* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
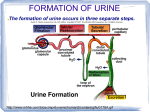
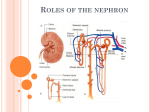
Physiology 441 The Renal System, Chp. 14 Text: Human Physiology (Sherwood), 6th Ed. Julie Balch Samora, MPA, MPH [email protected] 293-3412, Room 3145 Review • How is glucose transported? • What is the renal threshold? • Do we see this for passive transport? • Do the kidneys regulate glucose/ phosphate plasma concentration? Review cont… • What is the vascular sequence in the nephron? • What is the tubular sequence? Review cont… • What happens if ↓ NaCl, ↓ ECF volume, and ↓ arterial blood pressure? Tubular Secretion • Additional mechanism to eliminate certain substances • Secretion of H+, NH3, K+, organic anions and cations • Acid and ammonia secretion imp. in acidbase balance • Ammonia is secreted during acidosis in order to buffer the secreted H+ H+ and NH3 secretion • Hydrogen and ammonia secretion aid with acid-base balance • H+ secretion provides a highly discriminating mechanism for varying the amt of H+ excreted in the urine, depending on the acidity of the body fluids • NH3 is secreted in pronounced acidosis to buffer the H+ secreted into the urine K+ Secretion • K+ is actively reabsorbed in the proximal tubule, but is also actively secreted in the distal tubule. • Allows fine degree of control over plasma K+ concentration • Secretion of K+ is variable and subject to aldosterone control • Even slight fluctuations in ECF [K+] can alter nerve and muscle excitability Organic anion and cation secretion • The proximal tubule contains 2 different carriers for secreting organic ions • These systems aid in secreting foreign organic substances • The liver helps this process by converting many foreign substances into anionic metabolites Process of Secretion Renal Processes 1 Urine excretion • The final quantity of urine formed averages about 1ml/min • This urine contains a high conc. of waste products & low or no conc. of substances needed by the body • Minimum volume of urine to eliminate wastes is 500 ml/day Plasma Clearance • The amount of plasma “cleared” of a substance • Plasma clearance for a substance that is FILTERED, but not REABSORBED or SECRETED == GFR == 125ml/min • EXAMPLE = INULIN INULIN- Filtered, NOT reabsorbed, NOT secreted Renal Processes 2 Plasma Clearance • Plasma clearance for a substance that is FILTERED AND REABSORBED, but NOT SECRETED < GFR • EXAMPLE = GLUCOSE, UREA • Clearance rate can be anywhere from 0 up to normal clearance (125 ml/min) depending on amount reabsorbed Glucose/urea- Filtered and reabsorbed, NOT secreted Renal Processes 2 Plasma Clearance • Plasma clearance for a substance that is FILTERED AND SECRETED > GFR • EXAMPLE = PAH (Para-aminohippuric acid) • Not only is the plasma that is filtered cleared of that substance, but additional amt cleared from plasma which was not filtered • Plasma clearance rate for PAH=RENAL PLASMA FLOW Plasma clearance rate for PAH = Renal Plasma Flow Renal Processes 2 Plasma Clearance Questions • What is the PC for a substance that is FILTERED AND REABSORBED, but NOT SECRETED? • What is the PC for a substance that is FILTERED AND SECRETED? • What is the PC for a substance that is FILTERED, but not REABSORBED or SECRETED? Osmolarity • Measure of the concentration of individual solute particles dissolved in fluid • The higher the osmolarity, the higher the concentration of solutes • WATER moves by osmosis from an area of lower osmolarity (higher water conc) to an area of higher osmolarity (lower water conc) until the concentration difference is eliminated Osmolarity • Isotonic- solution is the same conc. as normal body fluids (300 milliosmols/L) • Hypotonic- solution is more dilute than normal body fluids (< 300 milliosmols/L) • Hypertonic- solution is more concentrated than normal body fluids (> 300 milliosmols/L) Question • How can the kidneys put out a concentrated urine when the body is dehydrated? • How can the kidneys excrete a dilute urine when the body is overhydrated? Proximal tubule Distal tubule Distal tubule Glomerulus Bowman’s capsule Proximal tubule Cortex Medulla Collecting duct Descending limb of loop of Henle Loop of Henle Other nephrons emptying into the same collecting duct Vasa recta Ascending limb of loop of Henle To renal pelvis Fig. 14-5, p. 505 Countercurrent System • There is a vertical osmotic gradient in the interstitial fluid of the medulla • This gradient, with the help of ADH (vasopressin) allows the kidney to vary the concentration of the urine depending on the body’s needs • Countercurrent multiplication- loops of Henle and Juxtamedullary nephrons • Countercurrent exchange- vasa recta of the juxtamedullary nephrons Countercurrent System • At the end of the proximal tubule and beginning the loop of Henle, the filtrate is isotonic (300 mosm/L) • Na+ is actively reabsorbed against its concentration gradient in the proximal tubule, creating an osmotic gradient, pulling water across to maintain osmotic equilibrium Countercurrent Multiplication • The loops of Henle of the juxtamedullary nephrons are responsible for establishing the concentration gradient in the renal medulla • Desc. limb is freely permeable to H2O, but NOT NaCl – so H2O goes into IF • The ascending limb actively transports out NaCl • Asc. Limb IMPERMEABLE to water Medullary vertical osmotic gradient • There is a countercurrent flow produced by the close proximity of the two limbs • The ascending limb produces an interstitial fluid that becomes hypertonic to the ascending limb. • This interstitial fluid faces against the flow of fluid (countercurrent) in the descending limb, attracting the water by osmosis for reabsorption Countercurrent Multiplication • The fluid in the descending limb becomes progressively more concentrated • At the bottom, its concentration is 1200 mosm/L!! • As the asc. Limb is impermeable to water, when NaCl is pumped out, water remains, causing the remaining liquid in the loop to become hypotonic (100 mosm/L) Countercurrent Multiplication • Therefore, a vertical osmotic gradient varying from 300 to 1200 mosm/L exists in the medulla • The filtrate as it leaves the loop of Henle to enter the distal tubule is HYPOTONIC • Gets its name due to the flow in opposing directions through the two limbs and the stepwise multiplication of concentration due to transport and permeabilities Countercurrent Countercurrent exchange • The vasa recta are responsible for preserving the concentration gradient in the medulla that has been established by the loop of Henle • The blood in the vasa recta follows the same course as the loops of Henle of the juxtamedullary nephrons. • The vasa recta are exposed to the same gradient in the IF-blood concentration is similar Countercurrent exchange • This process is a passive, osmotic exchange b/t the IF and two closely opposed vessels with fluid flowing in opposite directions Importance of the Vertical Gradient • The collecting ducts are normally impermeable to water • However, if the body needs to conserve H2O, ADH (vasopressin) is secreted • ADH increases the permeability of the distal tubules and collecting tubules to H2O ADH- Saving Water • Due to the vertical osmotic gradient, the tubular fluid loses more water into the IF, which eventually enters the plasma • At the end of the collecting tubule, it is possible to have urine concentrated to 1200 mosm/L (very small volume excreted) Role of ADH • ADH is produced in the hypothalamus and stored in the posterior pituitary. The release of this substance signals the distal tubule and collecting duct, facilitating the reabsorption of water. • ADH works on tubule cells through a cyclic AMP mechanism. • During a water deficit, the secretion of ADH increases. This increases water reabsorption. • During an excess of water, the secretion of ADH decreases. Less water is reabsorbed. More is eliminated. Elimination of excess H2O • If overhydrated, no ADH released, therefore distal tubules and collecting ducts remain impermeable to H2O • Even though water wants to leave (due to osmotic forces), it cannot • Therefore, a large volume of dilute urine is excreted Urine Concentration Summary • The medullary vertical osmotic gradient and ADH allow the kidney to excrete urine of varying concentrations • Without this osmotic gradient, we could not produce a concentrated urine, and would be unable to conserve water • We would likewise be unable to rid the body of excess water w/o this system