* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Respiratory Physiology
Cushing reflex wikipedia , lookup
Freediving blackout wikipedia , lookup
Intracranial pressure wikipedia , lookup
Homeostasis wikipedia , lookup
High-altitude adaptation in humans wikipedia , lookup
Hemodynamics wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Cardiac output wikipedia , lookup
Physiology of decompression wikipedia , lookup
Alveolar macrophage wikipedia , lookup
Circulatory system wikipedia , lookup
Organisms at high altitude wikipedia , lookup
Haemodynamic response wikipedia , lookup
Common raven physiology wikipedia , lookup
RESPIRATORY
PHYSIOLOGY
What will we discuss in this chapter?
(Outline)
I. Pulmonary ventilation *
1.Mechanisms of pulmonary ventilation
2.Indexes of pulmonary ventilation function
II. Pulmonary gas exchange and Tissue gas exchange
1. Principles of gas exchange *
2. Pulmonary gas exchange *
3. Tissue gas exchange
III. Gas transport in the Blood
1. Transport forms of oxygen and carbon dioxide in the blood
2. Oxygen transport *
3. Carbon dioxide transport *
IV. Respiratory Regulation
1. Respiratory centers and formation of respiratory rhythm
2. Reflex regulation of respiration *
V. Role of the lungs in regulation of acid-base balance
Respiration System
Respiratory component element
Respiration is the exchange of gas between the body and the
environment.
External respiration : the exchange of gases between pulmonary
blood and the external environment, which involves not only
diffusion across the lung capillaries (pulmonary gas exchange,
but also the bulk movement of gases in and out of the lungs
(pulmonary ventilation,
Internal respiration : the exchange of gases between the tissue
cells and the systemic capillaries. The diffusion of gases
between the interstitial fluid and the cytoplasm.
Gas transport in the blood : physical solvation and chemical
constitution.
I.
Pulmonary ventilation
1. Mechanisms of pulmonary ventilation
pulmonary ventilation
Definition *: Pulmonary ventilation is the exchange of gas between the
alveoli and the environment.
Functional structure of pulmonary ventilation
Conducting airway and lung
Thorax and respiratory muscle
Pleural cavity and intrapleural pressure **
pulmonary ventilated dynamic *
pulmonary ventilated resistance *
Respiratory work
(1) Functional structure of
ventilation
pulmonary
① Conducting airway and
lung
Conducting airways
Nose, pharynx larynx are upper respiratory tract,
and others are lower respiratory tract
The conducting airways
warm and humidify the
inspired air but are not a
site of gas exchange.
The alveoli are composed of
a single layer of epithelial
cells and are the site for gas
exchange.
The combined surface
area of the alveoli is
approximately that of a
tennis court.
Distribution and resistance of
conducting airways
Defense mechanism of conducting
airways
Defense mechanism of conducting airways
Overview of lung function and
structure
•
•
•
•
•
Lung Functions
Lungs are a site for gas exchange
with the external environment.
Regulate acid-base balance.
Lungs have a defense mechanism.
Lungs are a blood reservoir.
Serve a biosynthetic function.
Lungs Anatomy
Lung Structure
• Lungs are composed of three basic elements:
conducting airways, alveoli, and blood supply.
• Conducting airways enable air to reach alveoli and
warm and humidify the air.
• Alveoli are blind sacs where gases in the inspired air
exchange with the blood.
• Blood supply provides the heat and moisture to warm
and humidify the inspired air and the nutrients for lung
tissue, and it is the site of exchange between the body
and inspired air.
Pneumocytes I and pneumocytes II
Blood Supply
Blood Supply for Gas Exchange
Blood Supply for Gas Exchange
The intersection of lung with the
external environment is huge
• An advantage: beneficial to gas exchange and
regulating acid-base balance.
• An disadvantage: exposed to foreign substances
which need more defense.
• Approximately 20% of the total blood volume
resides in the pulmonary vasculature normally,
but changes in the cardiac output.
• Lungs synthesize substances such as
leukotrienes from arachidonic acid, convert
substances to their active from.
② Thorax and respiratory muscle
(thorax)
Chamber—the chest
Contraction of the external intercostal
muscles makes chest volume larger
Contraction of the external intercostal
muscles makes chest volume larger
Diaphragm is the main muscle of
inspiration
Dome-shaped
Inspiration
Expiration
③ Pleural cavity and
intrapleural pressure
Pleural cavity, a room between the partial pleura and
the visceral pleura, a closed space that is not connect
to the outside air.
Intrapleural pressure forming *
Intrapleural pressure=-lung retractive pressure
Why?
Intrapleural pressure is always negative, less than
atmospheric pressure for whole life time.
Intrapleural pressure is as medium resulting in that
chest movement changes lungs volume.
Formation of intrapleural pressure
Formation of intrapleural pressure
Intrapleural Space
The chest consists of the rib cage and the diaphragm. Because of
the natural elastic properties of the chest wall and lungs, the chest
wall wants to expand and the lungs want to contract.
Pleural cavity and
intrapleural pressure
Physiological significance **
•Intrapleural pressure increases lungs expansion
for inspiration and ventilation.
•Intrapleural pressure increases backflow of
venous blood and lymphatic fluid to heart.
Intrapleural pressure and diseases
This produces
difficult breath
Pneumothorax
(2) Pulmonary ventilated dynamic
Moving air into and out of the lungs
(ventilation)
①Lung-Chest Interaction
• Lungs are suspended within a closed chamber—the chest.
• Functional residual capacity (FRC) is the equilibrium
volume when the elastic forces of the chest wall and lungs
are balanced.
• Changes in chest volume are responsible for changes in
lung volume.
• The chest consists of the rib cage and the diaphragm.
Because of the natural elastic properties of the chest wall
and lungs, the chest wall wants to expand and the lungs
want to contract.
Pressures in the lungs and chest
• Alveolar pressure is the pressure within the
lungs.
• Intrapleural pressure* is the pressure between
the chest wall and lungs.
• The pressures within the lungs and chest are
small in magnitude, being measured in
centimeters of water rather than in millimeters
of mercury.
② Pulmonary ventilated mechanism
• Direct dynamic: Pressure difference between atmosphere and
alveolar gas.
• Original dynamic: Contraction and relaxation of respiratory muscles
induce thoracic cavity changes (expansion or diminution)
• Pressure difference between atmosphere and alveolar gas results in:
– Lung extension (Inspiration), alveolar pressure< atmosphere, gas
in.
– Lung retraction (Expiration), alveolar pressure>atmosphere, gas
out.
• Mechanism of artificial respiration:
Making pressure difference between atmosphere and
alveolar gas to result in pulmonary ventilation.
Inspiration and Expiration
Inspiration and Expiration
Inspiration
During inspiration and
expiration, changes in
intrapleural pressure
alter alveolar pressure,
which generates a
pressure gradient
leading to airflow and
volume changes. The
temporal relationship
between these various
parameters is
illustrated in this figure.
Expiration
0.5
Volume Change (L)
0
-5
Intrapleural Pressure (cm H2O)
-8
+0.5
Air Flow (L/sec)
0
-0.5
+1
0
-1
Alveolar Pressure (cm H2O)
Inspiration and Expiration
•Inspiration:
diaphragm conrtraction→chest volume↑→intrapleural pressure
↓→lungs expansion→alveolar pressure<atmospheric pressure →air
is sucked into the lungs.
(At the end of an inspiration, alveolar pressure=atmospheric pressure
and airflow stops )
•Expiration:
diaphragm relaxation→chest volume↓→intrapleural pressure ↑→lungs
conrtraction→alveolar pressure>atmospheric pressure→ air is pushed
out of the lungs. Therefore, expiration is a passive process.
(At the end of an exspiration, also alveolar pressure=atmospheric
pressure and airflow stops )
•Stronger ventilation:
muscles of the chest wall help produce changes in chest volume
beyond that produced by the contraction and relaxation of the
diaphragm.
Contraction of the external intercostal muscles helps
increase the volume of the chest for stronger inspiration.
while contraction of the internal intercostal muscles helps to
decrease chest volume for stronger expiration.
•
Breathing pattern
• Abdominal breathing: induced by diaphragm
contraction or relaxation;
• Thoracic breathing: resulted from external
intercostal muscles contraction or relaxation;
• Combined breathing:
Abdominal breathing + Thoracic breathing
• Connection with clinic
Breathing pattern
Eupnea (quiet breathing): diaphragm and external intercostal
muscles are the main muscle of inspiration under resting
conditions.
– Contraction of the muscles increases chest volume inflating the
lungs.
– Expiration is a passive process (without muscle contraction).
– Muscles of the rib cage augment the action of the diaphragm.
Forced breathing (deep breathing, gasping, dyspnea):
Inspiration and expiration are active process with many muscles
contraction.
Amplitude of intrapulmonary pressure change is
related to breathing frequency, extent and unobstructed
respiratory tract.
Inspiration
Expiration
Eupnea:
-2~-1 mmHg
1~2 mmHg
Forced breathing: -100~-30 mmHg
60~140 mmHg
(3) Pulmonary ventilated resistance
thoracic elastic
resistance
elastic
resistance,70%
Respiratory
esistance
lung elastic
1/3
retracting force
lung elastic
resistance
2/3 lung surface
tension
inertial resistance
non-elastic
resistance 30%
viscous resistance
air way resistance
(80%一90%)
① Relationship between elastic
resistance and compliance
Elastic resistance (ER):
ER increased, not easily make lung`s deformation, and compliance used measures ER
Compliance, C *: it is expansibility of elastic tissue with external force action.
Relationship: C=1/ER
Change: easy extension→large compliance→small elastic resistance→easy inspiration.
Compliance, C
= △V
△P
unit:L/cmH2O
② Lung compliance, CL
lung volume %
• Definition: changes of transpulmonary
volume induced by changes in
transpulmonary pressure
• CL= △V/ △Ptp
– transpulmonary pressure
= alveolar pressure (PA)-intrapleural
pressure (Pip)
– eupnea, CLis about 0.2 L/cm H2O
• Influencing factors
– size of lung volume
• specific compliance, Csp :
compliance of unit lung volume
– respiratory phase
– body position
– Abnormal pulmonary surfactant
Lung compliance
curve
Transpulmonary pressure cmH2O
specific complaince=
eupneic compliance
(L/cmH2O)
functional residual volume
③Thoracic compliance, CT
thoracic volume %
CT=change in thoracic volume/change in
transmural pressure
– transmural pressure
= intrapleural pressure-atmospheric
pressure of outside chest wall
– CT is about 0.2 L/cm H2O
Functional
residual
volume
Thoracic compliance curve
transmural pressure cmH2O
Large slope of curve middle section, big compliance and small resistance; When
lung volume is justo major or justo minor, curve slope become smaller and elastic
resistance larger.
When lung volume is 67% of total lung capacity, transmural pressure is zero, and
chest is at a natural (neutral) position without thoracic morphing (deformation), and
does not display the elastic resistance (recoil force=0).
Lung volume <67% of total lung capacity, oppressive chest produce a elastic
recoil force outwards which is inspiratory dynamic and expiratory resistance.
Lung volume >67% of total lung capacity, oppressive chest produce a elastic
recoil force inwards which is expiratory dynamic and inspiratory resistance.
④ Lung-thorax compliance,CLT
• Changes in lung volume induced by unit transmural pressure
transmural pressure (Pt)=alveolar pressure(PA)-chest surface pressure (Pcs)
• CLT =1/R = 1/(RL+RT) = 1/(1/CL+1/CT)
Normal value: 0.1 L/cm H2O
lung volume %
• Normal equilibrium position of
pulmonary retractive force inward
and thoracal recoil force outward
is the level at 40% of total lung
capacity, which determine
numerical value of intrapleural
pressure and functional residual
volume.
transmural pressure cmH2O
physiological saline filling
lung collapse
⑤ pressure-volume
curve
Difference of
pressure-volume
curve between lungs
inflation and collapse,
and after deformation
can not rapidly
recover to its original
state.
lung volume
Hysteresis(滞后现象
)
air filling
intrapulmonary pressure
Cat`s pressure-volume curve in vitro
Lung Filling with physiological saline induces lung expansion with small
pressure, and whole lung filling requires lower pressure, hysteresis of empty
is not obvious after filling.
Pressure of filling lung with air is much larger than with physiological saline
(about 3 times) Reason: filling with air makes a liquid-air interface in alveolar
lining liquid and alveolar gas, then produce surface tension.
⑥ Surface tension, T
• Definition: with liquid-air interface, liquid surface contractility
made by liquid intermolecular gravitation.
• surface tension of spheric liquid-air interface is toward centrer
and make pulmonary alveoli contractible producing elastic
resistance.
Laplace`s law: P = 2T/ r
P: stand for the additional pressure
(retractive pressure) produced by
alveolar surface tension;
T: represents surface tension;
r: radius of curvature.
⑦ Pulmonary surfactant
Component: dipalmitoyllecithin (二 DPL, DPPC)
It is secreted by type II pneumocytes and monomolecular layer
distributed on liquid-air interface, and its density changes with changes
in alveolar volume, and its function is mainly to decrease surface
tension (2/3 of total surface tension )
Physiological significance **
It is beneficial to maintain alveolar volume (stability);
It reduces interstitial fluid production of lung interstitial tissue
and alveolar cavity to prevent pulmonary edema;
It decreases inspiratory resistance, reduces inspiratory work
and help pulmonary ventilation and lung expansion.
Surfactant, a phospholipid
secreted by type II pneumocytes
Alveolar volume changes with or
without surfactant
Surfactant
lowers the
surface
tension of
alveoli and
causes
surface
tension to
change with
volume, than
keeps alveolar
pressure
constant.
Neonatal respiratory distress
syndrome, NRDS
Alveolar volume changes
without surfactant
The surface tension of alveoli would cause small alveoli
to empty into larger alveoli if it were not for the effect of
surfactant. Clinic relation… Neonatal respiratory distress
syndrome, NRDS
Alveolar pressure does not
changes with surfactant
Law of
Laplace:
P=2T/r
Small-volume alveoli have a small surface tension while
large-volume alveoli have a large surface tension. This
enables alveoli of unequal size to exist side-by-side.
⑧ Non-elastic resistance
Inertial resistance
Viscous resistance
Airway resistance
Airway resistance is 80%一90% of total non-elastic resistance.
airway resistance, (AR)
=(atmospheric pressure-intrapulmonary pressure) (cmH2O) /unit time gas
flow rate (L/s)
•Influencing factor:
– airspeed
– airflow pattern
• laminar flow, R=8ηL/πr4,
• turbulent flow, R‘=fL/4π2r5
– airway calibre
– lung volume
•Distribution of airway resistance
more AR is upper respiratory tract (most AR at nasal cavity).
Resistance to air flow
• Medium-sized bronchi are the major site
of resistance.
• Autonomic nervous system and inspired
irritants alter resistance.
• Changes in lung volume alter resistance
because bronchi are supported by lung
tissue.
Medium-sized bronchi are the
major site of resistance
The contractile activity of the bronchiolar smooth muscle is influenced by
the autonomic nervous system (sympathetic nerve, relaxation, resistance↓;
parasympathetic nerve, contraction, resistance↑). Irritants such as
cigarette smoke cause an increase in resistance. An increase in lung
volume reduces resistance because the bronchi are pulled open. Patients
with elevated airway resistance often breathe from an elevated FRC in an
attempt to reduce the resistance.
(4) Respiratory work
• Work done by that respiratory muscles overcome elastic
resistance and non-elastic resistance to realize pulmonary
ventilation.
• It is 3~5 % of total body energy consumption and it is very small.
2. Indexes of pulmonary ventilation
function
(1) Lung Volumes and Capacities
• Four terms describe specific volumes
of the lungs: tidal, expiratory reserve,
inspiratory reserve, residual
• Four terms describe lung capacities:
functional residual, inspiratory, vital,
total lung
Measure of lung volumes
and capacities
Lung volumes and capacities *
• The change in lung volume needed to move air in and out is
called tidal volume (TV). During quiet breathing, tidal
volume results from the contraction-relaxation of the
diaphragm.
• The maximum lung volume that can be achieved above tidal
volume is called inspiratory reserve volume (IRV).
• The minimum lung volume that can be achieved below tidal
volume is called expiratory reserve volume (ERV).
• Like the heart, the lungs cannot be completely emptied. The
amount of air remaining in the lungs after a forced
expiration is called the residual volume (RV).
• The four lung volumes are combined in various ways to
calculate four lung capacities.
• ERV+RV=Functional residual capacity (FRC)
• TV+IRV=Inspiratory capacity (IC)
• ERV+TV+IRV=Vital capacity (VC)
• RV+ERV+TV+IRV=Total lung capacity (TLC)
* Functional residual capacity (FRC)
• The volume at which these two opposing forces (lungs,
contraction and chest, expansion) balance is called the
functional residual capacity (FRC).
• At FRC,the lungs and chest wall are in the “rest” position
where forces are balanced and the pressure within the
lungs equals atmospheric pressure.
• Inspiration begins from FRC.
• By the intrapleural space, changes in the chest volume,
make that the lungs are pulled along and their volume also
changes.
Lung volumes and capacities
Inspiratory Reserve
Volume (3000 mL)
Vital Capacity
Inspiratory
(4600 mL)
Capacity (3500 mL)
Tidal Volume
(500 mL)
EXpiratory Reserve
Volume (1100 mL)
Functional Residual
Residual
Volume (1200 mL)
Capacity (2300 mL)
The quantity of air moved by the lung can be divided into
various volumes and capacities. Their relationship to one
another is diagramed in this figure.
Lung volumes and capacities
Lung volumes and capacities
can be used to describe lungs
function in the hospital
(2) Dead space volumes
• Dead space is the volume of air that does not
reach areas of the lung where gas exchange
occurs.
• Anatomical dead space is due to the conduction
airways (150 mL).
• Alveolar dead space is due to alveoli that receive
inadequate blood flow (150 mL).
• Physiological dead space is the sum of
anatomical and alveolar dead spaces.
Dead space volumes
(3) Pulmonary ventilation
•Minute ventilation volume, Vm
•Vm =tidal volume×respiratory frequency
•Maximum voluntary ventilation
•ventilatory reserve percentage
=
Maximal voluntary ventilarion- Minute ventilation volume
×100%
Maximal voluntary ventilarion
Alveolar ventilation **:
=(tidal volume-dead space )×respiratory frequency
It is a pulmonary ventilative accurate estimating index
Ventilation Equations
• Minute ventilation is the total volume of air moved
into the lungs per unit time and equals the tidal
volume times the breathing frequency (MV=TV×F).
• Alveolar ventilation measures the volume of air
that actually reaches the alveoli per unit time
because it takes into account dead space volume
[VA =(TV-DS)×F ].
• Increasing tidal volume overcomes the effect of
dead space volume.
TABLE
Tidal Volume
(mL)
F
(breaths/min)
MV
(mL/min)
VA
(mL/min)
300
20
6000
3000
500
12
6000
4200
600
10
6000
4500
150
40
6000
0
Ventilation is uneven within the lungs
•The weight of the lungs produces uneven inflation of alveoli.
Lungs weight make different alveolar volume at the top and
bottom of the lungs (e.g. alveoli at the top of the lungs are at
a larger volume (more negative intrapleural pressure) than
those at the base (less negative intrapleural pressure).
Alveoli also exhibit a changing compliance as volume
changes. Those at the base are ventilated more than those
at the top of the lung (compliance regulation).
•Surfactant helps alveoli of different sizes remain inflated.
Surfactant can reduce surface tension which tries to make
the alveoli smaller, and keep alveolar pressure constant.
II. Pulmonary
gas exchange and Tissue
gas exchange
1. Principles of gas exchange *
General Considerations
• Dynamical movement of gas depends on gas partial pressure, that is to
say, driving force for gas movement is the difference in gas partial
pressure.
• Physical diffusion and amount of blood flow influence the amount of a
gas in the blood.
O2
Pulmonary
alveolus
pulmonary capillary blood
CO2
gas exchange
• gas exchange
O2
Tissue gas
blood
histiocytes
exchange
CO
2
2. Pulmonary gas exchange
• Gas partial pressure, e.g. Po2 is 160 mm Hg (21% of 760 mm Hg).
• Gas movement between alveolar air and blood is a passive
process (pulmonary gas exchange) determined by the
concentration gradient for the particular gas.
• Normally, the partial pressure of oxygen is high and the partial
pressure of carbon dioxide is low in alveolar air. The opposite is
true for the partial pressure of these gases in the blood entering
the lungs.
• It is these differences in partial pressures that produce the driving
force for oxygen to enter the blood and carbon dioxide to leave the
blood as blood flows through the alveolar capillary bed.
Partial pressure of O2 and CO2 in
alveoli, blood and tissue (mmHg)
Alveoli
O2
O2
O2
CO2
CO2
Venous
Blood
O2
CO2
Arterial
Blood
Pulmonary Capillary
Heart
O2
O2
CO2
O2
CO2
Tissue Capillary
CO2
Pulmonary gas exchange and tissue
gas exchange
Movement of gas between alveolar air and
blood
Gas Composition of Alveolar Air
• Partial pressures of oxygen and carbon dioxide in
alveolar air are not the same as those in
atmospheric air.
• Humidification lowers the Po2 of inspired air.
• Po2 of alveolar air is lower than inspired air because
of uptake by the blood.
• Carbon dioxide diffusing from pulmonary arterial
blood into alveolar air raises alveolar Pco2
compared to that of inspired air.
Pulmonary gas exchange and
tissue gas exchange
Influencing factors of pulmonary gas
exchange **
• Fick’s law of diffusion relates four factors that
determine the amount of gas transferred
through a sheet of tissue: (1) cross-sectional
area, (2) partial pressure, (3) diffusion constant,
(4) thickness, and (5) ventilation/perfusion
ratio.
• Diffusion constant is related to the gas
solubility and molecular weight.
• Movement of oxygen and carbon dioxide are
not limited by diffusion.
Influencing factors of
pulmonary gas exchange *
Fick’s law
Fick's law is a mathematical expression of some factors
Gas diffusion is proportional to
Surface area× Diffusion constant× Partial pressure gradient
Thickness
The physical properties of O2 and CO2 enable them to diffuse
rapidly between the alveolar air and the blood. Therefore, the
amount of these gases in the blood is not limited by diffusion.
O2 solubility
O2 solubility
O2 solubility
CO2 solubility
Respiratory membrane
Interocclusal
Alveolar Epithelial Base Membrane
Capillary Base Membrane
Capillary Epithelial Cells
Clearance
Alveolar Epithelial Cells
Liquid Layer Containing
Alveolar Surfactant
Normally, area of
Respiratory
membrane is very
large being
beneficial to gas
exchange
RBC
RBC
Alveoli
Capillary
RBC
Structural Diagram of Respiratory membrane
Respiratory membrane
Thickness of
Respiratory
membrane is
close related
to clinic
diseases
Normally,thickness
of Respiratory
membrane is very
small being
beneficial to gas
exchange
Blood flow affects the
amount of gas in the blood
• The amount of gas dissolved in
blood can be limited by pulmonary
blood flow.
• The amount of oxygen and carbon
dioxide in the blood is limited by
perfusion.
Movement of blood through the lungs
Overview of Pulmonary Blood Flow and Resistance
• The volume of blood flow through the lungs is the same as
through the systemic circulation but because the resistance
is lower (about one tenth the resistance of the systemic
circulation) , pressure is lower too.
• Pulmonary vascular resistance is increased by
norepinephrine, serotonin, and histamine; while adenosine,
acetylcholine, and nitric oxide decrease resistance.
• Reduced alveolar oxygen (hypoxia) causes increased
pulmonary vascular resistance.
Lung volume affects pulmonary
vascular resistance
• Pulmonary vascular resistance increases at both small and
large lung volumes because alveolar and extra-alveolar
vessels are affected differently by changes in lung volume.
• The capillaries are not supported by connective tissue, their
caliber is influenced by alveolar volume.
• At large lung volumes (ie, large alveolar volume), capillaries
are compressed, which raises their resistance to blood flow.
• At small lung volumes (ie, small alveolar volume), the
connective tissue is not stretched, allowing the extraalveolar vessel to narrow, and resistance is high at low lung
volumes because of extra-alveolar vessel narrowing.
Blood flow is uneven
within the lungs
• Gravity causes blood pressure and
therefore blood flow to be greater at the
base than at the top of the lung.
• Just as gravity produces regional
differences in alveolar inflation (see
Ventilation is uneven in the lungs), it also
produces regional differences in blood
flow.
Balancing ventilation and
perfusion
Normal Ventilation-Perfusion Imbalance
• Regional differences in ventilation and blood flow cause
the top of the lung to be overventilated and the bottom of
the lung to be overperfused under normal conditions.
• Regional differences in the ratio of ventilation to perfusion
result in regional differences in gas exchange from the top
to the bottom of the normal lung.
• Because of ventilation-perfusion imbalance, blood leaving
the top of the lung has a higher Po2 and a lower Pco2 than
blood leaving the base of the lung.
Normal ventilation-perfusion
imbalance
VA / Q mismatch from top to
bottom of the lung
Normal ventilation-perfusion
imbalance
Perfusion ( Q )
1
Ventilation ( VA )
Ve
nti
lat
io
n
or
Pe
rf
us
io
n
L/
mi
n
0
Apex of Lung
Base of Lung
Because of the effect of gravity, lung perfusion (Q),
and ventilation (VA) increase from the top (apex) to
the bottom (base) of the lung.
Normal ventilation-perfusion
balance
Venous Blood Turn into Arterial Blood Which realizes
Pulmonary Gas Exchange Efficiently.
Normal ventilation-perfusion
imbalance
Efficiency of Pulmonary Gas Exchange is lower.
Normal ventilation-perfusion
regulation
Pulmonary Gas Exchange is maintained by Regulation.
Shunts
• “Shunt” is a term used to describe a condition in which VA
/Q is zero due to no ventilation.
• Anatomical shunts result from blood vessels that do not
flow past alveoli (arterial blood perfusing the bronchi goes
directly into pulmonary veins without passing through the
lungs).
• Alveolar shunts result from alveoli that are not ventilated
or are not capable of exchanging gas.
• A physiological shunt is the sum of anatomical and
alveolar shunts.
• The greater the magnitude of the physiological shunt, the
lower the Po2 and the higher the Pco2 of arterial blood.
• The greater the magnitude of the physiological shunt, the
greater the alveolar-arterial oxygen difference.
Shunt and dead space are related
and represent the limits of VA/Q
• Shunt refer to conditions where VA/Q is zero
because of no ventilation, whereas dead space
refers to conditions where VA/Q is infinite
because of no blood flow.
• Both shunts and dead space have anatomical
and alveolar components.
• Shunts and dead space represent the limits of
VA/Q.
Shunt and dead space are related
and represent the limits of VA/Q
In the presence of a shunt,
alveolar air has the gas
composition of venous blood
(pco2 =46mm Hg; po2 =40mm
Hg) because it has not been
altered by exchange with
outside air. At the other
extreme, dead space, alveolar
air has the gas composition of
inspired air (po2 =150mm Hg;
pco2 =0) because it has not
been altered by exchange with
venous blood. Between these
extremes where these is some
degree of ventilation and
perfusion, alveolar air and,
therefore, pulmonary blood will
have a po2 and a pco2 between
these limits.
VA /Q =0
(Shunt)
VA /Q =Normal
Pc
o250
m
m
H
g
VA /Q =Infinity
(Dead Space)
0
0
50
100
Po2 mmHg
150
Mismatches in the ventilation to perfusion ratio (VA/Q) affect the Po2 and Pco2 in
alveolar air. In ventilated alveoli, as the level of perfusion decreases to zero (dead
space), the Po2 increases and the Pco2 decreases. In perfused alveoli, as ventilation
decreases to zero (shunt), the Po2 decreases and the Pco2 increases.
Normal alveolar ventilation and
blood perfusion matching each
other for gas exchange
Ventilation/perfusion ratio is about 0.84
Relationship between alveolar
ventilation and alveolar partial pressure
Abnormal alveolar ventilation for
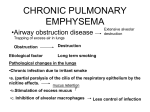
gas exchange
Emphysema results in increased shunt.
Body has anoxia.
Abnormal alveolar ventilation for
gas exchange
Fibrotic lung disease (纤维化肺疾病) results in
increased shunt.
Body has anoxia.
Abnormal alveolar ventilation for
gas exchange
Pulmonary edema results in increased shunt.
Body has anoxia.
Abnormal alveolar ventilation for
gas exchange
Asthma results in increased shunt.
Body has anoxia.
3. Tissue gas exchange
Definition *: gas exchange between capillary blood flow and
histiocytes.
Influencing factor of tissue exchange
– Distance between histiocytes and blood capillary
– Tissues metabolic level
Metabolic level ↑→O2 use↑, CO2 production↑→local PO2↓,
PCO2↑→big difference with blood gas partial pressure→ gas
exchange in tissue↑.
Local metabolites↑→capillary opening amount↑→gas
exchange in tissue↑.
– Blood flow velocity of blood capillary
Fast, there is not sufficient time to make gas exchange;
Slow, transport of O2 and CO2 within unit time is decreased.
Tissue gas exchange
III. Gas transport in the Blood
1. Transport forms of oxygen and carbon dioxide in the blood
Transport forms: physical dissolution (elementary
substance O2, CO2) and chemical constitution (HbO2,
HCO-3);
• Systemic arterial and pulmonary venous blood are
high in oxygen and low in carbon dioxide;
• Systemic venous and pulmonary arterial blood are
high in carbon dioxide and low in oxygen.
Gas composition of arterial
and venous blood
O2 exchange between the alveoli and
blood and O2 transport
Movement of carbon dioxide and
oxygen between the alveolar air
and the blood and between the
blood and peripheral tissue
depends upon concentration
gradients for these gases. As can
be seen in this figure, the
gradients favor the movement of
oxygen from alveolar air to the
tissue and movement of carbon
dioxide from the tissue to alveolar
air.
Venous blood
Po2=40 mmHg
Pco2=46 mmHg
O2 exchange between the blood and tissue
cells and O2 transport
Movement of carbon dioxide
and oxygen between the
alveolar air and the blood and
between the blood and
peripheral tissue depends upon
concentration gradients for
these gases. As can be seen in
this figure, the gradients favor
the movement of oxygen from
alveolar air to the tissue and
movement of carbon dioxide
from the tissue to alveolar air.
CO2 exchange between the tissue cells and
blood and CO2 transport
Movement of carbon dioxide
and oxygen between the
alveolar air and the blood and
between the blood and
peripheral tissue depends upon
concentration gradients for
these gases. As can be seen in
this figure, the gradients favor
the movement of oxygen from
alveolar air to the tissue and
movement of carbon dioxide
from the tissue to alveolar air.
CO2 exchange between the blood and alveoli and
CO2 transport
Movement of carbon dioxide
and oxygen between the
alveolar air and the blood and
between the blood and
peripheral tissue depends upon
concentration gradients for
these gases. As can be seen in
this figure, the gradients favor
the movement of oxygen from
alveolar air to the tissue and
movement of carbon dioxide
from the tissue to alveolar air.
2. Oxygen transport in the blood
• Oxygen is carried in two forms: dissolved (1.5%) and bound
to hemoglobin (98.5%).
• Dissolved oxygen is inadequate to meet the body’s needs.
• Hemoglobin greatly increases the blood’s oxygen-carrying
capacity.
• Three terms describe the amount of oxygen in the blood:
capacity, saturation, content.
• Oxygen binding to hemoglobin is influenced by pH, carbon
dioxide, 2,3-diphosphoglycerate (2,3-DPG), and
temperature.
• Carbon monoxide decreases the blood’s oxygen content
and capacity.
Oxygen transport in the blood
Physical dissolved form is secondary (1.5%).
Oxygen transport in the blood
Chemical combined form is dominating (98.5%).
Oxygen transport in the blood
under the low Po2 in the blood
Structure of Hemoglobin
Fe2+
Hemoglobin (Hb) enables the blood
to carry large quantities of oxygen.
Hb consists of a heme, an ironprophyrin, bound to a globin
molecule, a large polypeptide
chain. Four heme-globin
complexes combine to form the
whole Hb molecule. There are 4
different globin molecules that vary
slightly in amino acid composition
and are designated alpha, beta,
gamma, and delta chains. The most
common form is Hb A, which
consists of 2 alpha and 2 beta
chains. Oxygen binds to the iron
atoms in Hb and because the
molecule contains 4 iron atoms, 4
oxygen molecules can be bound.
(1) Characteristic of Hb combining with O2
Reaction: fast, reversible, no enzyme catalysis, influenced
by PO2.
After Fe ion combined with O2, Fe ion is still Fe2+, so it is
oxygenation rather than oxidization;
Absorbing ability different made by response of different
Hb to various spectrum.
Ability of HbO2 absorbing shortwave spectrum (e.g.
blue light) is stronger;
Ability of HHb absorbing long wave spectrum (e.g. red
light) is stronger;
Blood color is related to Hb content, quality,
arterial blood: bright red; venous blood: prunosus
Cyanosis : when reduced Hb (HHb) in the body
surface capillary bed blood is more than 5 g /100 ml,
skin and mucosa display violaceous color.
O2+ Hb
HbO2 **
PO2
PO2
Three terms are used to describe the amount of
oxygen in the blood
• Oxygen content refers to the total amount of oxygen in the blood,
that is, the sum of the amount dissolved plus the amount bound to
hemoglobin (Hb).
• Oxygen capacity is the maximum amount of oxygen that can
combine with Hb. It is determined by exposing blood to a very
high Po2 and calculating the amount bound to Hb after subtracting
the amount dissolved. The oxygen capacity is determined by the
amount of Hb in the blood and by the ability of Hb to bind oxygen.
• Oxygen saturation * is the proportion of the total number of
oxygen binding sites that are occupied. It is determined by the Po
and the ability of Hb to bind oxygen, but not by the amount of Hb
present in the blood.
Oxygen saturation = Oxygen content / Oxygen capacity ×100%
(2) Oxygen dissociation curve or named O2-Hb
binding curve
0 20
Po2 (mm Hg)
The curve describes relationship between the Po2
and the hemoglobin oxygen saturation **
He
m
og
lo
bi
n
O2
Sa
tu
rat
io
n
(%
)
Oxygen dissociation curve or
named O2-Hb binding curve
100
20
Arterial Po2
Venous Po2
10
%
Hemo
globin
Satur
ation
Oxygen Combined With Hb
Oxygen Dissolved In Blood
0
0
0
50
Oxyge
n
Conte
nt
(mL/1
00 mL
blood)
50
100
Po2 (mm Hg)
Oxygen is present in the blood in a dissolved form and is bound to
Hb. The partial pressure of oxygen determines how much is in each
form. Much more oxygen is bound to Hb at any partial pressure
than is dissolved.
Oxygen dissociation curve or named O2-Hb
binding curve
Total Blood
Oxygen Content
Oxygen Combined With Hb
Oxygen Dissolved In Blood
Oxygen Dissociation Curve
Oxygen dissociation curve
Notice that at normal arterial Po2 (100 mm
Hg), Hb is over 95% saturated and that
even at normal venous Po2 (40 mm Hg) it
is still 75% saturated. Because of Hb, 100
mL of blood contain approximately 19 mL
of O2 at arterial Po2 and about 14 mL at
venous Po2 . This means that 5 mL of O2
were delivered to the tissue by 100 mL of
blood because of Hb, more than 10 times
the amount present in the dissolved form
(0.3 mL).
Shape like Reversed “S” Style
Oxygen dissociation curve
Embryo and adult have some different percent O2
saturation of hemoglobin
Reason Why?
(3) Influencing factors of oxygen dissociation curve
**
Effect of pH on oxygen dissociation curve
pH decrease results in
curve right shift which
means that Hb releases
more O2 to tissue cells
for use.
Bohr effect *:pH↓ or PCO2↑ increase Hb releasing O2
(affinity↓)
Effect of Pco2 on oxygen dissociation curve
Pco2 increase results in
curve right shift which
means that Hb releases
more O2 to tissue cells for
use.
Effect of temperature on oxygen
dissociation curve
Temperature increase
results in curve right
shift which means that
Hb releases more O2 to
tissue cells for use.
Effect of 2,3-DPG on oxygen dissociation
curve
2,3-DPG increase results in curve
right shift which means that Hb
releases more O2 to tissue cells
for use.
Effects of various factors on oxygen dissociation curve
Al
ve
ol
ar
Ve
nti
lat
io
n
(B
as
ic
Ra
te
is
1)
pH
Al
ve
ol
ar
Ve
nti
lat
io
n
(B
as
ic
Ra
te
is
1)
Pco2 30 35
Po2 140 120
40
100
45
80
50
60
55
40
60
20
Normal
65 (mm Hg)
0 (mm Hg)
6.9
Reaction of changing in one factor with
other factors constant.
Reaction of changing in one factor with
other factors changeable as well.
Carbon monoxide decreases the blood’s
oxygen content and capacity
Inhalation of carbon monoxide (CO) has several effects on
oxygen transport by the blood. The affinity of CO for Hb is
240 times that for oxygen, so very small amounts of CO will
occupy a large number of the oxygen binding sites. This
effectively reduces the oxygen capacity of Hb. Because of
this, Hb becomes saturated with oxygen at very low Po2
values, values that are less than those in venous blood. This
means that little if any oxygen will be released for tissue use.
The net effect is that at normal alveolar Po2 oxygen content
and capacity of blood is greatly reduced even though Hb is
saturated and the amount of dissolved oxygen is normal.
Different ways influence total arterial O2
content (Summary)
3. Carbon dioxide transport
by blood
• Carbon dioxide is transported in the blood in
three forms: dissolved, as bicarbonate (main
form), and bound to hemoglobin.
• Blood contains more carbon dioxide than it
does oxygen.
• Carbon dioxide binding to hemoglobin is
affected by Po2.
(1)Carbon dioxide transport by
bicarbonate ion in the blood*
Tissue Fluid
blood plasma
Metabolism
(88%)
RBC
CA: carbonic anhydrase
Carbon dioxide transport by
bicarbonate ion in the blood
(2)Comparison of dissociation curve
of CO2 and O2 *
Carbon Dioxide
60
Venous Pco2
Oxygen
Arterial Pco2
30
0
C
o2
or
O2
C
on
te
nt
(m
L/
10
0
m
L
bl
oo
d)
0
50
Pco2 or Po2 (mm Hg)
100
The blood carries much more carbon dioxide than oxygen
(3) Effect of O2 On CO2 dissociation
curve *
Bloo
d
carb
on
dioxi
de
Cont
ent
(Volu
me%
)
Pco2 (kPa)
Haldane effect : O2 combining with Hb induces CO2 release,
and HHb easily combines with CO2.
Effect of O2 On CO2 dissociation curve
(4)Interrelationship between O2 and CO2 in
Transport by Blood **
Just as CO2 alters O2 binding to Hb (Bohr effect), O2 alters
CO2 binding (Haldane effect). As the Po2 increases, less CO2
can bind to Hb. This interrelationship between O2 and CO2
binding to Hb facilitates gas exchange with Hb both in the
lungs and in the tissue. In the lungs, Po2 is high, which
reduces CO2 binding to Hb, facilitating release into alveolar air.
In the tissue Po2 is low, which increases CO2 binding to Hb,
facilitating its removal from the tissue. As described in the
previous section (Oxygen Transport in the blood) changes in
Pco2 facilitate oxygen binding to Hb in an appropriate manner
in tissue and lung.
IV. Respiratory Regulation
1. Respiratory centers and formation of respiratory rhythm
Control of breathing rhythm
• Medulla and pons (bridge) form the integration center and
contain neural elements that define the basic breathing
rhythm (Using transecting method).
• In medulla, ventral respiratory group and the dorsal
respiratory group that are responsible for establishing this
rhythm.
• The basic rhythm is modulated by higher brain centers and
by receptors located in the chest wall and lungs.
• Primary efferent output (depth and frequency of respiration )
is via the phrenic nerve to the diaphragm.
• Motor nerves that exit the spinal cord at several levels in the
thorax innervate intercostal muscles. These muscles are
activated when large volumes of air must be moved.
• Reflex of cough and sneeze is useful for defence in
respiratory system.
Control of breathing rhythm
Rhythmicity unrhythmicity
The fourth
ventricle
midbrain
Intact vagus nerve
Cut vagus nerve off
Different respiratory centers in brain stem regulate
breathing rhythm
PC: Respiratory regulatory center; Böt C: Böt’s complex; VRG: ventral
respiratory group; DRG: dorsal respiratory group; PBKF: Kölliker-FuseNucleus; A/B/C/D: Different transect; NTS: nucleus tractus solitarius
Control of breathing rhythm
2. Reflex regulation of respiration
(1) Chemoreceptive reflex
Ventilation influenced by Po2 ,Pco2 , and pH ( [H+] )**
• Two groups of chemoreceptors, medullary and
peripheral, send afferent information to the medulla
and influence the depth and rate of respiration.
• Medullary chemoreceptors are sensitive to pH and
increase ventilation when pH falls ( [H+]↑ ).
• Peripheral chemoreceptors are sensitive to pH, Po2
, and Pco2 with Pco2 being most effective.
• Sensitivity of the peripheral chemoreceptors is
influenced by pH,. Po2 , and Pco2.
① Medullary chemoreceptors
Chemical sensitive Area
Chemical sensitive
Area influencing
respiration
Nuclei related
respiration
The medullary chemoreceptors or central chemoreceptors are sensitive to
pH. Since the blood-brain barrier is impermeable to H+, the medullary
chemoreceptors do not directly sense the pH of the blood. However, CO2
can diffuse from the blood into the cerebral spinal fluid where it is
converted to H+ and HCO3-.The hydrogen ions thus formed stimulate the
medullary chemoreceptors.
② Effects of plasma Pco2 on ventilation*
③ Effects of plasma Pco2 and
On ventilation *
+
H
④ Effects of plasma Po2 on ventilation*
2
he peripheral chemoreceptors: carotid
and aortic bodies
Ventilation↑
Notice, Serious
anoxemia (hypoxia)
will directly inhibit
respiration
⑤ Ventilation influenced by Po2 ,Pco2, and pH
( [H+] ) **
The relative levels of pH, Po2 , and Pco2 influence the sensitivity
of peripheral chemoreceptors to pH, Po2, or Pco2. When the Po2 or
pH is low, the carotid body sensitivity to Pco2 is increased.
Similarly, the carotid body sensitivity to oxygen is increased if the
Pco2 is elevated. However, under some circumstances these
interactions can be antagonistic. At high altitude Po2 falls because
of the fall in atmospheric pressure. This stimulates ventilation but
also reduces arterial Pco2 as carbon dioxide is blown off. The fall in
Pco2 reduces the primary drive for ventilation and the sensitivity of
the carotid body chemoreceptors to arterial oxygen. This leads to a
further fall in arterial Po2 , enhancing oxygen’s stimulatory effect on
ventilation. Ultimately, a steady state is reached between the
stimulatory response to hypoxia (low oxygen) and the inhibitory
effect of hypocapnia (low CO2).
(2) Other respiratory reflexes
Pulmonary stretch reflex : found in 1868 by Breuer and
Hering.
Definition*: pulmonary inflation or expansion result in
inspiration inhibition turning into expiration and pulmonary
collapse induces inspiration excitation (Hering-Breuer
reflex).
Pulmonary deflation reflex
Proprioceptive reflex of respiratory muscles
Defensive respiratory reflexes: cough reflex and sneeze
reflex.
Connect with clinic · · · · · ·
Effects of different factors
on respiration (Summary)
Changes in Ventilation
Pathological respiratory patterns
Coma
Respiratory
Depth
Cheyne-stokes’
breathing
Respiratory Center
Respiratory Center
Excitation
Pulmonary Blood
Encephalic high pressure
Biot’s breathing
Pathological periodical respiratory
pattern
V. Role of the lungs in regulation
of acid-base balance
Ventilatory Response to Acid-Base Changes
• Because the CO2-bicarbonate buffer system
plays a significant role in regulating pH, the
lungs can alter arterial pH by changing arterial
Pco2.
• Ventilation is increased in response to metabolic
acidemia.
• Ventilation is decreased in response to
metabolic alkalemia.
Role of the lungs in regulation
of acid-base balance
•The CO2-bicarbonate buffer system is the major way in which the
body maintains arterial pH because the lungs regulate the CO2
level of the blood and the kidneys regulate the amount of
bicarbonate (chapter4).
•CO2undergoes the following reaction in blood:
CO2 + H2O
H2CO3
H + + HCO3-
pH=6.1+log ( [HCO3-] / Pco2) {deriving from the HendersonHasselbalch equation}
•Normal blood values can be substituted for the various
parameters. To convert the units of mm Hg for Pco2 to mEq/L, Pco2
is multiplied by 0.03.
7.4=6.1+log [24mEq/L/(0.03×40 mm Hg)]=6.1+log 20/1
This relationship shows that as long as the ratio of bicarbonate to
CO2 is 20:1,pH will be 7.4. The body adjusts the amounts of these
two substances in order to maintain a normal pH. The lungs
regulate the amount of CO2.
Role of the lungs in regulation
of acid-base balance
• Arterial H+ concentration can change for a variety of
reasons. If the cause does not involve the lungs, it is said to
be of metabolic origin. It is called metabolic acidosis if the
pH decreases and metabolic alkalosis if the pH increases. If
the lungs are the cause of the acid-base disturbance, the
processes are called respiratory acidosis and respiratory
alkalosis.
• An elevation in arterial H+ concentration and Pco2 will
stimulate ventilation. The increase in ventilation will lower
the Pco2 driving (reaction 1) further to the left helping to
lower the H+ concentration. In addition, the kidneys will
generate bicarbonate and secrete H+.
• An decrease in arterial H+ concentration and Pco2 will
reduce ventilation allowing Pco2 to accumulate. This will
generate additional H+ and help to return the pH to normal.
Altered ventilation causes
acid-base changes
• CO2 + H2O H2CO3 H + + HCO3-
• An inability of the lungs to remove CO2
results in respiratory acidemia.
• Inappropriate removal of CO2 by the lungs
results in respiratory alkalemia.
Consideration after class
1. Please describe characteristic , forming
mechanism and physiological meaning of
intrathoracic pressure.
2. What are the influencing factors of the gas
exchange?
3. Please describe concept , characteristic and
influencing factors about oxygen dissociation curve.
4. How do changes in Po2 ,Pco2 , and pH ( [H+] )
influence the respiratory movement ?