* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 09-ACUTE INFLAMMATION.morphology, pptx
Adaptive immune system wikipedia , lookup
Atherosclerosis wikipedia , lookup
Neonatal infection wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immune system wikipedia , lookup
Complement system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Acute pancreatitis wikipedia , lookup
Rheumatic fever wikipedia , lookup
Periodontal disease wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Innate immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
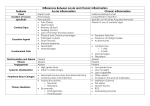
Morphologic Patterns Defect in leukocyte function Complement deficiency Systemic manifestation Acute Inflammation CELLULAR EVENTS: LEUKOCYTE EXTRAVASATION AND PHAGOCYTOSIS Vasodilation Role of Mediators in Different Reactions of Inflammation Increased vascular permeability Chemotaxis, leukocyte recruitment and activation Fever Pain Tissue damage Prostaglandins Histamine Nitric oxide Vasoactive amines Bradykinin Leukotrienes C4, D4, E4 PAF Substance P C5a Leukotriene B4 Chemokines IL-1, TNF Bacterial products IL-1, TNF Prostaglandins Prostaglandins Bradykinin Neutrophil and macrophage lysosomal enzymes Oxygen metabolites Nitric oxide Patterns of Acute Inflammation Outcomes of Acute Inflammation Patterns of chronic Inflammation Defect in leukocyte function Complement deficiency Systemic manifestation Patterns of Acute Inflammation Outcomes of Acute Inflammation Patterns of chronic Inflammation Defect in leukocyte function Complement deficiency Systemic manifestation Several types of inflammation vary in their morphology and clinical correlates. Why? The severity of the reaction specific cause the particular tissue site involved SEROUS INFLAMMATION FIBRINOUS INFLAMMATION SUPPURATIVE OR PURULENT INFLAMMATION ULCERS SEROUS INFLAMMATION: Serous inflammation is marked by the outpouring of a thin fluid e.g. the skin blister resulting from a burn or viral infection represents a large accumulation of serous fluid FIBRINOUS INFLAMMATION more severe injuries and more greater vascular permeability, larger molecules such as fibrinogen pass the vascular barrier, and fibrin is formed and deposited A fibrinous exudate is characteristic of inflammation in the lining of body cavities, such as the meninges, pericardium and pleura FIBRINOUS INFLAMMATION Fibrinous exudates may be removed by fibrinolysis But when the fibrin is not removed, it may stimulate the ingrowth of fibroblasts and blood vessels and thus lead to scarring (organization) characterized by the production of large amounts of pus or purulent exudate consisting of neutrophils, necrotic cells, and edema fluid Certain bacteria (e.g., staphylococci) produce this localized suppuration and are therefore referred to as pyogenic (pusproducing) bacteria Suppurative inflammation. A, A subcutaneous bacterial abscess with collections of pus. B, The abscess contains neutrophils, edema fluid, and cellular debris. Abscesses : localized collections of purulent inflammatory tissue caused by suppuration buried in a tissue, an organ, or a confined space Localized liquefactive necrosis liver abscess Removal of the dead tissue leaves behind a scar ULCERS An ulcer is a local defect of the surface of an organ or tissue that is produced by the sloughing (shedding) of inflammatory necrotic tissue ULCERS encountered in: 1) inflammatory necrosis of the mucosa of the mouth, stomach, intestines, or genitourinary tract 2) subcutaneous inflammation of the lower extremities in older persons who have circulatory disturbances Ulceration can occur only when tissue necrosis and resultant inflammation exist on or near a surface Epithelial Defect Necrotic base Fibrinopurulent exudates Granulation tissue Fibrosis Patterns of Acute Inflammation Outcomes of Acute Inflammation Patterns of chronic Inflammation Defect in leukocyte function Complement deficiency Systemic manifestation Acute inflammation may have one of the four outcomes: Complete resolution Healing by connective tissue replacement (fibrosis) Progression of the tissue response to chronic inflammation Abcess formation Complete resolution When? 1) the injury is limited or short-lived 2) there has been little tissue destruction 3) the damaged parenchymal cells can regenerate Complete resolution Mechanism: Neutralization and removal of chemical mediators Normalization of vascular permeability halting of leukocyte emigration Clearance of edema (lymphatic drainage) , inflammatory cells and necrotic debris (macrophages). Events in the resolution of inflammation Healing by connective tissue replacement (fibrosis): This occurs after substantial tissue destruction the inflammatory injury involves tissues that are incapable of regeneration there is abundant fibrin exudation. The destroyed tissue is resaorbed and eventually replaced by fibrosis. Progression of the tissue response to chronic inflammation: occurs when the acute inflammatory response cannot be resolved WHY? Due to: 1. the persistence of the injurious agent 2. some interference with the normal process of healing A 36-year-old man has had midepigastric abdominal pain for the past 3 months. An upper gastrointestinal endoscopy shows a 2cm, sharply demarcated, shallow ulceration of the gastric antrum. A biopsy specimen of the ulcer base shows angiogenesis, fibrosis, and mononuclear cell infiltrates with lymphocytes, macrophages, and plasma cells. Which of the following terms best describes this pathologic process? (A) Acute inflammation (B) Serous inflammation (C) Granulomatous inflammation (D) Fibrinous inflammation (E) Chronic inflammation Patterns of Acute Inflammation Outcomes of Acute Inflammation Patterns of chronic Inflammation Defect in leukocyte function Complement deficiency Systemic manifestation inflammation of prolonged duration weeks or months Mixture of active inflammation, tissue destruction, and attempts at repair it may follow: 1. acute inflammation or 2. begins insidiously, as a low-grade, often asymptomatic response. This is the cause of tissue damage in some of the most common and disabling human diseases, such as rheumatoid arthritis, atherosclerosis, tuberculosis, and chronic lung diseases 1. 2. Viral infection Persistent infections by certain microorganisms, e.g. tubercle bacilli, Treponema pallidum, fungi, and parasites. 3. Prolonged exposure to potentially toxic agents, either exogenous or endogenous e.g. of exogenous agent is particulate silica, when inhaled for prolonged periods, results in silicosis e.g. of endogenous agent is atherosclerosis (a chronic inflammatory process of the arterial wall induced by endogenous toxic plasma lipid components) 4. Autoimmunity: immune reactions develop against the individual's own tissues In these diseases, autoantigens evoke immune reaction that results in chronic tissue damage and inflammation e.g. rheumatoid arthritis and lupus erythematosus 1. Infiltration with mononuclear cells include 2. Tissue destruction 3. Macrophages Lymphocytes Plasma cells Eosinophils induced by the persistent offending agent or by the inflammatory cells. Healing by connective tissue replacement of damaged tissue, accomplished by proliferation of small blood vessels (angiogenesis) and, in particular, fibrosis MONONUCLEAR CELL INFILTRATION Macrophages the dominant cellular player in chronic inflammation The mononuclear phagocyte system (sometimes called reticuloendothelial system) consists of closely related cells of bone marrow origin, including blood monocytes and tissue macrophages mononuclear phagocyte system –monocytes begin to emigrate into extravascular tissues quite early in acute inflammation and within 48 hours they may constitute the predominant cell type Macrophages may be activated by a variety of stimuli, including Activation results in cytokines (e.g., IFN-γ) secreted by sensitized T lymphocytes and by NK cells bacterial endotoxins other chemical mediators increased cell size increased levels of lysosomal enzymes more active metabolism greater ability to phagocytose and kill ingested microbes. Activated macrophages secrete a wide variety of biologically active products that, if unchecked, result in the tissue injury and fibrosis . Products of macrophages 1.Acid and neutral proteases 2.Chemotactic factors 3.Reactive oxygen metabolites 4.Complement components 5. Coagulation factors 6.Growth promoting factors for fibroblasts, blood vessels and myeloid progenitor cells 7.Cytokines : IL-1, TNF 8.Other biologic active agents ( PAF, interferon, AA metabolites) to eliminate injurious agents such as microbes Function?!!.. to initiate the process of repair It is responsible for much of the tissue injury in chronic inflammation The roles of activated macrophages in chronic inflammation. Acute & Chronic inflam. persist In chronic inflammation, macrophage accumulation persists, this is mediated by different mechanisms: 1. Recruitment of monocytes from the circulation, which results from the expression of adhesion molecules and chemotactic factors 2. Local proliferation of macrophages after their emigration from the bloodstream 3. Immobilization of macrophages within the site of inflammation Lymphocytes Both T & B Lymphocytes migrates into inflammation site –Lymphocytes and macrophages interact in a bidirectional way, and these reactions play an important role in chronic inflammation Activated lymphocytes and macrophages influence each other and also release inflammatory mediators that affect other cells. •Eosinophils are abundant in immune reactions mediated by IgE and in parasitic infections • respond to chemotactic agents derived largely from mast cells • Granules contain major basic protein: toxic to parasites and lead to lysis of mammalian epithelial cells Mast cells are widely distributed in connective tissues express on their surface the receptor that binds the Fc portion of IgE antibody , the cells degranulate and release mediators, such as histamine and products of AA oxidation GRANULOMATOUS INFLAMMATION Granulomatous inflammation is a distinctive pattern of chronic inflammatory reaction characterized by focal accumulations of activated macrophages, which often develop an epithelial-like (epithelioid) appearance Infections Bacterial Parasitic Fungal Inorganic dusts Foreign bodeis unknown Examples of Diseases with Granulomatous Inflammations Disease Cause Tissue Reaction Tuberculosis Mycobacterium tuberculosis Noncaseating tubercle Caseating tubercles Leprosy Mycobacterium leprae Acid-fast bacilli in macrophages; noncaseating granulomas Syphilis Treponema pallidum Gumma: wall of histiocytes; plasma cell Cat-scratch disease Gram-negative bacillus Rounded or stellate granuloma Sarcoidosis Unknown etiology Noncaseating granulomas Crohn disease Immune reaction against intestinal bacterial dense chronic inflammatory infiltrate with noncaseating granulomas Role of lymphatic and Lymph Nodes in Inflammation u Represents a second line of defense u Delivers antigens and lymphocytes to the central lymph nodes u Lymph flow is increased in inflammation u May become involved by secondary inflammation (lymphangitis, reactive lymphadenitis) Patterns of Acute Inflammation Outcomes of Acute Inflammation Patterns of chronic Inflammation Defect in leukocyte function Complement deficiency Systemic manifestation 1. 2. Genetic Acquired lead to increased vulnerability to infections A. Defect in leukocyte adhesions: - Leukocyte adhesion deficiency 1 β chain of CD11/CD18 integrins - Leukocyte adhesion deficiency 2 Fucosyl transferase required for synthesis of sialylated oligosaccharide (receptor for selectin) B. Defect of phagocytosis (Chédiak-Higashi syndrome) An autosomal recessive condition characterized by neutropenia (decreased numbers of neutrophils), defective degranulation, and delayed microbial killing C. Defect of bactericidal activity (Chronic granulomatous disease) Patients susceptible to recurrent bacterial infection. Chronic granulomatous disease results from inherited defects in the genes encoding several components of NADPH oxidase, which generates superoxide. Thermal injury, diabetes, malignancy, sepsis, immunodeficiencies Hemodialysis, diabetes mellitus Chemotaxis Adhesion Leukemia, anemia, sepsis, diabetes, neonates, malnutrition Phagocytosis and microbicidal activity Patterns of Acute Inflammation Outcomes of Acute Inflammation Patterns of chronic Inflammation Defect in leukocyte function Complement deficiency Systemic manifestation Complement deficiency hereditary deficiency of C3 results in an increased susceptibility to infection with pyogenic bacteria. Deficiencies of the late components of the classical complement pathway (C5-C8) result in recurrent infections by Neisseria Inherited deficiencies of C1q, C2, and C4 increase the risk of immune complexmediated disease (e.g., SLE) hereditary deficiency of complement components, especially C3 (critical for both the classical and alternative pathways), results in an increased susceptibility to infection with pyogenic bacteria. Inherited deficiencies of C1q, C2, and C4 do not make individuals susceptible to infections, but they do increase the risk of immune complex-mediated disease (e.g., SLE), possibly by impairing the clearance of apoptotic cells or of antigen-antibody complexes from the circulation. Deficiencies of the late components of the classical complement pathway (C5-C8) result in recurrent infections by Neisseria (gonococci, meningococci) but not by other microbes. Lack of the regulatory protein C1 inhibitor allows C1 activation, with the generation of down-stream vasoactive complement mediators The result is hereditary angioedema, characterized by recurrent episodes of localized edema affecting the skin and/or mucous membranes. Patterns of Acute Inflammation Outcomes of Acute Inflammation Patterns of chronic Inflammation Defect in leukocyte function Complement deficiency Systemic manifestation Acute phase reaction/response - IL-1 and TNF - Fever - Malaise - Anorexia Bone marrow - leukocytosis - IL-1 + TNF Lymphoid organs Liver -IL-6, IL-1, TNF -Acute phase proteins C-reactive protein Lipopolysaccharide binding protein Serum amyloid A a-2 macroglobulin Haptoglobin Ceruloplasmin fibrinogen Fever is produced in response to Pyrogens What are pyrogens? act by stimulating prostaglandin synthesis in the vascular and perivascular cells of the hypothalamus. Bacterial products (called exogenous pyrogens), stimulate leukocytes to release cytokines such as IL-1 and TNF (called endogenous pyrogens) that increase the enzymes (cyclooxygenases) that convert AA into prostaglandins. Fever •In the hypothalamus, the prostaglandins, especially PGE2, stimulate the production of neurotransmitters such as cyclic AMP, which function to reset the temperature set-point at a higher level. •NSAIDs, including aspirin , reduce fever by inhibiting cyclooxygenase and thus blocking prostaglandin synthesis. •fever may induce heat shock proteins that enhance lymphocyte responses to microbial antigens. Increased erythrocyte sedimentation rate •The rise in fibrinogen causes erythrocytes to form stacks (rouleaux) that sediment more rapidly at unit gravity than do individual erythrocytes. This is the basis for measuring the erythrocyte sedimentation rate (ESR) as a simple test for the systemic inflammatory response, Increased erythrocyte sedimentation rate during inflammation (ESR) TNF IL-1 IL-6 Hepatic synthesis of some plasma proteins most notably fibrinogen Rapid agglutination of erythrocytes Inflammation Systemic Manifestations Leukocytosis: WBC count climbs to 15,000 or 20,000 cells/μl most bacterial infection Lymphocytosis: Infectious mononucleosis, mumps, German measles Eosinophilia: bronchial asthma, hay fever, parasitic infestations Leukopenia: typhoid fever, infection with rickettsiae/protozoa An experiment introduces bacteria into a perfused tissue preparation. Leukocytes then leave the vasculature and migrate to the site of bacterial inoculation. The movement of these leukocytes is most likely to be mediated by which of the following substances? (A) Bradykinin (B) Chemokines (C) Histamine (D) Prostaglandins (E) Complement C3a A 32-year-old woman has had a chronic cough with fever for the past month. On physical examination, she has a temperature of 37.5°C, and on auscultation of the chest, crackles are heard in all lung fields. A chest radiograph shows many small, ill-defined nodular opacities in all lung fields. A transbronchial biopsy specimen shows interstitial infiltrates with lymphocytes, plasma cells, and epithelioid macrophages. Which of the following infectious agents is the most likely cause of this appearance? (A) Staphylococcus aureus (B) Plasmodium falciparurn (C) Candida albi cans (D) Mycobacteriurn tuberculosis (E) Klebsiella pneumo nine (F) Cytomegalovirus Time 4-6 hours to 3-5 days Vascular involvement Neutrophils Cardinal signs of inflammation Lymphatics Active hyperemia Edema, occ.fibrin thrombi Role to remove exudate Can lead to inflammation. Lymphangitis Lymphadenitis