* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Soft Tissue Infection Case Study 1
Survey
Document related concepts
Transcript
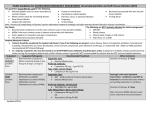
Soft Tissue Infection Case Study 1 By: Linda Iskandar The Case A 52 year old female BIBA Presents with cellulitis of left lower leg Painful, swollen and erythematous left lower leg Febrile (38.5 C), Tachycardic (HR 118/min), with mild hypotension ( BP 105/65) Patient was hyperglycaemic BGL (23 mmol/L) Allergic to penicillin Patient weighs 110 Kg Patient/social history NIDDM Hypertension GORD Past ulceration of lower leg Hypothyroidism Hypercholesterolemia Depression osteoarthritis Social history: Ex smoker Non alcohol Lives at home by herself Medication chart Medications Metformin Gliclazide Ramipril Esomeprazole Thyroxine Atorvastatin Sertraline Diazepam Paracetamol Dose 1000mg 1 tds 80mg 1 bd 10mg 1 d 40mg 1 d 50 mcg 1 d 40 mg 1 d 50mg 1 d 1 d prn 665mg 2 tds Indications NIDDM NIDDM Blood pressure GORD Hypothyroidism Hypercholesterolemia Depression Anxiety Osteoarthritis Blood results Test 16/03/09 15/03/09 12/03/09 Reference Range WCC 25.3 x 109/L 22.2 x109/L 19.7 x 109/L 5-15 x 109/L Neutrophils 14.3 x 109/L 12.3 x109/L 10.1 x 109/L 2.1-7 x 109/L Creatinine 93 umol/L 89 umol/L 90 umol/L 60-140 umol/L Hb 127g/L 130g/L 129 g/L 120-155 g/L CRP 389 mg/L 343mg/L 290 mg/L < 10mg/L No major drug interactions where found and physical examination and systemic symptoms were suggestive of cellulitis Cellulitis Cellulitis is a bacterial infection of the skin affecting the dermis and subcutaneous tissue. The main bacteria responsible for cellulitis are Streptococcus and Staphylococcus. Cellulitis may occur anywhere on the body, but the lower leg is the most common site of infection. It usually begins as a small area of tenderness, swelling, and redness that spreads to adjacent skin. This area then begins to enlarge, and following symptoms maybe experienced; Redness of the skin Warmth Swelling Tenderness or pain in an area of skin Discharge, such as leaking yellow clear fluid or pus. http://www.cancer.umn.edu/cancerinfo/NCI/Media/CDR0000579036.jpg Cellulitis Risk factors: Immunosuppression Diabetics Obesity Wounds (surgical and non-surgical) History of peripheral vascular disease Treatment: First line – di/flucloxacillin 2g IV Q6H Patients allergic to penicillin; Cephazoline 2g IV Q8H Clindamycin 450mg IV or orally Q8H Course of events 11/03: Patient started on IV Ceftriaxone for cellulitis, Actrapid for hyperglycaemia and IV fluids. Ceftriaxone Ceftriaxone belongs to the antibacterial group Cephalosporins and it is one of the broad spectrum antibiotics. This group of antibiotics contain a betalactam ring that interferes with the bacterial peptidoglycan synthesis. It is therefore bactericidal and effective against gramnegative and gram positive organisms. Course of events 13/03: Patient is intermittently febrile with no improvement, blood cultures negative. 16/03: Still no improvement and increased oedema of subcutaneous tissue. 17-18/03: Pustules developed and spread to dorsum of foot and upper leg with signs of fat necrosis. Necrotising fasciitis Necrotising fasciitis (NF) more commonly known as “flesheating disease” is a rare infection of the subcutaneous tissues, and it is more commonly seen in immune compromised patients. There are many types of bacteria that might be the cause for NF these include; Group A streptococcus (Streptococcus pyogenes), Staphylococcus aureus (MRSA), Vibrio vulnificus, Clostridium perfringens, Bacteroides fragilis. But the organism that is most commonly found to cause NF is group A beta-hemolytic streptococci, and normally develops from a previous complicated wound. Pathophysiology The bacteria spreads form the subcutaneous tissue along the superficial and deep fascial planes. This facilitation happens by bacterial enzymes and toxins, which leads to vascular occlusion, ischemia, tissue necrosis and superficial nerves damage. The following two factors are needed to promote bacterial growth in NF. 1. Surface protein expression: M1 and M3 surface proteins increase the adherence of streptococci to the tissue, they also work by protecting the bacteria from phagocytosis. 2. Toxin production: Streptococcal pyrogenic exotoxins (SPEs) A,B and C these release exotoxins that activate the T-cells and leads to the overproductions of cytokines. Signs and symptoms NF symptoms begins with fever and chills. After 2-3 days, erythema is noted, with redness, swelling and blister formation. NF may develop after chronic venous leg ulcers and skin blister. NF may also occur in the setting of diabetes mellitus, surgery, trauma, or infectious processes. Course of events cont... 19/03: Blood cultures still negative, IV Clindamycin added. 20/03: Debridement of skin, subcutaneous tissue and deep fascia of all affected areas. Slowly the erythema and oedema reduced and there were no signs of necrosis. Clindamycin Clindamycin belongs to the antibacterial group lincosamides. It works by reversibly binding to the 50S sub-unit of bacterial ribosome inhibiting its protein synthesis and preventing peptide bond formation. It is bacteriostatic against a variety of gram +ve aerobic and anaerobic organisms. Clindamycin Gram positive aerobes Staphylococcus aureus Streptococcus pneumoniae Strep pyogenes Anaerobes Clostridium perfringens Fusobacterium necrophorum Peptostreptococcus anaerobius Protozoa Plasmodium falciparum. Also used in the treatment of Chlamydia trachomatis and Gardnerella vaginalis NF treatments The most effective treatment is to perform surgical debridement or in severe cases amputation as to prevent further spreading, along with IV antibiotics (vancomycin or clindamycin) and hyperbaric oxygen therapy (HBOT). The inclusion of clindamycin in the initial antibiotic regimen has been associated with a better outcome in streptococcal toxic shock, this could possibly be due to its inhibition of bacterial protein synthesis and thereby reduces toxin production. Surgical Debridement Surgical debridement is a fast and selective procedure that effectively results in the removal of the patient's dead, damaged, or infected tissue in order to promote healing of the surrounding healthy tissue. Courses of events cont…. 22/03: Patient was transferred to Prince of Wales hospital for hyperbaric oxygen treatment Hyperbaric oxygen therapy (HBOT) HBOT is sometimes used in treatment of NF depending on the severity of the infection. It works by providing 100% oxygen at a higher than atmospheric pressure. The oxygen is used to inhibit anaerobic bacterial growth and promote tissue recovery. HBOT has been shown to further reduce morbidity and mortality by about 10%-20% in some patients when used in conjunction with antibiotics and surgery. Take Home Message Control the infection before the patient is discharged. Necrotising fasciitis can commonly be mistaken for cellulitis. Provide the patient with preventive measured to inhibit the infection from coming back (e.g. refer to community wound care clinic) Educate on the different signs and symptoms that the patient needs to look out for especially because she is a diabetic. Educate the patient on the importance of QUM and consider Webster pack to help with compliance. Promote healthy eating habits and moderate exercise References 1. 2. 3. 4. 5. 6. 7. 8. 9. Australian Medicines Handbook, 2010. Australian Medicines Handbook Pty Ltd. Adelaide, Australia. Walker R, Edwards C. (2003). Clinical Pharmacy and Therapeutics. Churchill Livingstone 4th edition; (chapter 37). Groote De M.A. And Johnson P. (2004). Skin, bone and soft tissue infections. World health organisation; (chapter 8). McNamara, D.R., I.M. Tleyjeh, E.F. Berbari, B.D. Lahr, J.W. Martinez, S.A. Mirzoyev, and L.M. Baddour. "Incidence of Lower-Extremity Cellulitis: A Population-Based Study in Olmsted County, Minnesota." Mayo Clin Proc. 82.7 July 2007: 817-821. Cellulitis. Last accessed 25th February; available at: http://www.merckmanuals.com/home/sec18/ch211/ch211b.html Bisno AL, Stevens DL. (1996). Streptococcal infections of skin and soft tissues. N Engl J Med 334: 240-245. Treatment of soft tissue infections. Last accessed 25th February , available at: http://www.who.int/water_sanitation_health/emerging/en/patmycrobact8.pdf. Hersh AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med. Jul 28 2008;168(14):1585-91. skin image. Last accessed 28th February 2011, available at: http://www.cancer.umn.edu/cancerinfo/NCI/Media/CDR0000579036.jpg 8. 9. 10. 11. 12. Ellis Simonsen SM, van Orman ER, Hatch BE, et al. Cellulitis incidence in a defined population. Epidemiol Infect. Apr 2006;134(2):293-9. Davies HD, McGeer A, Schwartz B, et al. Invasive group A streptococcal infections in Ontario, Canada. Ontario Group A Streptococcal Study Group. N Engl J Med. Aug 22 1996;335(8):547-54. Cephalosporin. Last accessed 28th February 2011, available at: http://www.emedexpert.com/compare/cephalosporins.shtml Cellulitis image. Last accessed 28th February 2011, available at: http://www.google.com.au/imgres?imgurl=http://findmeacure.com/wp-content /uploads/2008/03/cellulitis_left_leg.jpg&imgrefurl=http://findmeacure.com/200 8/03/04/cellulitis/&usg=__3Suw8XSrbscuH0f5a-_XFQfhdTc=&h=482&w= 640 &sz=80&hl=en&start=2&zoom=1&um=1&itbs=1&tbnid=1jtZEaU3zf_m4M:&t bnh=103&tbnw=137&prev=/images%3Fq%3Dcellulitis%26um%3D1%26hl%3D en%26sa%3DN%26tbs%3Disch:1&ei=QbKGTdrpJI-lcfO3kJUD. Cellulitis image. Last accessed 28th February 2011, available at: http://www.google.com.au/imgres?imgurl=http://rpmedia.ask.com/ts%3Fu%3D /wikipedia/commons/thumb/6/60/Cellulitis3.jpg/190px-Cellulitis3.jpg&imgrefurl =http://www.ask.com/wiki/Anaerobic_cellulitis&usg= __5YFjswgembbFYmdiky 7Sbr6CeW8=&h=1632&w=1224&sz=271&hl=en&start=25&zoom=1&um=1&it bs=1&tbnid=-Hsyhm_7Ffmx_M:&tbnh=150&tbnw=113&prev=/images%3Fq%3 Dcellulitis%26start%3D20%26um%3D1%26hl%3Den%26sa%3DN%26ndsp%3D 20%26tbs%3Disch:1&ei=MbOGTaSIPIzQcdHlqbQF