* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Sepsis Project Presentation 3744KB Jan 14 2015 08:21:43 AM
Cancer immunotherapy wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Inflammation wikipedia , lookup
Common cold wikipedia , lookup
Rheumatic fever wikipedia , lookup
Acute pancreatitis wikipedia , lookup
Innate immune system wikipedia , lookup
Urinary tract infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Sarcocystis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Hepatitis C wikipedia , lookup
Schistosomiasis wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis B wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Infection control wikipedia , lookup
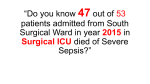
George Adolf Myths The elderly, for the most part are the only people who contract sepsis. Sepsis only affects people with preexisting conditions. Sepsis is the same thing as blood poisoning (septicemia). Sepsis and septic shock are always fatal. Incidence Over 750,000 patients are diagnosed with sepsis annually, with an increase of 90% in the number of diagnoses over the last 10 years. The cause for this is believed to be the rise of drug-resistant bacteria Mortality In otherwise healthy individuals, the mortality rate for sepsis is 5% If severe sepsis develops, mortality rises sharply If hypotension (the hallmark of septic shock) is present, mortality rises to 50% At-Risk Populations Elderly, infants, surgical patients, chronically ill and immunosupressed patients are all at increased risk of contracting sepsis because of compromised or diminished immune function. The mortality rates for these catagories are also raised. Definitions a. Sepsis – a SIRS response triggered by infection b. Septicemia – sepsis originating from an infection in the bloodstream c. Systemic Inflammatory Response Syndrome – systemic (bodywide) immune response meeting two or more of the following criteria i. Temperature above 100.4 ˚F , below 96.8 ˚F ii. HR > 90 bpm iii. RR > 20 or PaCO2 < 32 mmHg iv.Extreme high/low WBC count S/S of Sepsis a. Chills, low grade fever, shaking, body aches, N&V, vertigo, other flu-like symptoms b. Occasional AMS including confusion, lethargy and increased fatigue Purpura/rash in children with sepsis caused by meningococcal infection Influenza vs. Sepsis Sepsis can be misdiagnosed as the flu because symptoms are nearly identical often. Try to rule out sepsis when considering a diagnosis of influenza. Sources of Infection Dirty wounds (debris) Complex wounds (open fractures) Burns Puncture wounds Impaled Objects Crush Injuries Infected Wounds Progression of Sepsis a. Local infection occurs triggering non-specific inflammatory cell response i. Vasodilation occurs allowing more blood to reach infected area enhancing immune response by allowing increased movement of antibodies and immune cells (Phagocytes) into affected area in order to combat infection ii. Increased Local Vessel Permeability Increases, permits antibodies & phagocytes to move out of bloodstream into surrounding infected cells Sepsis Chain Image: various causes & signs of infection/sepsis Progression of Sepsis cont. b. Local Inflammatory Response Ineffective > infection spreads beyond original location c. Body initiates systemic inflammatory response to infection > infection becomes sepsis at this point Progression of Sepsis cont. d. Severe sepsis i. Organ dysfuntion, poor perfusion or hypotension ii. Characterized by: hypotension (<90 mmHg systolic), altered mental state, hyperglycemia w/o Hx of diabetes, hypoxemia, & decreased urine output iii. Body’s response to severe sepsis > release of histamines, prostaglandins, cytokines causing systemic vasodilation and increased capillary permeability> fluid shift from intravascular space to the extravascular space > increased systemic inflammation & relative hypovolemia causing hypotension Progression of Sepsis cont. e. Septic Shock i. When aggressive fluid replacement and vasopressors fail to maintain a SBP of at least 90 w/ continued signs of severe sepsis > pt now in septic shock (tx increasingly difficult, mortality now over 50%) Progression of Sepsis cont. f. Multiple organ dysfunction Syndrome i. Two or more organs fail to function properly, homeostasis not maintained without aggressive interventions ii.MODS will develop within 3-5 days of uncorrected septic shock iii. Final stage of an infection that has overtaken the body > death shortly Assessment a. ABCs, manage critical problems b. Complete SAMPLE hx i. How long has pt been ill? ii. Is there any hx of infections? iii. Prior medical complications/conditions? iv. Any surgeries? v. Pain or fever? c. Complete physical exam i. Sick/Not Sick ii. Signs of infection? A sign of infection A bad IV site Management of Sepsis a. Oxygen – patients with sepsis have an increased oxygen demand, oxygen supply to tissue is often inadequate even with supplemental O2 in patients with severe sepsis b. Ventilatory Support – patients with severe sepsis often require mechanical ventilatory support, consider intubation and the use of a respirator if available c. Capnography and Pulse Oximetry to maintain SpO2 above 90, and monitor PaCO2 – respiratory alkalosis (PaCO2 < 32 mmHg) is common Management of Sepsis cont. d. Monitor hypotension and use fluid replacement, Trendelenburg position to maintain adequate BP e. Initiate IV access – consider large bore IVs for aggressive Tx with crystalloid solutions, bolus in 500 mL increments to maintain SBP of at least 90 mmHg f. Consider vasopressors (dopamine) for pts not responsive to fluid boluses g. Once infection successfully located or suspected consider IV antibiotics if available – some EMS agencies are beginning to carry drugs such as Rocephin Keep in mind: Septic patients are prone to rapid deterioration, ALS providers should be utilized if available rapid transport if airway compromise or inadequate respiration; registers V,P, or U on AVPU scale; unstable vitals or oral temperature > 100˚F