intolerance. • What might this suggest and how might it affect your treatment? New Scenario: Different Presenting Clinical Symptoms • • • • • • • Significant anxiety; lots of rumination Early morning awakening 11 pound weight loss Suicidal ideas Anger outbursts and marked irritability Social withdrawal (impact on job search) No sex drive (impact on marriage) Questions • Given the clinical picture, what class of antidepressants should be considered as a first-line choice?....and why? • He reports that after the first day of treatment there is an increase in anxiety and agitation…what is going on and what might you do to address this situation? Side Effect Problems: how might you address each? • Significant nausea • Onset of initial insomnia • After he begins to respond positively, there is some return of libido…he is relieved… • 4 weeks later he reports an inability to reach an orgasm..what is likely to be happening? • What can you do? Side Effect Problems: how might you address each? • Different scenario: after 4 weeks, he starts to experience impotency…what is happening/ • What might you do? New Scenario • Treatment is successful… he has reached remission. • What do you do now? New Scenario • Treatment is successful… he has reached remission. • 2 months into continuation he reports break-thru depressive Sx….what might be happening?....what can you do?