* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 21 L.Interventions for Clients with Problems of the Thyroid
Survey
Document related concepts
Transcript
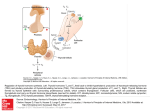
Evaluating Outcomes for Clients with Thyroid and Parathyroid Problems Hyperthyroidism Thyrotoxicosis Graves’ disease, the most frequent causes: goiter, exophthalmos, pretibial myxedema Laboratory assessment Thyroid scan Ultrasonography Electrocardiography Drug Therapy Radioactive iodine therapy; not used in pregnant women – Additional drug therapy may be needed. – Implement radiation precautions. – Monitor regularly for changes in thyroid function. Surgical Management Surgery possible in absence of good response to drug therapy. Postoperative care for: – Hemorrhage – Respiratory distress – Hypocalcemia and tetany – Laryngeal nerve damage – Thyroid storm or thyroid crisis Infiltrative Opthalmopathy Provide symptomatic treatment. Treatment of hyperthyroidism does not correct eye and vision problems of Graves’ disease. Elevate the head of bed at night. Instill artificial tears. Treat photophobia with dark glasses. (Continued) Infiltrative Opthalmopathy (Continued) Give steroid therapy. Provide diuretics. Hypothyroidism Decreased metabolism from low levels of thyroid hormones Myxedema coma a rare, serious complication Mostly a result of thyroid surgery and radioactive iodine treatment of hyperthyroidism Clinical manifestations Decreased Cardiac Output Interventions: – Monitor circulatory status. – Monitor for signs of inadequate tissue oxygenation. – Monitor for changes in mental status. – Monitor fluid status and heart rate. – Administer oxygen or mechanical ventilation, as appropriate. Ineffective Breathing Pattern Interventions: – Observe and record rate and depth of respirations. – Auscultate the lungs. – Assess for respiratory distress. – Assess the client receiving sedation for respiratory adequacy. Disturbed Thought Processes Interventions: – Assess lethargy, drowsiness, memory deficit, poor attention span, and difficulty communicating. – These problems should decrease with thyroid hormone treatment. – Provide a safe environment. – Provide family teaching. Myxedema Coma Coma, respiratory failure, hypotension, hyponatremia, hypothermia, hypoglycemia Emergency care Thyroiditis Inflammation of the thyroid gland Three types of thyroiditis: acute, subacute (granulomatous), and chronic (Hashimoto’s disease)— the most common type Dysphagia and painless enlargement of the gland Nonsurgical management, drug therapy Thyroid Cancer Papillary, follicular, medullary, and anaplastic Collaborative management Surgery treatment of choice: thyroidectomy Suppressive doses of thyroid hormone for 3 months after surgery Study performed after drugs are withdrawn Hyperparathyroidism Parathyroid glands: calcium and phosphate balance Hypercalcemia and hypophosphatemia Nonsurgical management: – Diuretic and fluid therapy – Drug therapy: phosphates, calcitonin, calcium chelators Surgical Management Parathyroidectomy care: preoperative – Client stabilized; calcium levels normalized – Studies: bleeding and clotting times, CBC – Teaching: coughing, deep-breathing exercises, neck support Operative procedures (Continued) Surgical Management (Continued) Postoperative care includes: – Observe for respiratory distress. – Keep emergency equipment at bedside. – Hypocalcemic crisis can occur. – Recurrent laryngeal nerve damage can occur. Hypoparathyroidism Decreased function of the parathyroid gland Iatrogenic hypoparathyroidism Idiopathic hypoparathyroidism Hypomagnesemia Interventions: correcting hypocalcemia, vitamin D deficiency, and hypomagnesemia If a manifestation is caused by hyperthyroidism, indicate “HYPER”. If a manifestation is caused by hypothyroidism, indicate “HYPO.” Tremors Heat intolerance Weight gain Tachycardia Insomnia Dry, coarse, brittle hair Decreased activity tolerance Decreased body temperature Palpitations Apathy Diaphoresis Thinning of scalp hair Thick, brittle nails Constipation HYPO = Hypothyroidism HYPER = Hyperthyroidism Tremors: HYPER Heat intolerance: HYPER Weight gain: HYPO Tachycardia: HYPER Insomnia: HYPER Dry, coarse, brittle hair: HYPO Decreased activity tolerance: HYPO Decreased body temperature: HYPO Palpitations: HYPER Apathy: HYPO Diaphoresis: HYPER Thinning of scalp hair: HYPER Thick, brittle nails: HYPO Constipation: HYPO The pathology of Graves’ disease is (select one) A. B. C. D. increased release of TSH (thyroid stimulating hormone) by the anterior pituitary. an autoimmune disorder in which antibodies are made and attach to the TSH receptor sites on the thyroid tissue. the development of a thyroid nodule which releases increased amounts of thyroid hormones. a lack of dietary iodine. B Graves’ disease is an autoimmune disorder in which antibodies are made and attach to the TSH receptor sites on the thyroid tissue. When these antibodies, known as thyroid-stimulating immunoglobulins (TSIs), bind to the thyroid gland, the gland increases in size and overproduces thyroid hormones. Clients with Graves’ disease also have exophthalmos (wide-eyed appearance) and pretibial myxedema. How can laboratory tests help differentiate hyperthyroidism caused by Graves’ disease versus hyperthyroidism caused from hyperpituitarism? With hyperthyroidism, both the T3 and T4 blood levels are elevated, causing hypermetabolism. An elevated free thyroxine (FT4) or Free T4 index may be more useful as it provides information about the active hormone. The FT4 is also elevated in hyperthyroidism. In Graves’ disease, the autoantibodies bind to the TSH receptor and activate it, causing an overproduction of thyroid hormones. The increased metabolic rate negatively feeds back and suppresses hypothalamic secretion of thyrotropin hormone, which in turn suppresses thyroid-stimulating hormone (TSH). The TSH is decreased in Graves’ disease. When the TSH levels are elevated despite increased synthesis of thyroid hormones, hyperpituitarism is a possible cause. If the statement is true, place a “T” before the statement. If the statement is false, place a “F” before the statement. A client is given radioactive iodine by mouth and scanned 24 hours later during a thyroid scan. Drug therapy for hyperthyroidism commonly includes antianxiety medications [alprazolam (Xanax), lorazepam (Ativan)] to relieve diaphoresis, anxiety, tachycardia, and palpitations. Results from drug therapy and from radioactive iodine therapy are usually seen in 48-72 hours. A patient with hyperthyroidism has a need for increased calories, carbohydrates, and especially proteins. A client is given radioactive iodine by mouth and scanned 24 hours later during a thyroid scan. TRUE The thyroid scan evaluates the position, size, and functioning of the thyroid gland. The uptake of the radioactive iodine is measured. Normally the thyroid has an uptake of 5 – 35% when measured at 24 hours. The uptake of radioactive iodine is increased in hyperthyroidism. Drug therapy for hyperthyroidism commonly includes antianxiety medications [alprazolam (Xanax), lorazepam (Ativan)] to relieve diaphoresis, anxiety, tachycardia, and palpitations. – FALSE – The most commonly ordered antithyroid drugs are the thioamides, including propylthiouracil (PTU) and methimazole (Tapazole), which block thyroid hormone production. – Iodine preparations decrease blood flow through the thyroid gland. This reduces the production and release of thyroid hormone. – Lithium carbonate also inhibits thyroid hormone release. – Beta-adrenergic blocking drugs, such as propranolol (Inderal) and atenolol (Tenormin), relieve diaphoresis, anxiety, tachycardia, and palpitations. Results from drug therapy and from radioactive iodine therapy are usually seen in 48-72 hours. FALSE The response to thioamides is delayed because the client may have large amounts of thyroid hormone stored that continues to be released. With the use of iodine preparations, improvement usually occurs within 2 weeks, but weeks may be needed before metabolism returns to normal. A patient with hyperthyroidism has a need for increased calories, carbohydrates, and especially proteins. TRUE The client is hypermetabolic and has an increased need for calories, carbohydrates, and proteins. Proteins are especially important because the client is at risk for a negative nitrogen balance. More questions What should be assessed to determine if antithyroid agents (such as propylthiouracil) are effective? What are common side effects associated with these drugs? Effectiveness of therapy can be demonstrated by a decrease in the severity of symptoms of hyperthyroidism. Of particular concern is the effect of the thyroid hormone activity on cardiac function. The drugs should lower the systolic BP, narrow the pulse pressure, lower the heart rate, and eliminate dysrhythmias if effective. Weight gain is another sign of effective therapy. The most common side effects are nausea, vomiting, and rash. Hypothyroidism is a possible side effect for which dose adjustment may be indicated. Indicate if the statement regarding thyroidectomy is true (T) of false (F). A client should avoid coughing following surgery. Clients are at risk for hypocalcemia following a thyroidectomy. Permanent hoarseness occurs if laryngeal nerve damage occurs. In acute respiratory obstruction, a laryngeal stridor will be heard. Neck extension should be avoided to decrease tension on the suture line. A client should avoid coughing following surgery. FALSE, BUT IT IS IMPORTANT TO SUPPORT THE NECK WHEN COUGHING OR MOVING. PLACING BOTH HANDS BEHIND THE NECK WHEN MOVING REDUCES THE STRAIN ON THE SUTURE LINE. Clients are at risk for hypocalcemia following a thyroidectomy. TRUE. THE PARATHYROID GLANDS CAN BE DAMAGED OR THEIR BLOOD SUPPLY IMPAIRED. HYPOCALCEMIA AND TETANY RESULT IF PARATHYROID HORMONE IS DECREASED. EARLY SIGNS OF HYPOCALCEMIA ARE NUMBNESS AND TINGLING AROUND THE MOUTH OR FINGERS AND TOES. Permanent hoarseness occurs if laryngeal nerve damage occurs. FALSE. THE NURSES ASSESSES THE CLIENT’S VOICE AT 2-HOUR INTERVALS AND DOCUMENTS CHANGES. THE CLIENT IS REASSURED THAT HOARSENESS IS USUALLY TEMPORARY. In acute respiratory obstruction, a laryngeal stridor will be heard. TRUE. EMERGENCY TRACHEOSTOMY EQUIPMENT IS KEPT IN THE CLIENT’S ROOM. Neck extension should be avoided to decrease tension on the suture line. TRUE. SANDBAGS AND PILLOWS ARE USED TO SUPPORT THE HEAD AND NECK. Thyroid Storm What interventions are implemented prior to a thyroidectomy to prevent the risk of a thyroid storm? What signs and symptoms are common during a thyroid storm? What are the primary concerns during a thyroid storm? Thyroid Storm Prior to surgery a clients receive antithyroid drugs, beta blockers, steroids, and iodides before to prevent thyroid crisis. Signs and symptoms of a thyroid storm are related to the increase in metabolic rate. They include fever, tachycardia, systolic hypertension, abdominal pain, N&V, diarrhea, agitation, tremors, restlessness, confusion, psychosis, and seizures, It has a mortality rate of 25%. It is important to identify the causative event. The primary concerns will be maintaining airway patency, providing adequate ventilation, and stabilizing the hemodynamic status. Myxedema During hypothyroidism, cellular energy production is decreased and metabolites build up. The metabolites are compounds of proteins and sugars called glycosaminoglycans. These compounds build up inside cells, which increases mucous and water, forms cellular edema, and changes organ texture. The edema is mucinous edema (called myxedema) rather than edema caused by water alone. Myxedema Coma A rare, serious complication of untreated or inadequately treated hypothyroidism. Decreased metabolism leads to a flabby heart increased chamber size Cardiac output decreases Perfusion to the brain and other organs decreases Decreased perfusion makes slowed cellular metabolism worse. Tissue and organ failure occurs. What is the most common reason a person seeks medical help prior to being diagnosed A. B. C. D. with hypothyroidism? (select one) Weight gain Dyspnea Depression Hoarseness C. Depression Depression is the most common reason for seeking medial attention. Family members often bring the client for the initial evaluation. The client may be too lethargic, apathetic, or drowsy to recognize changes in his or her condition. Other psychosocial changes include paranoia, agitation, disturbed thought process, and impaired memory. Indicate “T” for a true statement and “F” for a false statement. The client with more severe symptoms of hypothyroidism is started on the lowest dose of thyroid hormone replacement. A client is placed on thyroid hormone replacement until T3 and T4 level become normal, and is then gradually tapered off the medication. Increased mental awareness is a sign of effective thyroid hormone replacement therapy. Emergency care of the client during myxedema coma includes levothyroxine sodium IV. True or False The client with more severe symptoms of hypothyroidism is started on the lowest dose of thyroid hormone replacement. TRUE. This caution is especially important when the client has known cardiac problems. Severe hypertension, heart failure, and myocardial infarction can occur if the initial dose is too high or if the dose is increased too rapidly. A client is placed on thyroid hormone replacement until T3 and T4 level become normal, and is then gradually tapered of the medication. FALSE The client with hypothyroidism requires lifelong thyroid hormone replacement. True or False Increased mental awareness is a sign of effective thyroid hormone replacement therapy. TRUE Other signs of resolving hypothyroidism will also demonstrate effective therapy. Emergency care of the client during myxedema coma includes levothyroxine sodium IV. TRUE Other interventions include maintain a patent airway, replacing fluids, administering glucose IV, administering corticosteroids, checking temperature frequently, monitoring BP, covering client with warm blankets, and monitoring mental status. Conditions that could lead to hyperparathyroidism include which of the following? Indicate all that apply. Congenital thyroid dysgenesis Parathyroid carcinoma Vitamin D deficiency Hypomagnesemia Chronic renal failure with hypocalcemia. Neck trauma Causes of hyperparathyroidism include the BOLD items: Congenital dysgenesis Parathyroid carcinoma Vitamin D deficiency Hypomagnesemia Chronic renal failure with hypocalcemia. Neck trauma Other causes are parathyroid adenoma, congenital hyperplasia, neck radiation, parathyroid hormone-secreting carcinomas of lung, kidney , or GI tract. Indicate “T” for a true statement and “F” for a false statement. A client with hyperparathyroidism is at risk for pathologic fractures. Hypercalcemia associated with hyperparathyroidism is treated with dietary restriction of calcium. A positive Chvostek’s sign and Trousseau’s sign indicate hypercalcemia. Serum PTH, calcium, and phosphate levels and urine cyclic adenosine monophosphate (cAMP) are the most commonly used laboratory tests to detect hyperparathyroidism. True or False A client with hyperparathyroidism is at risk for pathologic fractures. TRUE An increased rate of bone destruction occurs when the levels of PTH are high, resulting in pathologic fractures, bone cysts, and osteoporosis. Hypercalcemia associated with hyperparathyroidism is treated with dietary restriction of calcium. FALSE A diuretic and fluid therapy is the most common method used to lower calcium. Other drug therapy includes oral phosphates, calcitonin, and calcium chelators such as Mithramycin. True or False A positive Chvostek’s sign and Trousseau’s sign indicate hypercalcemia. FALSE Low calcium levels are associated with increased neuromuscular activity. Chvostek’s and Trousseau’s are found in hypocalcemia. Serum PTH, calcium, and phosphate levels and urine cyclic adenosine monophosphate (cAMP) are the most commonly used laboratory tests to detect hyperparathyroidism. TRUE In hyperparathyroidism, serum PTH is increased, calcium is increased, phosphate is decreased, and urinary cAMP is increased.