* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Varicella Infection
Traveler's diarrhea wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Tuberculosis wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Toxoplasmosis wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Henipavirus wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Chagas disease wikipedia , lookup
Onchocerciasis wikipedia , lookup
Herpes simplex wikipedia , lookup
Sarcocystis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
West Nile fever wikipedia , lookup
Leptospirosis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Trichinosis wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Antiviral drug wikipedia , lookup
Schistosomiasis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
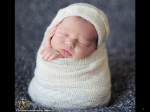
Neonatal infection wikipedia , lookup
Systemic Infections in Pregnancy Dr. Jasmin Sapanghila-Tamon • • • • • Varicella Rubella Hepatitis B Syphilis HIV Varicella Infection Varicella Infection • DNA Herpesvirus • Primary infection causes varicella (chickenpox) • Recurrent infection causes herpes zoster (shingles) Pathogenesis and Clinical Features • Incubation period 14-16 days • Mild prodrome for 1-2 days • Maculopapular rash generally appears first on the head; most concentrated on trunk Mode of Transmission • Direct Contact – with patient who sheds the virus from vesicles • Indirect Contact – through articles fresh soiled by discharges of infected persons • Airborne – or spread by droplet infection Period of Communicability: • The patient is contagious about a day before the eruption of rashes and continuous to be so up to the 5th or 6th day after the last scab formation or until all vesicles have become encrusted. Diagnostic Test: • Determination of V-Z virus though Complement Fixation Test • Determination of V-Z virus through Electron Microscopic examination of vesicular fluid Complications: • Secondary infection of the lesions – furuncles, cellulites, skin abscess, erysipelas • Meningoencephalitis • Pneumonia • Sepsis Groups at Increased Risk of Complications of Varicella • Normal adults • Immunocompromised persons • Newborns with maternal rash onset within 5 days before to 48 hours after delivery Is risk of severe chickenpox increased in pregnancy? • No definite evidence that varicella is more likely to be fatal in pregnant women than in non pregnant adult Hermmann KL. Clin Obstet Gynecol 1982;25:605-609. Fetal Effects of Varicella • No infection • Infection – Congenital Varicella syndrome – Neonatal varicella infection – Infant herpes zoster Transmission to the Fetus • • • • <13 weeks AOG: 0.4% 13-20 weeks AOG: 2% >20 weeks AOG: 0 Within 5 days before or after delivery: 10-20% neonatal varicella infection Congenital Varicella syndrome • Damage to sensory nerves • Damage to optic nerve and lens vesicles • Damage to cervical and lumbosacral cord • Damage to brain Diagnosis of Congenital varicella syndrome • Cordocentesis to estimate fetal VZV-specific IgM ab • Chorionic villus sampling to detect VZV DNA sequence using PCR • Serum AFP • UTZ Management of the mother – Post exposure • Check VZV immunity • Consider – Prevention of chickenpox – VZIG – Treatment of chickenpox with antiviral – Counseling of mother and close fetal monitoring Exposure Criteria for Use of VZIG: 1. Continuous household contact 2. Playmate/officemate contact >1hour indoors 3. Hospital contact – adjacent bed or infected staff member 4. Newborn of infected mother – from 5days before to 2days after delivery AND 5. Time lapse from exposure is less than 96 hours Varicella zoster Immunoglobulin (VZIG) – Prevent congenital varicella syndrome ? • No definite evidence • No congenital varicella syndrome among 97 pregnant women who received VZIG, but not sufficient power to reach significance • Documented cases of congenital varicella syndrome despite VZIG Enders et al Lancet 1994: 343; 1548-1551. If patient is not pregnant but has a significant exposure to varicella – give vaccine within 120 hours of exposure – 70-100% effective if given within 72 hours of exposure – Not effective if given beyond 5 days of exposure but will produce immunity Treatment • Generally, there is no need to treat uncomplicated varicella since this is almost always a self-limiting disease. • Only in an immunocompromised host or when complications such as pneumonitis or encephalitis occur should antiviral therapy be considered. Treatment • For women infected with varicella – Give acyclovir 800mg 5 times a day for 5-7 days – Not recommended for routine use among otherwise healthy infants and children with varicella Summary • Chickenpox may be serious for pregnant women and fetus • Increasing numbers of seronegative women could result in increase chickenpox in pregnancy • Vaccine strategy should aim to protect all non immune adults especially women of reproductive age • Congenital varicella syndrome may be a rare occurrence, but the risk to the fetus is so high that prevention, post exposure prophylaxis and treatment, once infected, should always be an option. Rubella Rubella • Highly communicable disease • Infected person may shed the virus in the upper respiratory tract from 1 week before to 5-7 days after the onset of rash • Incubation Period: 14 days (12-23 days) Rubella Low grade fever and mild upper respiratory tract infection Maculopapular rash on the face and neck, trunk and proximal extremities Development of adenopathy Rash fades within 1-3 days of onset • Incubation Period: 12-23 days • 20%-50% of infections may be asymptomatic • Viremia precedes clinical signs by 1 week, and adults are infectious during viremia until 57 days of the rash Rubella • Risk of congenital defects: – </=12 weeks AOG: 80% – 13-14 weeks AOG: 54% – 15-28 weeks AOG: 25% Congenital Rubella Syndrome • • • • • • • Eye defects Heart disease – PDA Sensorineural deafness CNS defects Pigmentary retinopathy Purpura Hepatosplenomegaly and jaundice • Radiolucent bone disease Rubella in Pregnancy • There is no treatment to ameliorate maternal disease or reduce the risk to the fetus when maternal infection is present • Prevention of fetal infection requires prevention of maternal infection through widespread vaccination programs WHO Recommendation • All countries to assess their rubella status and introduce immunization and surveillance, if appropriate Rubella • Do serum rubella IgG on all pregnant patients • If patient is seronegative to rubella, give rubella vaccine postpartum Counseling and Management • Pregnant women with confirmed rubella infection must have proper counseling about the risks and types of congenital anomalies Counseling and Management • Routine use of rubella Ig is not recommended for postexposure prophylaxis since this does not prevent infection nor viremia. Advisory Committee on CDC, Aug, 2006 Rubella Vaccine • Long term protection (about 15 years) from vaccination is about 98 to 99%; thus about 2% of vaccinated women may be negative when tested. • Ideally all vaccinated women should have their serological status determined before becoming pregnant. Rubella Screening • MMR should not be given to adolescents who are known to be pregnant or to adolescents who are considering becoming pregnant within 3 months of vaccination. Recommendations • Routine screening for rubella susceptibility by history of vaccination or by serology is recommended for all women of childbearing age at their first clinical encounter. • Susceptible non pregnant women should be offered rubella vaccination; susceptible pregnant women should be vaccinated immediately after delivery. • An equally acceptable alternative for non pregnant women of childbearing age is to offer vaccination against rubella without screening. Hepatitis B • Caused by DNA hepadnavirus • Incubation period: 6 weeks to 6 months • Highest concentration in the blood, lower concentrations in other body fluids • Transmitted by percutaneous or mucous membrane exposure to infectious blood or body fluids that contain blood Risk Factors 1. Persons of Asian, Alaskan, Sub-Saharan African descent 2. History of IV drug use 3. History of STD 4. Multiple sexual partners 5. Worker or patient in a hemodialysis unit 6. Health care or public safety worker Risk Factors 7. Household contact with Hepatitis B carrier 8. Sexual contact with Hepatitis B carrier 9. Worker or residence in an instiution for the developmentally disabled 10. History of blood transfusion 11. Delivery to a carrier mother Hepatitis B • Risk for chronic infection is inversely related to age at infection • In adults, approximately half of newly acquired HBV infections are symptomatic, 1% result in acute liver failure • 90% of infants and 30% of children aged <5 years become chronically infected Diagnosis HBs Ag Total anti HBc IgM anti HBc Anti HBs Interpretation - - - - Never infected + - - - Early acute infection; after vaccination (18 days) + + + - Acute infection - + + - Acute resolving infection - + - + Recovered from previous infection and immune + + - - Chronic infection - - - + Immune in conc >/= 10mIU/mL Pregnancy and HBV Infection • Transmission of HBV from mother to infant (predominantly intrapartum) is one of the most efficient modes of HBV spread • 4 Routes 1. Transplacental 2. Intrapartum 3. Post-partum 4. Breast milk Pregnancy and HBV Infection Perinatal Transmission Rates of Hepatitis B Virus Clinical Status Transmission Rate HBsAg +, HBeAg - 10-20% HBsAg +, HBeAg + 90% Acute Hepatitis B first trimester 10% Acute Hepatitis B third trimester 80-90% Hepatitis B TREATMENT Acute Hepatitis B • primarily supportive on an ambulatory basis with bed rest • High protein diet • Avoidance of hepatotoxic drugs Treatment of Hepatitis B Chronic Hepatitis B Goals of therapy 1. Suppression or complete resolution of chronic active hepatitis 2. Halting progression of liver disease 3. Converting patients to a noninfectious state Prevention • Hepatitis B immune globulin (HBIG) – 0.06mL/kg • Hepatitis B vaccine • Periodic testing to determine ab levels in immunocompetent persons is not necessary, and booster doses of vaccine are not recommended Hepatitis B CDC National strategy to eliminate transmision of HBV 1. Prevention of perinatal infection 2. Routine infant vaccination 3. Vaccination of previously unvaccinated children and adolescents through age 18 4. Vaccination of previously unvaccinated adults at increased risk for infection Hepatitis B Post-Exposure Prophylaxis Percutaneous or mucosal exposure to HbsAg (+) blood or body fluids that contain blood Sexual or needle sharing contact of an HbsAg (+) person Administer Hepatitis B vaccine and Hepatitis B Ig Victim of sexual assault/abuse of a perpetrator who is HbsAg (+) Administer Hepatitis B vaccine and Hepatitis B Ig Administer Hepatitis B vaccine and Hepatitis B Ig Hepatitis B Post-Exposure Prophylaxis Victim of sexual assault/abuse of a perpetrator with unknown HbsAg status Administer Hepatitis B vaccine Percutaneous or mucosal Administer Hepatitis exposure to HbsAg (+) blood or B vaccine body fluids that contain blood from a source with unknown HbsAg status Management of HbsAg (+) Persons • Persons with chronic HBV infection should be referred for evaluation of CLD • Household, sexual and needle-stick sharing contacts of chronically infected persons should be identified • Sexual partners should be counseled to use methods to protect themselves from sexual exposure to infectious body fluids • Protect liver from further harm Syphilis Syphilis • Caused by the spirochete Treponema pallidum • Acquired by sexual contact • 3-10% contract the disease from a single sexual encounter with an infected partner Stages 1. Primary – genital &extragenital 2. Secondary – bacteremia involving all major organs 3. Latent – lack of clinically apparent disease 4. Tertiary – 1-20 years after the disease has become latent, progressive damage involving CV, muskuloskeletal and CNS Syphilis • Primary Syphilis – Chancre – hallmark lesion • Typically single, painless ulcer with raised rounded borders and a “clean” indurated base arise at the site of entry of T.pallidun into the body, inapparent breaks in the host’s skin during intercourse Secondary syphilis Diagnosis • Dark field microscopy of secretions from chancre demonstrate the spirochetes Diagnosis • Non Treponemal Tests: – VDRL, RPR - screening tests - correlates with disease activity - use to assess treatment response Diagnosis • Treponemal Tests: – FTA-ABS, TPHA - confirmatory test - remains positive for the remainder of the patients’ lives regardless of treatment or disease activity Fetal and Neonatal Infections • Spirochetes readily cross the placenta causing congenital infection • Hepatomegaly, anemia, thrombocytopenia, ascites and hydrops • High serologic titers and unknown duration of infection are major predictors of congenital syphilis Treatment • Penicillin G is the treatment of choice for all stages of syphilis • No proven alternatives to penicillin therapy during pregnancy • Jarisch-Herxheimer reaction - acute febrile reaction frequently accompanied by headache, myalgia, and fetal heart deceleration - usually occur within the first 24 hours after treatment Management of Sex Partners • Persons exposed within 90 days before the diagnosis of primary, secondary or early latent syphilis must be treated presumptively • If exposed >90 days before the diagnosis, treat presumptively if the serologic test result is not immediately available and follow up is uncertain • Long term partners of patients with late latent syphilis should be evaluated clinically and serologically and treat on the basis of the findings Follow up • Patients should be reexamined clinically and serologically using non treponemal test titers 3,6,12, and 24 months after treatment • Failure of nontreponemal test titers to decline 4-fold within 6 months after treatment might be indicative of probable treatment failure • For retreatment, give Penicillin G x 3doses HIV Introduction Human Immunodeficiency Viruses • DNA retroviruses • HIV-1 and HIV-2 – most cases are caused by HIV-1 infection • mode of transmission – sexual intercourse: major mode of transmission – blood or blood-contaminated products – mothers may infect their fetuses Pathogenesis • thymus-derived lymphocytes, T lymphocytes, defined phenotypically by the CD4 surface antigen, are the principal target – CD4 site serves as a receptor for the virus • co-receptors are necessary for infection – chemokine receptors – CCR5 and CXCR4 Pathogenesis • after initial infection, the level of viremia usually decreases to a set point – patients with the highest viral burden at this time progress more rapidly to AIDS and death • over time, the number of T cells drop insidiously and progressively -- results in profound immunosuppression Clinical Manifestations • Incubation period: days to weeks • acute illness – similar to many viral syndromes – lasts less than 10 days – common symptoms: fever, night sweats, fatigue, rash, headache, lymphadenopathy, pharyngitis, myalgias, arthralgias, nausea, vomiting and diarrhea Clinical Manifestations AIDS • HIV-positive assay results associated with any number of clinical findings • CD4+ count of less than 200/mm3 • generalized lymphadenopathy, oral hairy leukoplakia, aphthous ulcers, and thrombocytopenia • neurologic disease is common Clinical Manifestations • opportunistic infections: – esophangeal or pulmonary candidiasis – persistent herpes simplex, zoster lesions – condyloma acuminata – tuberculosis – cytomegalovirus pneumonia, retinitis or gastrointestinal disease – molluscum contagiosum – Pneumocystis pneumonia – toxoplasmosis Serological Testing Standard Testing Protocol • Enzyme Immunoassay (EIA) – used as a screening test for HIV antibodies – repeatedly positive screening test has a sensitivity of more than 99.5% – positive test is confirmed with either Western blot or immunoflourescence assay (IFA) Maternal and Fetal-Neonatal Infection • mother-to-child transmission accounts for most pediatric HIV infections • pregnancy rates among women with HIV infection increased significantly in the current era Maternal and Fetal-Neonatal Infection • transmission rates 20% before 36 weeks 50% days before delivery 30% intrapartum 30-40% during breastfeeding Maternal and Fetal-Neonatal Infection • Vertical transmission is more common in preterm births, especially if with prolonged membrane rupture – 3.7 relative risk for intrapartum viral transmission Maternal and Fetal-Neonatal Infection • transmission at birth was increased from 15 to 25% in women whose membranes were ruptured for more than 4 hours • placental inflammation and chorioamnionitis may increase HIV 1 transmission by 3% Management during Pregnancy • counseling is mandatory – should be started early in pregnancy • antiviral therapy – therapeutic goal: maximal and enduring suppression of viral load and restoration and preservation of immunologic function – therapy should be offered to all HIVinfected pregnant women regardless of CD4+ T cell count or HIV RNA level Management during Pregnancy • antiviral therapy (generally) – Symptomatic • severe symptoms of HIV • AIDS – CD4 count 200cells/mm3 or less – Viral load 1,000 copies/ml or greater Management during Pregnancy Antiretroviral agents: 1. nucleoside reverse transcriptase inhibitors 2. non-nucleoside reverse transcriptase inhibitors 3. protease inhibitors 4. fusion inhibitors – block HIV-1 cell membrane binding and cell entry Management during Pregnancy • measurement of CD4+ T-cell count approximately every trimester, or about every 3-4 months • HIV RNA levels should be monitored 4 weeks after initiation of treatment, then monthly until undetectable, then every 3 months, and finally near term • monitor for antiretroviral toxicities during the initial 1-2 months of treatment – surveillance for hepatic toxicity and lactic acidosis Management during Pregnancy • treatment failures – nonadherence – inadequate drug potency – suboptimal levels of antiretrovirals – viral resistance Management during Pregnancy • additional medical care – hepatitis B, influenza, and pneumococcal vaccines are given after viral suppression – therapies for opportunistic infection and tuberculosis – if CD4+ T-cell count is below 200/mm3, primary prophylaxis for P. carinii pneumonia is recommended (sulfamethoxazole-trimethoprim, dapsone) Prevention of Vertical Transmission • 2 principal approaches: 1. antiretroviral therapy 2. cesarean delivery Prevention of Vertical Transmission TIME OF ADMINISTRATION Antepartum Intrapartum Neonate ZIDOVUDINE REGIMEN 100 mg orally five times daily, initiated at 14 to 34 weeks and continued throughout pregnancy intravenous zidovidine in a 1-hr initial dose of 2 mg/kg, followed by a continuous infusion of 1 mg/kg/hr until delivery give syrup at 2 mg/kg every 6 hours for 6 weeks, begin at 8 to 12 hours after birth Prevention of Vertical Transmission Cesarean Delivery • vertical transmission was reduced by one half when cesarean section was compared with vaginal delivery • when antiretroviral therapy was given along with cesarean delivery, the likelihood of transmission was reduced by 87% Prevention of Vertical Transmission Cesarean Delivery • scheduled cesarean delivery should be discussed and recommended for HIV-infected women whose HIV-1 RNA load exceeds 1000 copies/ml – recommended at 38 weeks Breastfeeding • not recommended • the probability of transmission per liter of breast milk ingested is estimated to be similar in magnitude to heterosexual transmission with unsafe sex in adults • risk is related to maternal HIV RNA level, HIV disease status, breast health, duration of breastfeeding • most transmission occur in the first 6 months Post partum • otherwise healthy women with normal CD4+ T cell counts and low HIV RNA levels may discontinue treatment after delivery • close monitoring • pyschologic support is important Postpartum • Contraception – All HIV infected individuals should be counseled to use condoms consistently – OCP – significantly interact with amprenavir/ fosamprenavir, efavirenz, lopinavir, nelfinavir, nevirapine, and ritonavir – IUD