* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Acute Disease Service: Hot Topics in Infectious - cmsa
Henipavirus wikipedia , lookup
West Nile fever wikipedia , lookup
Hepatitis C wikipedia , lookup
Meningococcal disease wikipedia , lookup
Chagas disease wikipedia , lookup
Oesophagostomum wikipedia , lookup
Swine influenza wikipedia , lookup
Schistosomiasis wikipedia , lookup
Influenza A virus wikipedia , lookup
Leptospirosis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
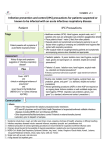
Acute Disease Service: Hot Topics in Infectious Diseases in Oklahoma Laurence Burnsed & Becky Coffman Oklahoma State Department of Health Acute Disease Service Communicable Disease Division 1000 Northeast Tenth Street Oklahoma City, OK 73117-1299 Acute Disease Service: Background • Mission – Prevention and control of communicable diseases via application of epidemiologic methods • Primary program activities – – – – – Epidemiologist-on-Call system (24/7/365) Surveillance and investigation of notifiable diseases Prevent transmission/secondary cases Outbreak response OK-HAN: Partner notification of urgent/important health events – Education of internal/external partners and public Acute Disease Service: Program Activities • Epidemiologist-on-Call – Available 24/7/365 for infectious disease consultation – Resource for questions/concerns posed for communicable disease issues (exception HIV/STDs) – Investigation of urgent events • Investigation, implementation of control measures – Determine exposed, susceptible contacts – Implement control measures (isolation, exclusion, active monitoring of contacts, prophylaxis) Why are some diseases reportable? • Uncommon but severe disease • Disease for which there is a public health intervention to prevent the spread of disease • Enhance ability to detect clusters or outbreak of a disease • New disease that we are trying to learn more about its epidemiology Example Disease Investigations • Measles – Cases suspected on clinical presentation immediately investigated – Laboratory testing coordinated to confirm – Identify susceptible contacts, implement control measures • Meningococcal Disease – Cases investigated immediately upon report – Identify exposed contacts, recommend postexposure prophylaxis External Partners Acute Disease Service works with external partners during disease investigations and provides disease consultation – – – – – – – Hospital personnel (Infection Preventionists) Laboratory personnel Healthcare Providers (physicians, nurses, PA’s, etc.) Veterinarians City officials School officials State and Federal Agencies • • • • • • Department of Environmental Quality Department of Agriculture Department of Education Food & Drug Administration US Department of Agriculture Centers for Disease Control and Prevention Novel Influenza Viruses • What makes an influenza strain novel? – It’s a different subtype from the currently circulating human influenza A H1 or H3 viruses – It’s an influenza A subtype that originated from a nonhuman species – It’s an influenza A subtype from a genetic reassortment between animal and human influenza viruses Influenza A H3N2v – 2010: First identified in U.S. pigs • The H3N2v virus had genes from pig, bird, and human influenza viruses and had the 2009 H1N1 pandemic virus M gene. – 2011 – 2013 human cases detected • 2011: 12 cases (IN, IA, ME, PA) • 2012: 309 cases in 12 states • 2013 to date: 17 cases (IN, IL, MI, OH) – No cases confirmed among OK residents to date! Summary of H3N2v Symptoms and Exposure Information • Symptoms are consistent with seasonal influenza: – Fever, cough, sore throat, myalgia, fatigue – CDC clinical guidance posted to the OSDH influenza A H3N2v web page: http://www.ok.gov/health/index.html – Antivirals recommended for high-risk groups – Susceptible to oseltamivir and zanamivir – Rapid antigen tests may not detect flu A H3N2v, negative does not exclude infection with this strain • Severity is also similar to other circulating flu strains – 16 (5%) of 335 cases hospitalized, 1 death – All had underlying medical conditions Influenza A H3N2v and Agricultural Fairs • Why is there concern with Ag venues? – Pigs from multiple places come in close contact with other pigs and people – Asymptomatic swine can shed the virus • Greater than 90% of cases have occurred in people who had close contact with pigs while exhibiting or helping to exhibit pigs at fairs – The majority of cases have occurred in persons ≤18 yrs of age Enhanced Public Health Surveillance for Influenza A H3N2v • OK-HAN distributed to: – Hospital IPs, labs, EDs, clinicians statewide • Enhanced surveillance activities: – Advise clinicians to consider H3N2v in patients with ILI who report direct contact with swine or attending a swine exhibit • Report suspected cases to ADS • Collect respiratory specimen for testing at OSDH PHL Influenza A H7N9 Background • April 2013: First reported in China – Avian influenza strain – Cases in 8 Chinese provinces, one case in Taipei with history of travel to affected Chinese province – Cases reported contact with poultry or live animal markets – Sharp decline in incidence after live animal market closures in affected provinces – No evidence of sustained person-to-person transmission – Note: No cases detected in US to date! Summary of H7N9 Clinical Information • Confirmed cases: present with severe respiratory illness: – High fever, non-productive cough, dyspnea, hypoxia, evidence of lower respiratory tract disease (infiltrates, opacities) – Complications: septic shock, respiratory failure, acute respiratory distress syndrome, acute renal dysfunction, encephalopathy • As of August 30: 135 human cases, 44 (33%) deaths Enhanced Public Health Surveillance for Influenza A H7N9 • OK-HAN distributed to: – Hospital IPs, labs, EDs, clinicians statewide • Enhanced surveillance activities: – Advise clinicians to consider H7N9 in patients with respiratory illness and appropriate travel or exposure history – Report suspected cases to ADS Epi-on-Call (24/7/365) – Collect respiratory specimen for testing at OSDH PHL • Focus testing on several respiratory illness cases requiring hospitalization Oklahoma Influenza and Respiratory Virus Sentinel Surveillance Program • Sentinel physicians and labs are located in each of the 8 regions of OK – Submit influenza-like illness & lab info weekly – Conducted year round • Influenza season occurs from the beginning of October to the end of April – The peak of influenza season occurs approximately at the beginning of February www.ok.gov/health/Disease,_Prevention,_Preparedness/Acut e_Disease_Service/Disease_Information/OK_Flu_View.html Respiratory Hygiene/Cough Etiquette Prevents spread of respiratory infections at the first point of contact in a healthcare setting Who: Any employee, patient or visitor in a healthcare facility with signs of a cold or respiratory infection How: – – – – Separate people with respiratory symptoms in waiting areas Ask symptomatic persons to wear a surgical mask Provide tissues and trash receptacles Perform hand hygiene after coughing, sneezing or touching respiratory secretions Signage/Education 2013-2014 Influenza Vaccine MERS CoV Background • Middle East Respiratory Syndrome Coronavirus – Viral respiratory disease first identified in Saudi Arabia during 2012 – Caused by a novel coronavirus • Distinct from coronavirus associated with SARS – Source not clearly understood yet. MERS CoV: Symptoms and Transmission • Symptoms and care – Fever, cough, shortness of breath – Most develop severe respiratory disease – Supportive care only • Transmission – Person-to-person, close contacts – Eight clusters identified in six countries among close, person contacts – One cluster involving healthcare personnel caring for a MERS CoV case MERS CoV Case Count • Case count as of September 5, 2013 – 108 cases, 50 (46%) deaths – 8 countries • All cases have a direct or indirect link to one of four countries: Saudi Arabia, Qatar, Jordan, United Arab Emirates – Onsets: April 2012 – May 2013 – Median age of cases is 56 years – No confirmed cases detected in the US MERS CoV Investigation • Similar to novel flu, investigations coordinated by OSDH ADS – Initial investigation: clinical history, exposures – Specimen collection by clinician or CHD for confirmation (via CDC) – Investigation of contacts, testing symptomatic – Implement disease prevention and control measures Healthcare-Associated Infections (HAIs) • Any condition caused by an infectious agent that – occurs in a patient in a hospital and – was not present (or incubating) when the patient was admitted to the hospital Financial Burdens of HAIs • Direct medical costs in the United States are estimated* to range** from: – Between $5.7 – $31.5 billion – Every year *Using Consumer Price Index (CPI) **Ranges of costs due to estimation Source: The Direct Medical Costs of Healthcare-Associated Infections in US Hospitals and the Benefits of Prevention. March 2009. www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf - Estimated Costs of Top Five HAIs: $9.8 Billion per Year Zimlichman, E., Henderson, D., Tamir, O., et. al. Health Care–Associated Infections: A Meta-analysis of Costs and Financial Impact on the US Health Care System. JAMA Intern Med. Published online September 02, 2013. http://archinte.jamanetwork.com/article.aspx?articleid=1733452 Social Burdens of HAIs • Direct Hospital Costs – Fixed costs: buildings, utilities, equipment, technology, labor – Variable costs: medications, food, consultations, treatments, procedures, devices, lab tests, radiographic tests, supplies • Indirect Costs – Lost wages, diminished productivity, short/long term morbidity, mortality, income lost by family members, forgone leisure time, time spent by family for hospital visits, travel costs • Intangible Costs – Psychological costs (anxiety, grief, disability), pain & suffering, change in social functioning Source: The Direct Medical Costs of Healthcare-Associated Infections in US Hospitals and the Benefits of Prevention. March 2009. www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf Prevention of HAIs • • • • • • Hand hygiene Use of personal protective equipment Removal of invasive lines ASAP Pre-op antibiotics: short-term Appropriate pre-op prep Cleaning and disinfection of equipment and environment • Timely reporting of organisms by lab CDC’s Isolation Precautions • Recommendations for acute care hospitals, home health care, ambulatory care, and long-term care settings • New topics: – – – – – Increase in MDRO’s Change in populations at risk New therapies and procedures Bioterrorism New pathogens www.cdc.gov/hicpac/2007IP/2007isolationPrecautions.html Two Categories of Precautions • Standard Precautions • Transmission Based Precautions – Empiric Precautions (proactive application of Transmission Based Precautions) Hand Hygiene • “The single most effective action to prevent spread of disease” • CDC recommends the use of alcohol-based handrubs by health care personnel Hand Hygiene Products • Soap and water – when hands are visibly soiled – when working with patients who have spore-forming organisms (such as C. difficile or B. anthracis) – after using the restroom or changing a diaper • Alcohol-based hand rubs – when hands are visibly clean – towelettes are not as effective so should not be used in healthcare settings www.who.int www.cdc.gov/injectionsafety/ Unsafe injection practices and circumstances that likely resulted in transmission of hepatitis C virus (HCV) at clinic A — Nevada, 2007 http://www.cdc.gov/mmwr/PDF/wk/mm5719.pdf Personal Protective Equipment (PPE) • • • • • Gloves Masks N-95 Respirators Gowns Eye protection Transmission-Based (Expanded) Precautions • Use in addition to standard precautions when pathogen is known or suspected • Based on routes of transmission: – Contact – Droplet – Airborne Infection Isolation (AII) Contact Transmission • Organisms spread by direct contact or contact with items in the patient's environment (indirect) • Examples: – Herpes simplex – Staph infections – Many gastroenteritis agents – MDRO’s such as MRSA Contact Isolation • • • • Private room Wear gloves when entering the room Wear a gown if soiling is likely Dedicate equipment to stay in the room until discharge when possible • Pay special attention to disinfection of contaminated surfaces Spencer, Maureen. Environmental Technology: Practical Implications , presented at APIC 2011, Baltimore MD Droplet Transmission • Organisms that are spread by large particle droplets > 5 • Examples: – Influenza – Bacterial meningitis – Whooping cough – Mumps – Pneumocystis carinii pneumonia Droplet Isolation • Private room – Or separate from others by at least 3 feet • Wear a standard surgical mask when entering the room • Patient follows Respiratory Hygiene/Cough Etiquette Airborne Transmission • Organisms transmitted by very small airborne droplet nuclei <5 • Examples: – Tuberculosis – Chickenpox – Measles – Smallpox Airborne Infection Isolation • Place patient into a negative airflow room • Don a fit-tested and fit-checked N-95 “mask” when entering the room – If the organism is known, susceptible people should not enter the room (measles, varicella) • Minimize patient movement • Place surgical mask on patient if necessary to leave the room Airborne Infection Isolation (AII) Rooms • Air is ventilated to outside, away from windows and doors • Continuous negative air pressure • Door of the room must be kept closed • Test airflow regularly (> daily when occupied) • Six air changes per hour (ACH) required for existing buildings, newly constructed rooms must be >12 ACH Empiric Precautions • Use precautions based on symptoms when diagnosis is still unknown: Symptom Diarrhea Precautions Contact Wound infections Rash Cavitary lung disease Contact Droplet/Airborne Airborne Respiratory infections Meningitis Droplet/Contact Droplet/Contact Antibiotic Resistance • MRSA (methicillin-resistant Staph aureus) – VISA and VRSA • VRE (vancomycin-resistant Enterococcus) • Acinetobacter baumanii • Drug-resistant Mycobacterium tuberculosis • Clostridium difficile (due to aby overuse) • Carbapenem-resistant Enterobacteriaceae www.cdc.gov/HAI/organisms/organisms.html Carbapenem-resistant Enterobacteriaceae (CRE) • CRE = carbapenem-resistant and carbapenemase-producing Enterobacteriaceae. • Klebsiella pneumoniae carbapenemase (KPC) is the most common type of carbapenemase in the US. • It is usually found in wounds or in the stool. • Effective antibiotics are limited. Triple-drug combinations are often used for bacteremia. Epidemiology of CRE • Enterobacteriaceae are normal flora of the respiratory and GI tract – Also nasopharynx, the respiratory tract, and the urinary tract • Transmission from person-to-person occurs through the hands of healthcare staff • Colonization rates vary – May persist up to several months • Some strains may be transmitted more easily • Environment thought to play a lesser role CRE: Who’s at risk? • • • • • • Patients with long hospitalizations Long-term acute care residents Immunocompromised patients Invasive tubes or devises Unhealed open wounds People can be “colonized”, meaning CRE is not causing illness, but can still be spread. Outbreaks of CRE • KPC outbreak at National Institutes of Health (NIH) for 6 months, starting in June 2011. – Total of 18 patients: transmission to 17 patients, 8 developed bloodstream infections (BSIs), and 6 attributable deaths. www.sciencetranslationalmedicine.org, 22 Aug. 2012, Vol 4., Issue 148 • KPC (CRKP) outbreak in an acute-care hospital in Denver, starting in May 2012. – Total of 8 patients: three were infected, five were colonized. No deaths. MMWR, Feb. 15, 2013, Vol. 62, No. 6, p 108 Outbreaks of CRE continued • KPC (CRKP) outbreak in an acute care hospital in West Virginia, from April 2009 – February 2011. – 40 total cases identified – Spread among 14 acute care hospitals, 2 LTACHs, and 10 nursing homes Clinical Infectious Diseases, Volume 53, Issue 6, p. 532-540 Summary of Prevention Strategies • Core measures: 1. Hand hygiene 2. Contact Precautions 3. Healthcare personnel education 4. Minimizing device use 5. Patient and staff cohorting 6. Lab notification 7. Promote antimicrobial stewardship 8. CRE screening • If transmission occurs in the facility: 1. Active surveillance 2. Chlorhexidine bathing www.cdc.gov/hai/organisms/cre/cre-toolkit/index.html When You Have a Patient With CRE • • • • Contact precautions Active surveillance may be performed Lab results will be verified with CDC Communicate with facilities when transferring patients • Use the transfer form on CDC website for all transfers: • www.cdc.gov/HAI/toolkits/InterfacilityTransfer CommunicationForm11-2010.pdf Use the transfer form on CDC website for all transfers: • www.cdc.gov/HAI/toolkits/InterfacilityTransferC ommunicationForm11-2010.pdf What the Health Department is Doing • Health Alert distributed to providers and IPs • Reporting is voluntary, and encouraged • Survey of hospitals performed: – Of 58 responses, 10 hospitals reported having at least one CRE in 2012 • Epidemiologists facilitate confirmatory testing • Consultation regarding control measures on a case-by-case basis “24/7” Acute Disease Service: 405-271-4060 Appropriate Antibiotic Use • Be Smart: Know When Antibiotics Work – Antibiotics don’t cure viral infections – Most respiratory infections are caused by viruses – Don’t pressure your healthcare provider for antibiotics – When you are prescribed antibiotics, take exactly as instructed www.cdc.gov/getsmart/ Fewer New Antibiotics • From 1983 to 2010, FDA approval of new antibiotics declined from four to less than one antibiotic per year – Less profitable in comparison with other drug classes for chronic or lifestyle conditions – FDA approval takes approximately 8 years, therefore there is little likelihood of a new antibiotic before 2015 Antibiotic Stewardship • Antibiotics are the only drug where use in one patient can affect the usefulness in another • As much as 50% of antibiotic use is unnecessary • Antibiotic stewardship programs limit inappropriate use of antibiotics and promote appropriate use • www.cdc.gov/getsmart/healthcare Environmental Cleaning • The inanimate environment plays a role in facilitating transmission of organisms. • Cleaning and disinfection reduces the numbers of microorganisms in the environment. • Cleaning not always seen as a high priority. • Germs can survive for days → weeks → months on surfaces. • Cleaning/disinfecting priorities might be upsidedown (high-touch vs. low-touch). Environmental Contamination X’s = culture- positive sites BBP Exposure in a Healthcare Setting in OK • In March 2013, OSDH and the Board of Dentistry inspected and found numerous deficiencies in a Tulsa oral surgeon’s office. • Patient with no other risk factors became HCV positive. • Issues included inappropriate use of multidose vials, misuse of the autoclave, and misguided corrosive cleaning of instruments. Next Steps • Press conferences held to inform the public. • Notification letters sent to 7000 patients. • HIV, hepatitis B and hepatitis C tests provided at OCCHD and TCCHD sites. Educational materials were provided . • To date, 4087 people were tested, and: – HCV positive = – HBV positive = – HIV positive = 82 5 4 In Progress • Patients with negative test results who had dental procedures in the 6 months before it closed, need to return for follow-up testing at least 6 months past the last dental clinic date. • Analysis of data obtained from chart reviews. • Identification of high-risk situations. • Linking likelihood of exposure via Dr. H’s office using genotyping. • Determining how many infected may have had different (non-dental) exposures. • In Summary: • Patients, visitors and employees all have a part in healthcare-associated infections • The environment can lays an important part in infection control and prevention • Use of antibiotics affects your community • Infections can be prevented through the use of – – – – Standard and transmission-based precautions Environmental cleaning Vaccination Communication Remember! • Protect yourself • Protect your patients • Protect your coworkers • Protect your family, friends and community Questions? Thank you! Call Acute Disease Service “24/7” 405-271-4060 http://ads.health.ok.gov Presenter Contact Information Laurence Burnsed MPH Administrative Program Manager [email protected] Becky Coffman MPH, RN, CIC Epidemiologist [email protected] Acute Disease Service 405-271-4060 The Far Side by Gary Larson